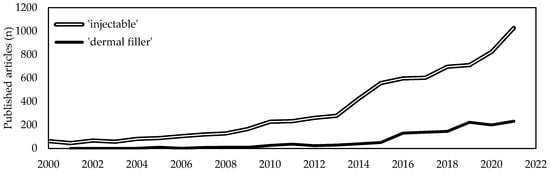
Soft tissues diseases significantly affect patients quality of life and usually require targeted, costly and sometimes constant interventions. With the average lifetime increase, a proportional increase of age-related soft tissues diseases has been witnessed. Due to this, the last two decades have seen a tremendous demand for minimally invasive one-step resolutive procedures. Intensive scientific and industrial research has led to the recognition of injectable formulations as a new advantageous approach in the management of complex diseases that are challenging to treat with conventional strategies. Among them, collagen-based products are revealed to be one of the most promising among bioactive biomaterials-based formulations. Collagen is the most abundant structural protein of vertebrate connective tissues and, because of its structural and non-structural role, is one of the most widely used multifunctional biomaterials in the health-related sectors, including medical care and cosmetics. Indeed, collagen-based formulations are historically considered as the “gold standard” and from 1981 have been paving the way for the development of a new generation of fillers. A huge number of collagen-based injectable products have been approved worldwide for clinical use and have routinely been introduced in many clinical settings for both aesthetic and regenerative surgery.
- collagen
- injectable collagen
- medical devices
1. Introduction
2. Collagen as Biomaterial
Collagen is the most abundant structural protein of vertebrate connective tissues, and accounts for about the 30% of the total body protein content [17][18][19][20][21][22][23][24][25][17,18,19,20,21,22,23,24,25]. The collagen family is a group of proteins that share a unique molecular fingerprint that is characterized by the presence of a right-handed triple-helical domain formed by three left-handed polyproline-II helices [26][34][35][26,34,35]. This superfamily accounts for 28 members, named from type I to XXVIII according to the discovery order [34][36][34,36]. Type I collagen was the first to be discovered and accounts for the 70% of the total collagen found in the human body [26]. This protein is a hetero trimer of about 400 kDa consisting of two identical α1 (≈139 kDa) chains and one α2 (≈129 kDa) chain of about 1000 amino acid residues [20][37][20,37]. Both chains are characterized by the repetition of the Glycine-X-Y triplet, where the X and Y positions are usually represented by proline and hydroxyproline, respectively [34][37][34,37]. Hydroxylation of proline residues is a typical modification of collagen and, because it accounts for about 11–14% of total residues, it is commonly used as a marker to detect and quantify collagen in tissues [35][38][35,38]. Another peculiarity of fibril-forming type I collagen molecules is their ability to spontaneously assemble to form fibrils in which molecules are quasi-hexagonally packed and super-twisted in a right-handed structure along the longitudinal axis of the fibril [39][40][41][39,40,41]. Thus, collagen molecules are aligned parallel to one another with a staggering of about 67 nm (D-banding) and can assemble into fibrils that can be greater than 500 µm in length and 500 nm in diameter [25][34][42][43][25,34,42,43]. Then, fibrils assemble in fibers whose 3D arrangement is tissue specific. Type I collagen not only covers a crucial structural role in tissue architecture maintenance but is actively involved in several biological and pathological processes [44]. The involvement of collagen in numerous cellular processes prompted research towards the use of collagen as biomaterial for the development of simplified ECM-like structures [20][35][20,35]. To