Parkinson’s disease 7 (PARK7/DJ-1) is a multifunctional protein whose protective role has been widely demonstrated in neurodegenerative diseases, including PD, AD, or ischemic stroke. Recent studies also revealed the importance of PARK7/DJ-1 in the maintenance of the gut microbiome and also in the regulation of intestinal inflammation. All these findings suggest that PARK7/DJ-1 may be a link and also a potential therapeutic target in gut and brain diseases.
- PARK7/DJ-1
- gut-brain axis
- inflammatory bowel diseases
- Crohn’s disease
- ulcerative colitis
- neurodegenerative disorders
- Parkinson’s disease
- Alzheimer’s disease
- blood-brain barrier
- oxidative stress
1. Introduction
2. Gut-Brain Axis
2.1. Epidemiological Evidence of a Gut-Brain Axis
IBD, including Crohn’s disease (CD) and ulcerative colitis (UC), affects more than 6.8 million people worldwide with a constantly growing prevalence [15][10]. It is well known that besides the gastrointestinal manifestations of IBD it can also affect the musculoskeletal system and the skin [16][11]. More recent epidemiological data also suggest a pathological crosstalk between intestinal inflammation and the development of neurodegenerative disorders, including PD and AD. Indeed, Lin et al. were the first who demonstrated the associations between the development of PD and IBD in a retrospective cohort study [17][12]. They found that IBD was associated with a 35% increased risk of PD. Within a few years, numerous independent large cohort studies confirmed their original observation. A Danish study demonstrated that IBD patients have a 22% increased risk of PD as compared with non-IBD individuals [18][13]. Similarly, a Swedish and an American study also found an increased PD hazard ratio in IBD patients compared to controls [19,20][14][15]. Also, the meta-analysis of Zhu et al. showed that CD and UC increase the risk of PD by nearly 30% compared to controls [21][16]. In accordance with the above studies, a South Korean cohort study showed that IBD patients were at a 1.87 times higher risk for PD than controls, respectively [22][17]. Similar to PD, epidemiological studies also revealed an increased risk of AD and dementia in patients with IBD. A meta-analysis by Fu et al. demonstrated that the risk of AD was increased by 52% in patients with gastrointestinal pathologies [23][18]. In addition, a recently published population-based cohort study demonstrated that the overall incidence of dementia among patients with IBD was significantly elevated (5.5% vs. 1.4% among controls) [24][19]. Although it is still not clear how intestinal diseases affect the development of CNS diseases, some previous epidemiological observations suggest that the systemic spreading of intestinal inflammation may be involved in the pathological crosstalk between the two organs. Indeed, a study of Peter et al. demonstrated that anti-tumor necrosis factor (TNF-α) therapy of the patient with IBD reduced the incidence of PD by 78%, as well [19][14]. Moreover, a South Korean study found that in IBD patients receiving anti-TNF therapy did not develop PD, and corticosteroid therapy also reduced the risk of PD