this, several companies isolate medical-grade type I collagen from several sources and manufacture collagen-based implantable devices that are currently used in many clinical settings. Besides its advantages in term of biocompatibility for its physiological structural and non-structural functions, the use of collagen as biomaterial offers several advantages including low immunogenicity, tunable properties, and biodegradability. The low evolutionary gap and the high conservation of type I collagen amino acid composition among vertebrates make that homology up to 95% [19][45][46][47][48][19,45,46,47,48].3. Collagen-Based Injectable Formulations
More than 60 kinds of collagen-based fillers are available on the market, according to the end-use and they have routinely been introduced in many clinical settings (Table 12). The most common collagen extraction sources for the manufacture of collagen based injectable formulations are bovine, swine, porcine, equine and human derived, whose advantages and disadvantages are described in depth elsewhere [19][20][25][19,20,25]. Bovine collagen is one of the most commonly used fillers for effectively reducing wrinkles and other facial imperfections. More famous branded bovine-based collagen fillers are Zyderm®, Zyplast®, Contigen® (Allergan Inc., Dublin, Ireland), Artefill® (Suneva Medical, San Diego, CA, USA), and Artecoll® (Canderm Pharma Inc., Saint-Laurent, QB, Canada). Others include CHondroGrid® (Bioteck Spa, Arcugnano, Italy), Integra Flowable Wound Matrix® (Integra LifeScience Corp., Princeton, NJ, USA), Resoplast® (Rofil Medical International, Breda, The Netherlands), Atelocell® (KOKEN Co., Ltd., Bunkyo-ku, Tokyo, Japan). However, bovine collagen is known to be exposed to zoonosis (e.g., the foot and mouth disease and the group of the bovine spongiform encephalopathies, among which the most dangerous for humans is the transmissible spongiform encephalopathy) and to trigger allergies (about 2–4% of population) [49][50][51][71,72,73]. In addition to the strict regulation to which all implantable products are subjected, two consecutive negative patient skin tests at 6 and 2 weeks are required before use [51][52][73,74]. This sensitivity has been considered generally acceptable for implants for human use and actually bovine collagen is principally used for the treatment of the integumental [6][53][54][55][56][57][58][59][60][61][62][63][64][65][66][67][68][69][70][71][72][73][74][6,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96] (NCT01060943) and musculoskeletal apparatus [75][76][77][78][79][80][81][82][83][84][85][86][87][88][89][90][97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112] and to a minor extent for the gastrointestinal [91][92][93][94][95][96][97][98][113,114,115,116,117,118,119,120], urinary [99][100][101][102][103][104][65,121,122,123,124,125] and cardiovascular [105][106][107][126,127,128] systems. Recently, bovine collagen in fibrillar form has been employed as an organ protection system during thermal ablation of hepatic malignancies [108][129].
| Source | Manufacturer | Product | Additives | Applications | Ref. | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Equine | Euroresearch S.r.l. (Milan, Italy) | www.euroresearch.it | , accessed on 14 February 2023 | Nithya | – | Integumental | [109] | [163] | |||||||||
| Linerase | – | Integumental | [110][111][112][113][114] | [164,165,166,167,179] | |||||||||||||
| Nearmedic Italy S.r.l. (Como, Italy) | www.salvecoll.com | , accessed on 14 February 2023 | Salvecoll-E | – | Integumental | [115] | [60] | ||||||||||
| Bioteck Spa (Arcugnano, Italy) | www.bioteck.com | , accessed on 14 February 2023 | Biocollagen gel | Type III collagen, bone spongy powder | Musculoskeletal | – | |||||||||||