by 92% among CD patients [22][17]. Moreover, a lower risk of PD was demonstrated in IBD patients treated with anti-inflammatory mesalazine or its derivative sulfasalazine [25][20]. Besides IBD, the role of CeD and gluten sensitivity has been suggested in the development of neurological and psychiatric disorders, including epilepsy, anxiety, depression, autism, and schizophrenia, as well [26][21]. Although the knowledge is sparse it is easy to accept that, similarly to IBD, the systemic spreading of inflammation may contribute to the development of CNS diseases. All of these epidemiological observations support the theory of the so-called "gut-brain axis”, in which the gastrointestinal alterations contribute to the development of CNS diseases, possibly through inflammatory mechanisms.2.2. Experimental Evidences of Gut Brain-Axis
Besides the epidemiological observations, numerous experimental studies, using animal models of UC and CD, have demonstrated that gastrointestinal inflammation may affect the brain. In these experimental models, the chemical agent 2,4,6- trinitrobenzene sulfonic acid (TNBS) or dextran sodium sulfate (DSS) were used to induce local, human IBD-like inflammation in the intestine of the mice [27,28][22][23]. These data demonstrated that intestinal inflammatory processes induce PD and AD-related pathological changes in the brain, including increased BBB permeability, neuro-inflammation, α-syn aggregation, and dopaminergic loss [29,30,31][24][25][26]. These experimental results are in accordance with the epidemiological observations suggesting that intestinal inflammation can induce PD and AD-associated pathological alterations in the CNS. The relevant experimental evidences demonstrating the GBA crosstalk were summarized in Table 1.|
Animal Model of IBD |
Effect on the CNS |
Refs. |
|---|---|---|
|
TNBS-induced colitis in rabbit |
Increased blood-brain barrier permeability |
|
|
TNBS-induced colitis in rat |
Elevated blood-brain barrier permeability and reduced endothelial barrier antigen expression |
|
|
Increased interleukin IL-6 expression in the hypothalamus and cerebral cortex |
||
|
DSS-induced colitis in mouse |
Elevated TNF-α, IL-1ß, and IL-6 expression in the substantia nigra |
|
|
Increased TNF-α and IL-6 expression in the cortex and decreased TJ protein occludin and claudin-5 in the brain |
||
|
Increased nigral level of IL-1ß and dopaminergic neuron death |
||
|
Increased COX-2 expression in the hippocampus and hypothalamus |
||
|
α-syn aggregation in the midbrain |
||
|
Microglial polarization into M1 and M2 phenotype in the medial prefrontal cortex |
||
|
Increased IL-1ß, IL-6, TNF-α and IL-10 expression in the hippocampus |
||
|
NLRP3 activation, amyloid plaque accumulation, and apoptosis in hippocampus, Cortex |
||
|
Elevated IL-1ß and TNF-α expression in the brain |
||
|
Increased microglia and astrocyte activation and loss of dopaminergic neurons in the substantia nigra pars compacta after PD inducing MPTP treatment |
||
|
Increased neurotoxic effect of MPTP treatment |
3. PARK7/DJ-1
4. Role of PARK7/dj-1 in the Pathogenesis of Neurodegenerative Diseases
The connection between PARK7/DJ-1 and neurodegenerative diseases was first suggested nearly two decades ago when it was identified as a causative factor in rare inherited forms of PD [7]. Since then, the role of PARK7/DJ-1 in neurodegenerative diseases has been intensively studied, and it has become clear that PARK7/DJ-1 may play a role not only in PD but in almost all neurological diseases associated with oxidative stress, inflammation, and tissue damage [9,126,127][9][53][54].4.1. Genetic Evidence for the Role of PARK7/DJ-1 in Parkinson’s Disease
The group of Parkinson’s disease molecules involves 23 genes located on different chromosomes and having different functions [128][55]. However, one thing that is common in the members of the PARK family is that they are all associated with the higher risk of PD [129][56]. This relationship was first suggested in 2003 when Bonifati and colleagues found a large (about 14 kb) deletion and a missense mutation (Leucine166Proline, L166P) in the PARK7/DJ-1 gene in a Dutch and an Italian family, leading to the identification of PARK7/DJ-1 as a causative gene for familial PD with recessive inheritance [7]. Since then, more than 20 PARK7/DJ-1 mutations have been associated with PD [130][57].4.2. Role of PARK7/DJ-1 in Parkinson’s Disease
Experimental data suggest that PARK7/DJ-1 plays a protective role in neurodegenerative diseases via its antioxidant properties. Indeed, the lack of PARK7/DJ-1 in stem cell-derived neurons and SH-SY5Y cells resulted in increased vulnerability to oxidative stress [131,132,133][58][59][60]. In addition, the neuroprotective effect of the administration of recombinant PARK7/DJ-1 was demonstrated in the rodent model of 6-hydroxydopamine (6-OHDA) and MG-132 treatment-induced PD [134][61]. Furthermore, it has been demonstrated that pharmacological protection of PARK7/DJ-1 against overoxidation preserves its antioxidant properties. Indeed, Miyazaki et al. and Kitamura et al. identified small molecule compounds, including UCP0054277, UCP0054278, and Compound 23 (Comp23), that can bind to the C106 region of PARK7/DJ-1 and keep it in reduced, biologically active form [8,135][8][62]. The protective effects of these compounds against oxidative stress were confirmed in hydrogen peroxide- (H2O2) treated wild type and PARK7/DJ-1-knockdown SH-SY5Y neuronal cells [8,135,136][8][62][63]. In further experiments, they also demonstrated that administration of UCP0054278 and or Comp23 suppressed the loss of dopaminergic neurons and motor dysfunction in an animal model of 6-OHDA or rotenone-induced PD [8,126][8][53]. Glyoxalase activity of PARK7/DJ-1 in neuroprotection may also be of great importance since AGEs have been suggested to contribute to the development of neurodegenerative diseases. Indeed, glycation-mediated AGE formation has been reported in the Lewy bodies in PD patients [137][64]. The relationship between AGEs and PD could be due to the ability of AGEs to cross-link α-syn, as has been shown using in vitro studies [138][65].4.3. Role of PARK7/DJ-1 in Alzheimer’s Disease