| Biocollagen crunch | Type III collagen, bone powder, bone spongy chips |
Musculoskeletal | – | ||||||||||||||
| ActivaBone CLX gel | Bone powder, exur, Vitamin C | Musculoskeletal | – | ||||||||||||||
| ActivaBone Injectable Paste |
Demineralized bone matrix, bone powder, exur, Vitamin C | Musculoskeletal | – | ||||||||||||||
| ActivaBone modulable paste |
Demineralized bone matrix, bone powder, bone cortical and spongy granules, exur, Vitamin C | Musculoskeletal | – | ||||||||||||||
| ActivaBone Crunch | Demineralized bone matrix, bone powder, cortical and spongy chips, exur, Vitamin C | Musculoskeletal | – | ||||||||||||||
| Bovine | Bioteck Spa (Arcugnano, Italy) | www.bioteck.com | , accessed on 14 February 2023 | CHondroGrid | – | Musculoskeletal | [90] | [112] | |||||||||
| Integra LifeScience Corp. (Princeton, NJ, USA) | www.integralife.com | , accessed on 14 February 2023 | Integra Flowable Wound Matrix | Glycosaminoglycans | Integumental | [66] | [88] | ||||||||||
| Helitene | – | Soft tissues | [108] | [129] | |||||||||||||
| Rofil Medical International (Breda, The Netherlands) | Resoplast | Lidocaine hydrochloride | Integumental | – | |||||||||||||
| Suneva Medical (San Diego, CA, USA) | www.sunevamedical.com | , accessed on 14 February 2023 | ArteFill | Polymethylmethacrylate, lidocaine | Integumental | [53][55][56][57][58][59][60][61][62][63] | [75,77,78,79,80,81,82,83,84,85] | ||||||||||
| Datascope Corp., (Montvale, NJ, USA) | VasoSeal | – | Cardiovascular | [107] | [128] | ||||||||||||
| BioMimetic Therapeutics, LLC (Franklin, TN, USA) | www.biomimetics.com | , accessed on 14 February 2023 | Augment | β-tricalcium phosphate, recombinant human platelet-derived growth factor-BB | Musculoskeletal | [75][77][78][79][80][81][82][83][84][85][86][87][88][89] | [97,99,100,101,102,103,104,105,106,107,108,109,110,111] | ||||||||||
| KOKEN Co., Ltd. (Bunkyo-ku, Tokyo, Japan) | www.kokenmpc.co.jp | , accessed on 14 February 2023 | Atelocell | Type III collagen | Integumental, gastrointestinal |
[64][65][91][92], NCT01060943 | [86,87,113,114], NCT01060943 | ||||||||||
| B. Braun (Crissier, Switzerland) | www.bbraun.com | , accessed on 14 February 2023 | Gelofusine | – | Cardiovascular | [105][106] | [126,127] | ||||||||||
| Allergan, Inc. (Dublin, Ireland) | www.abbvie.it | , accessed on 14 February 2023 | Zyplast | Glutaraldehyde | Integumental | [6][54][61][67][68][69][70][73][74][76][94]] | [6,76 | [ | ,83 | 95] | ,89 | [97] | ,90 | [ | ,91,92,95,96,98,116 | 116 | ,117,119,180] |
| Zyderm | – | Integumental | [6][61][67][98][116] | [6,83,89 | [68] | ,90 | [71] | ,93 | [72] | ,94 | [96] | ,118,120,180] | |||||
| Contigen | glutaraldehyde | Gastrointestinal and genitourinary | [93][100][101][102][103][104] | [115,121,122,123,124,125] | |||||||||||||
| Swine | GUNA (Milan, Italy) | www.guna.com | , accessed on 14 February 2023 | Dental Skin BioRegulation |
Vitamin C, magnesium gluconate, pyridozine chlorhydrate, riboflavin, thiamine chlorhydrate | Skin | [117] | [181] | |||||||||
| Dental ATM BioRegulation |
Hypericum | Musculoskeletal | [118] | [130] | |||||||||||||
| MD-HIP | Calcium phosphate | Musculoskeletal | [119] | [131] | |||||||||||||
| MD-ISCHIAL | Rhododendron | Musculoskeletal | [120] | [132] | |||||||||||||
| MD-KNEE | Arnica | Musculoskeletal | [121][122][123] | [133,143,144] | |||||||||||||
| MD-LUMBAR | Hamemelis | Musculoskeletal | [120][124][125] | [132,134,135] | |||||||||||||
| MD-NECK | Silicio | Musculoskeletal | – | ||||||||||||||
| MD-SHOULDERS | Iris | Musculoskeletal | [126][127] | [145,146] | |||||||||||||
| MD-SMALL JOINTS | Viola | Musculoskeletal | – | ||||||||||||||
| MD-THORACIC | Cimifuga | Musculoskeletal | – | ||||||||||||||