The role of PARK7/DJ-1 has also been suggested in AD. It was shown that the PARK7/DJ-1 binding compound UCP0054278 improved the AD-related cognitive deficits and prevented the degeneration of synaptic functions in AD modeling APdE9 transgenic mice [9]. Similarly, a recent study by Cheng et al. demonstrated that overexpression of DJ in the brain by lentiviral infection ameliorated β-amyloid protein (Aβ) deposition and the cognitive function of 5XFAD transgenic mice modeling AD [139][66]. The results also demonstrated that reactive oxygen species and oxidative stress marker malondialdehyde content were significantly decreased, while the antioxidant superoxide dismutase activity was significantly increased in the brain of 5XFAD mice overexpressing PARK7/DJ-1 [139][66]. In addition, AGEs are present in amyloid plaques in the brain of AD patients and have been suggested to promote the aggregation of Aβ and tau [140][67]. According to experimental data, the glyoxalase activity of PARK7/DJ-1 may reduce these deleterious effects of AGEs in neurons. Indeed, the protective role of PARK7/DJ-1 against dicarbonyl stress was demonstrated using mouse embryonic fibroblasts, human SH-SY5Y cells, and C. elegans, as well [114][68].4.4. Role of PARK7/DJ-1 in Huntington’s Disease
Huntington’s disease (HD) is an autosomal dominant inherited disease associated with polyglutamine expansion in the huntingtin (Htt) protein, leading to its misfolding and toxic aggregation [141][69]. A recent study by Sajjad et al. demonstrated that the level of oxidized PARK7/DJ-1 Cys106 level was elevated in the frontal cortex of HD patients [127][54]. They demonstrated that overexpression of PARK7/DJ-1 ameliorated mutant Htt toxicity in a yeast and Drosophila model of HD, suggesting the importance of the chaperoning activity of PARK7/DJ-1 in vivo. Their results also demonstrated that mild oxidation of PARK7/DJ-1 at cysteine 106 is required for its chaperone function; however, the complete oxidation of cysteine 106 leads to impaired PARK7/DJ-1 and detrimental cellular outcomes [127][54].4.5. Role of PARK7/DJ-1 in Ischemia-Reperfusion Induced Brain Injury
The importance of PARK7/DJ-1 has also been demonstrated in the ischemic-reperfusion injury of the brain. Indeed, intrastriatal injection of recombinant human PARK7/DJ-1 markedly reduced infarct size after middle cerebral artery occlusion of rats and protected SH-SY5Y against H2O2-induced apoptosis [133][60]. PARK7/DJ-1-deficient animals produced a significantly larger infarct size in the animal model of Endothelin-1 induced stroke compared to wild-type controls [142][70]. On the contrary, the administration of ND13 corresponding to the 13-N-terminal amino acids of PARK7/DJ-1 was shown to improve motor function after ischemic injury [143][71]. Similarly, PARK7/DJ-1 binding Comp23 reduced the infarct size of cerebral ischemia in rats [8,136,144][8][63][72].5. Role of PARK7/DJ-1 in the Pathogenesis of Gastrointestinal Diseases
In addition to the previously discussed effects of PARK7/DJ-1 in the pathomechanism of CNS diseases, its role in the disease of other organs including the heart [145[73][74][75],146,147], lung [148,149][76][77] and intestine [10,12,13,14,114,150,151,152][68][78][79][80][81][82][83][84] was recently studied.5.1. Genetic Evidence of the Role of PARK7/DJ-1 in Gastrointestinal Diseases