| MD-MATRIX | Citric acid, nicotinamide | Soft tissues | [125][128][129] | [135,136,160] | |||||||||||||
| MD-MUSCLE | Hypericum | Musculoskeletal | [118] | 130 | [120][121][124][125][127][ | ,132 | 128 | ,133 | ] | ,134 | [129 | ,135 | ][130] | [,136,137,146,160] | |||
| MD-POLY | Drosera | Musculoskeletal | – | ||||||||||||||
| MD-NEURAL | Citrullus | Musculoskeletal | [120][124][129] | [132,134,160] | |||||||||||||
| MD-TISSUE | Ascorbic acid, magnesium gluconate, pyridoxine chlorhydrate, riboflavin, thiamine chlorhydrate | Soft tissues | – | ||||||||||||||
| Joint Biomaterials S.r.l. (Mestre, Italy) | www.joint-biomateriali.it | , accessed on 14 February 2023 | CartiRegen | Fibrin glue | Musculoskeletal | – | |||||||||||
| Ubiosis (Gyeonggi-do, Republic of Korea) | www.ubiosis.com | , accessed on 14 February 2023 | COLTRIX CartiRegen | – | Musculoskeletal | – | |||||||||||
| COLTRIX TendoRegen | – | Musculoskeletal | – | ||||||||||||||
| Sewon Cellontech Co., Ltd. (Seoul, Republic of Korea) | www.swcell.com | , accessed on 14 February 2023 | CartiFill | Glucose, CaCl, amino acids, vitamin B, fibrin glue |
Musculoskeletal | [131][132], NCT02539030, NCT02519881 | [138,139], NCT02539030, NCT02519881 | ||||||||||
| CartiZol | Glucose, CaCl, amino acids, vitamin B | Musculoskeletal | [133], NCT02539095 | [140], NCT02539095 | |||||||||||||
| RegenSeal | – | Musculoskeletal | [134] | [141] | |||||||||||||
| TheraFill | – | Integumental | [64][65] | [86,87] | |||||||||||||
| Sunmax Biotechnology Co., Ltd. (Tainan, Taiwan) | www.sunmaxbiotech.com | , accessed on 14 February 2023 | Facial Gain | Lidocaine | Integumental | NCT03844529 | |||||||||||
| Collagen Implant I | – | Integumental | – | ||||||||||||||
| Evolence (Skillman, NJ, USA) |
Dermicol-P35 | Ribose | Integumental | [2] | 2 | [135] | ,147 | [136] | ,148 | [137], NCT00929071, NCT00891774 | [,149], NCT00929071, NCT00891774 | ||||||
| Mentor Corp. (Santa Barbara, CA, USA) |
Fibrel | – | Integumental | [138][139] | [150,151] | ||||||||||||
| Tissue Science Labs. (Aldershot, UK) |
Permacol | – | Gastrointestinal | [140][141][142][143][144][145][146] | [153,154,155,156,157,158,159] | ||||||||||||
| EternoGen, LLC (Columbia, MO, USA) |
RPC Pure Collagen | Ethylenediamine tetraacetic acid | Integumental | [147] | [67] | ||||||||||||
| Aspid S.A. de C.V. (Mexico City, Mexico) | www.aspidpharma.com | , accessed on 14 February 2023 | Fibroquel | Polyvinylpyrrolidone | Musculoskeletal | [148][149], NCT04517162 | [161,162], NCT04517162 | ||||||||||
| ColBar LifeScience Ltd. (Tel Aviv, Israel) | www.ortho-dermatologics.com | , accessed on 14 February 2023 | Evolence | Ribose | Integumental | [135][150] | [147,152] | ||||||||||
| Human | Fascia Biosystem (Beverly Hills, CA, USA) |
Fascian | Lidocain | Integumental | [6][151][152] | [6,168,171] | |||||||||||
| Fibrocell Science (Exton, PA, USA) | www.fibrocell.com | , accessed on 14 February 2023 | Isolagen therapy | – | Integumental | NCT00655356 | |||||||||||
| Inamed Corporation (Santa Barbara, CA, USA) | www.inamed-cro.com | , accessed on 14 February 2023 | Cosmoplast | Glutaraldehyde, lidocaine hydrochloride | Integumental | [6][153] | [6,169] | ||||||||||
| Cosmoderm | lidocaine hydrochloride | Integumental | [6][153] | [6,169] | |||||||||||||
| Life Cell Corp. (Branchburg, NJ, USA) |
Dermalogen | Type and VI collagen, elastin, fibronectin, chondroitin sulfate, and other proteoglycans | Integumental | [154] | [170] | ||||||||||||
| Cymetra | Elascin, glycosaminoglycans, Lidocaine hydrochloride | Integumental | [6][96][155][156][157][158] | [6,118,172,173,174,175] | |||||||||||||
| Collagenesis, Inc., (Beverly, MA, USA) |
Autologen | Elastin, fibronectin, glycosaminoglycans | Integumental | – | |||||||||||||