First, the genome-wide association (GWA) study of Dubois et al. involving 4533 coeliac disease cases and 10750 controls suggested that the genomic region of the short arm of chromosome 1 containing the PARK7/DJ-1 gene and also that of TNF Receptor Superfamily Member 9 (TNFRSF9) is strongly associated with the risk of coeliac disease [153][85]. A year later, in 2011, another GWA study comprising 6687 cases with ulcerative colitis (UC) and 19718 controls prepared by Anderson et al. revealed that the 1p36 chromosomal region, containing TNFRSF9, ERFF11, UTS2, and PARK7/DJ-1 genes, is associated with a higher risk of UC [150][82]. Not long after this, Lee et al. demonstrated that cDJR-1.1, the C. elegans homolog of the human PARK7/DJ-1 is expressed in the intestine of the worms. In addition, their results showed that lack of cDJR-1.1 makes the worms vulnerable to glyoxal-induced intestinal toxicity, giving the first in vivo evidence suggesting the protective role of PARK7/DJ-1 in intestinal pathology [114][68].5.2. Role of PARK7/DJ-1 in Coeliac Disease
The first direct human evidence suggesting the possible role of PARK7/DJ-1 in the pathomechanism of small intestinal diseases was the study of Vörös et al. [10][78]. In this study, the researchers' research group demonstrated the increased mRNA expression and protein level of PARK7/DJ-1 in the small intestinal mucosa of patients with untreated coeliac disease. In this study, the researchers found that PARK7/DJ-1 immunopositivity is present in the epithelial cells of the duodenal crypt, and also in the lamina propria of duodenal biopsies derived from therapy-naive children with celiac disease. Moreover, the researchers found that, following the introduction of a gluten-free diet, the amount of PARK7/DJ-1 normalizes, suggesting the possible role of PARK7/DJ-1 in the pathomechanism of celiac disease.5.3. Role of PARK7/DJ-1 in Inflammatory Bowel Disease
Despite the growing interest, there are relatively little data about the role of PARK7/DJ-1 in the pathomechanism of IBD. Recently, Di Narzo et al. investigated the plasma proteome of adult patients with Crohn’s disease (CD; n = 126) and ulcerative colitis (UC; n = 46) compared to that of healthy subjects (n = 72) using a high-throughput SOMAmer-based capture array [152][84]. They found that a total of 493 proteins showed altered levels in the plasma of patients with IBD compared to healthy subjects; among them, 219 were up- and 274 were down-regulated. One identified protein with an increased presence in the plasma of UC patients compared to that of healthy subjects was PARK7/DJ-1. The role of PARK7/DJ-1 in coeliac disease and IBD-related intestinal inflammation is demonstrated, however, further studies are needed to resolve the contradictions and elucidate the precise role of PARK7/DJ-1 in IBD.5.4. The Role of PARK7/DJ-1 in Intestinal Dysbiosis
A recent publication of Singh et al. investigated the effect of PARK7/DJ-1 deficiency on the intestinal microbiome of healthy mice [14][81]. They investigated the effect of PARK7/DJ-1 deletion on bacterial composition of the intestine by 16S rRNA sequencing. Analysis of fecal samples showed that overall composition of the microbiome did not differ between PARK7/DJ-1−/− and PARK7/DJ-1+/+ and mice at the phylum level. However, calculation of the F/B ratio showed that it decreased significantly in PARK7/DJ-1−/− mice compared to PARK7/DJ-1+/+ mice, suggesting the functional role of PARK7/DJ-1 on the composition of the intestinal microbiome. The deeper analysis of the data showed an increased presence of Alistipes and Rikenella species in PARK7/DJ-1−/− mice. The role of these species has been described regarding the pathomechanism of IBD [159][86]. Changes in the composition of intestinal microbiome affect its metabolite production. Accordingly, they demonstrated that the amount of fecal and also that of serum amino acids, including valine, leucine, phenylalanine, alanine, tyrosine and isoleucine, were downregulated, whereas SCFAs, including malonate, dimethylamine, trimethylamine and acetoin, were upregulated in PARK7/DJ-1−/− mice compared to that of PARK7/DJ-1+/+ mice. Although the metabolic changes of PARK7/DJ-1−/− mice were complex, Singh et al. suggested that it can lead to metabolic stress of the intestine, as demonstrated by the increased inflammation of the intestine. Indeed, they found increased levels of pro-inflammatory monocyte chemotactic protein-1 (MCP-1) and calprotectin in feces of PARK7/DJ-1−/− mice compared to that of PARK7/DJ-1+/+ mice. However, it must be also noted that the expression of other pro-inflammatories such as granulocyte monocyte colony stimulating factor IFN-β decreased, and that of many others, including IL-12p70, TNF-α, IL-17A, IFN-γ, IL-23 and IL-6 did not change. Finally, since the association of the intestinal microbiome and also that of PARK7/DJ-1 with neurodegenerative diseases is well known, they investigated the molecular biological changes in the midbrain of PARK7/DJ-1−/− mice by RNA-sequencing. They found the upregulation of PD related inflammatory genes, including polymerase family member 1 (Parp1) and MMP-8 in the midbrain of PARK7/DJ-1−/− mice compared to that of PARK7/DJ-1+/+ mice, suggesting that changes in the intestinal microbiome and/or lack of PARK7/DJ-1 may alter the pathology of the CNS.6. Role of PARK7/DJ-1 in GBA Diseases
Based on the current knowledge, it is assumed that PARK7/DJ-1 represents a molecular link between intestinal and brain diseases. Indeed, recent studies demonstrated that PARK7/DJ-1, through its antioxidant and anti-inflammatory properties, plays a role in the maintenance of healthy intestinal microbiome and mucosal integrity, thus influencing the local and systemic inflammation characteristic for IBD. As intestine-derived inflammatory factors can reach the BBB and impair its integrity, the inflammation can also spread also to the brain. The increased presence of inflammatory mediators induces the inflammation of CNS and may also alter the synthesis and function of PARK7/DJ-1 itself in the brain (Figure 1). Indeed, it has been shown that TNF-α, TGF-β, or LPS reduces the expression of PARK7/DJ-1, and also that increased amounts of MMP-3 may induce its degradation (Table 2). Also, the oxidative stress is an important factor that regulates the synthesis and function of PARK7/DJ-1 in the brain. Moreover, oxidative stress has been demonstrated to play a key role in the inactivation and degradation of PARK7/DJ-1 (Table 2).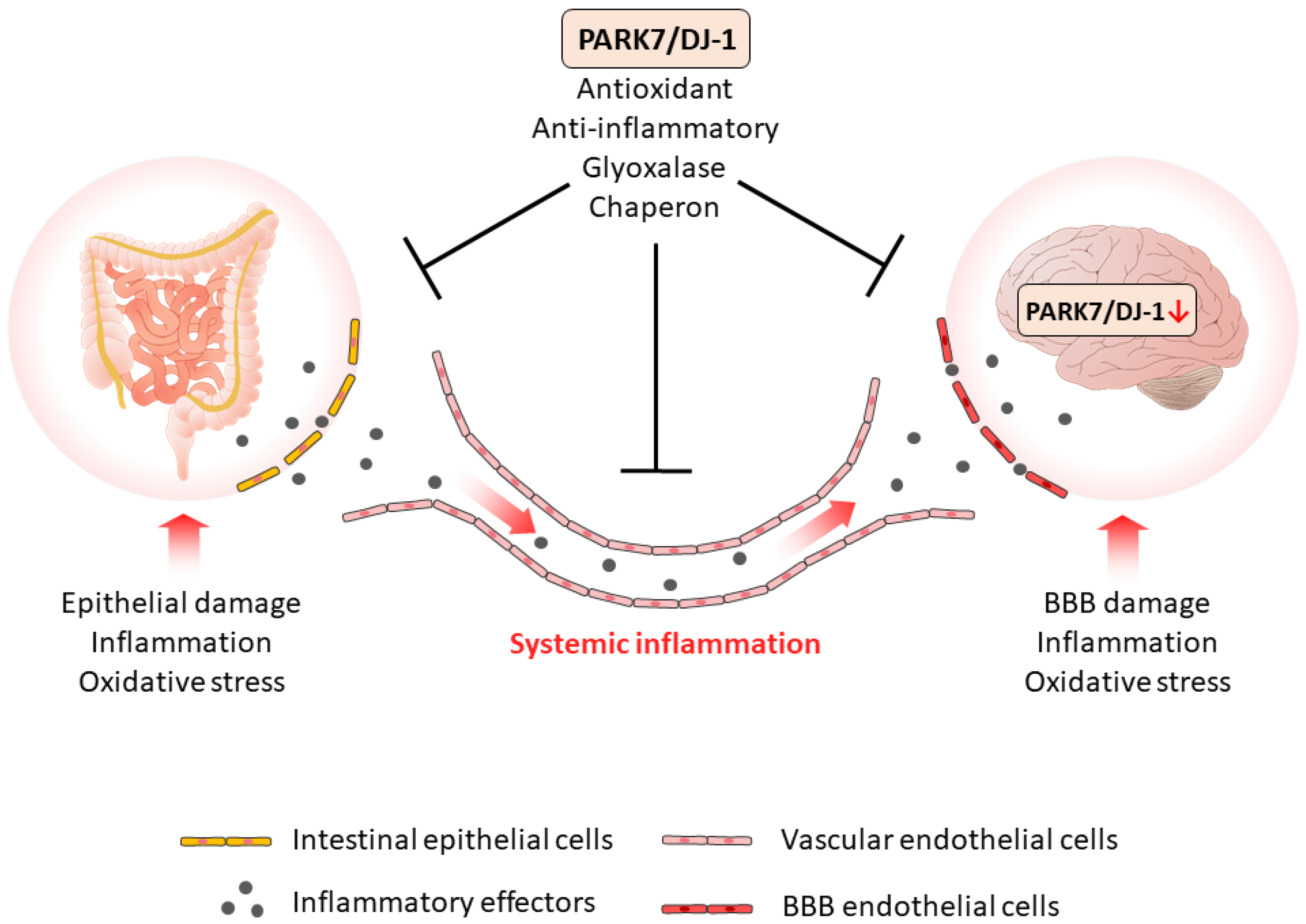