| Dermologen | - | Integumental | [156] | [173] | |||||||||||||
| Plant | Vesco Pharmaceutical Co. Ltd. (Bangkok, Thailand) | www.vescopharma.com | , accessed on 14 February 2023 | Collagen C 1000 | Vitamin C | Integumental | – | ||||||||||
| Silkworm | Monodermà (Milan, Italy) www.monoderma.com |
Fillagen | Hyaluronic acid, carboxymethylcellulose | Integumental | [159] | [178] | |||||||||||
| n. d. | Taumed (Rome, Italy) | www.taumed.it | , accessed on 14 February 2023 | Karisma | Hyaluronic acid, carboxymethylcellulose | Integumental | – | ||||||||||
| n. d. | LABO International S.r.l. (Padova, Italy) | www.labosuisse.com | , accessed on 14 February 2023 | Fillerina con 3D collagen |
Hyaluronic acid | Integumental | – | ||||||||||
| n. d. | Hebey Mepha Pharm Group Co., Ltd. (Shandong, Hebei, China) | www.mephacn.com | , accessed on 14 February 2023 | Collagen Plus | – | Integumental | – | ||||||||||
| n. d. | Pierre Mulot Laboratories (Paris, France) |
Neutroskin | Vitamin C | Integumental | – | ||||||||||||
| n. d. | Elements Pharmaceuticals (Shijiazhuang, Hebei, China) | www.elementspharma.com | , accessed on 14 February 2023 | Ele-collagen | Vitamin C, Vitamin B6 | Integumental | – | ||||||||||
| n. d. | Globus Medical (Audubon, PA, USA) | www.globusmedical.com | , accessed on 14 February 2023 | Kinex Bioactive gel | Bioglass, hyaluronic acid | Musculoskeletal | – |
4. Clinical Efficacy of Collagen-Based Injectable Implants
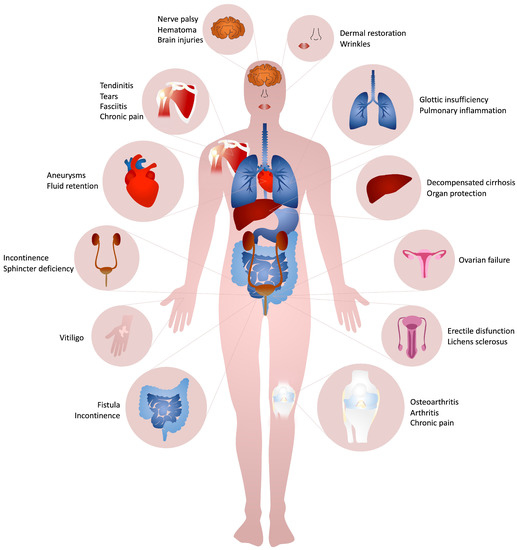
Collagen-based formulations are mainly used for the treatment of several kind of diseases belonging mainly to the musculoskeletal (i.e., hip or knee osteoarthritis [90][119][121][123][133][160][161][112,131,133,140,142,144,182], sprained knee pain [122][143], injured cartilage [131][134][138,141], piriformis syndrome [128][136], ankle and hindfoot arthritis [81][103] or fusion [78][84][85][86][87][100,106,107,108,109], lumbar spinal fusion [77][99], myofascial pain syndrome [118][130][130,137], chronic pain [120][132], acute lumbar spine pain [124][134], partial-thickness rotator cuff tears [127][134][162][141,146,183], plantar fasciitis [163][184], calcific supraspinatus tendinitis [126][145], pain [118][120][124][130][130,132,134,137]), urogenital (i.e., urinary incontinence [101][103][104][164][165][166][167][168][122,124,125,185,186,187,188,189], neurogenic urinary incontinence [169][190], lichens sclerosus [111][165], intrinsic sphincter deficiency [170][171][172][191,192,193], post-prostatectomy incontinence [99][102][173][174][175][176][65,123,194,195,196,197], retrograde ejaculation [177][198]), gastrointestinal (i.e., glottic insufficiency [91][92][94][96][97][156][178][179][180][181][182][113,114,116,118,119,173,199,200,201,202,203], rectal fistula [140][141][143][144][153,154,156,157], fecal incontinence [93][142][183][184][69,115,155,204]), and integumental (i.e., nasolabial folds [2][54][64][65][74][109][137][147][155][185][186][187][188][2,67,76,86,87,96,149,163,172,205,206,207,208], nasojugal folds [150][152], lip [2][55][73][136][153][155][2,77,95,148,169,172], cheek and temple area [155][172], glabellar groove [55][77], post-rhinoplasty dorsal irregularities [55][189][77,209], depressed acne scars [55][155][190][77,172,210] augmentation, post-burn hands malfunction [66][88] and vitiligo [110][164]) systems, as well as for non standard clinical applications (i.e., facial nerve rehabilitation after palsy [129][191][160,211], organ protection during thermal ablation [108][129], COVID-19 associated hyperinflammation [148][149][161,162] (NCT04517162), vitiligo [110][164], ovarian function after premature ovarian failure [192][212], the closure of artery aneurysms [107][193][128,213] and blood volume augmentation [106][194][127,214]) (Figure 2).