|
Molecule |
Effect on PARK7/DJ-1 |
Tissue or Cell Type |
Refs. |
|---|---|---|---|
|
Negative regulators of PARK7/DJ1 |
|||
|
H2O2 |
Overoxidation |
Human brain |
|
|
p53 |
Reduced expression |
mouse embryonic fibroblasts |
|
|
BAG5 |
Decreased stability |
HEK293 human embryonic kidney |
|
|
MMP-3 |
Proteomic fragmentation |
CATH.a mouse neuronal |
|
|
LPS |
Reduced expression |
HT-29 human colonic adenocarcinoma |
|
|
TNF-α |
Reduced expression |
HT-29 human colonic adenocarcinoma |
|
|
TGF-β |
Reduced expression |
HT-29 human colonic adenocarcinoma |
|
|
miR-128-3p |
Reduced expression |
Human hepatocellular carcinoma |
|
|
miR-494 |
Reduced expression |
3T3-L1 mouse adipocytes and Neuro-2a neuroblastoma |
|
|
miR-203 |
Reduced expression |
SW1990/DDP human pancreatic cancer cells |
|
|
Positive regulators of PARK7/DJ1 |
|||
|
STAT5A |
Increased expression |
human leukemic pre-B |
|
|
SG2NA |
Protection from degradation |
Neuro2a neuroblastoma |
|
|
IL-17 |
Increased expression |
HT-29 human colonic adenocarcinoma |
|
|
H2O2 |
Increased expression |
HT-29 human colonic adenocarcinoma |
|
References
- Brudek, T. Inflammatory Bowel Diseases and Parkinson’s Disease. J. Parkinson’s Dis. 2019, 9, S331–S344.
- Houser, M.C.; Tansey, M.G. The gut-brain axis: Is intestinal inflammation a silent driver of Parkinson’s disease pathogenesis? NPJ Parkinson’s Dis. 2017, 3, 3.
- Zhang, Y.-Z.; Li, Y.-Y. Inflammatory bowel disease: Pathogenesis. World J. Gastroenterol. 2014, 20, 91–99.
- Galea, I. The blood–brain barrier in systemic infection and inflammation. Cell. Mol. Immunol. 2021, 18, 2489–2501.
- Holmqvist, S.; Chutna, O.; Bousset, L.; Aldrin-Kirk, P.; Li, W.; Björklund, T.; Wang, Z.-Y.; Roybon, L.; Melki, R.; Li, J.-Y. Direct evidence of Parkinson pathology spread from the gastrointestinal tract to the brain in rats. Acta Neuropathol. 2014, 128, 805–820.
- Huang, M.; Chen, S. DJ-1 in neurodegenerative diseases: Pathogenesis and clinical application. Prog. Neurobiol. 2021, 204, 102114.
- Bonifati, V.; Rizzu, P.; Van Baren, M.J.; Schaap, O.; Breedveld, G.J.; Krieger, E.; Dekker, M.C.; Squitieri, F.; Ibanez, P.; Joosse, M.; et al. Mutations in the DJ-1 gene associated with autosomal recessive early-onset parkinsonism. Science 2003, 299, 256–259.
- Kitamura, Y.; Watanabe, S.; Taguchi, M.; Takagi, K.; Kawata, T.; Takahashi-Niki, K.; Yasui, H.; Maita, H.; Iguchi-Ariga, S.M.; Ariga, H. Neuroprotective effect of a new DJ-1-binding compound against neurodegeneration in Parkinson’s disease and stroke model rats. Mol. Neurodegener. 2011, 6, 48.
- Kitamura, Y.; Inden, M.; Kimoto, Y.; Takata, K.; Yanagisawa, D.; Hijioka, M.; Ashihara, E.; Tooyama, I.; Shimohama, S.; Ariga, H. Effects of a DJ-1-Binding Compound on Spatial Learning and Memory Impairment in a Mouse Model of Alzheimer’s Disease. J. Alzheimer’s Dis. 2017, 55, 67–72.
- Alatab, S.; Sepanlou, S.G.; Ikuta, K.; Vahedi, H.; Bisignano, C.; Safiri, S.; Sadeghi, A.; Nixon, M.R.; Abdoli, A.; Abolhassani, H.; et al. The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 2020, 5, 17–30.
- Levine, J.S.; Burakoff, R. Extraintestinal manifestations of inflammatory bowel disease. Gastroenterol. Hepatol. 2011, 7, 235.
- Lin, J.-C.; Lin, C.-S.; Hsu, C.-W.; Lin, C.-L.; Kao, C.-H. Association Between Parkinson’s Disease and Inflammatory Bowel Disease: A Nationwide Taiwanese Retrospective Cohort Study. Inflamm. Bowel Dis. 2016, 22, 1049–1055.
- Villumsen, M.; Aznar, S.; Pakkenberg, B.; Jess, T.; Brudek, T.A.-O. Inflammatory bowel disease increases the risk of Parkinson’s disease: A Danish nationwide cohort study 1977–2014. Gut 2018, 68, 18–24.
- Peter, I.; Dubinsky, M.; Bressman, S.; Park, A.; Lu, C.; Chen, N.; Wang, A. Anti-Tumor Necrosis Factor Therapy and Incidence of Parkinson Disease Among Patients with Inflammatory Bowel Disease. JAMA Neurol. 2018, 75, 939–946.
- Weimers, P.; Halfvarson, J.; Sachs, M.C.; Saunders-Pullman, R.; Ludvigsson, J.F.; Peter, I.; Burisch, J.; Olén, O. Inflammatory Bowel Disease and Parkinson’s Disease: A Nationwide Swedish Cohort Study. Inflamm. Bowel Dis. 2019, 25, 111–123.
- Zhu, F.; Li, C.; Gong, J.; Zhu, W.; Gu, L.; Li, N. The risk of Parkinson’s disease in inflammatory bowel disease: A systematic review and meta-analysis. Dig. Liver Dis. 2019, 51, 38–42.
- Park, S.A.-O.; Kim, J.; Chun, J.A.-O.; Han, K.; Soh, H.A.-O.; Kang, E.A.; Lee, H.J.; Im, J.A.-O.; Kim, J.S. Patients with Inflammatory Bowel Disease Are at an Increased Risk of Parkinson’s Disease: A South Korean Nationwide Population-Based Study. J. Clin. Med. 2019, 8, 1191.
- Fu, P.A.-O.; Gao, M.A.-O.; Yung, K.A.-O. Association of Intestinal Disorders with Parkinson’s Disease and Alzheimer’s Disease: A Systematic Review and Meta-Analysis. ACS Chem. Neurosci. 2019, 11, 395–405.
- Zhang, B.A.-O.; Wang, H.A.-O.; Bai, Y.M.; Tsai, S.J.; Su, T.P.; Chen, T.J.; Wang, Y.A.-O.; Chen, M.A.-O. Inflammatory bowel disease is associated with higher dementia risk: A nationwide longitudinal study. Gut 2021, 70, 85–91.
- Ríos, J.P.; Navarro, C.J.M.; Navarro, M.J.P.; Tapia, M.J.C.; Vera, M.J.P.; Arillo, V.C.; García, M.R.G.; Castellanos, A.M.; Sevilla, F.E. Association of Parkinson’s disease and treatment with aminosalicylates in inflammatory bowel disease: A cross-sectional study in a Spain drug dispensation records. BMJ Open 2019, 9, e025574.
- Lerner, A.A.-O.; Benzvi, C. “Let Food Be Thy Medicine”: Gluten and Potential Role in Neurodegeneration. Cells 2021, 10, 756.
- Antoniou, E.; Margonis, G.A.; Angelou, A.; Pikouli, A.; Argiri, P.; Karavokyros, I.; Papalois, A.; Pikoulis, E. The TNBS-induced colitis animal model: An overview. Ann. Med. Surg. 2016, 11, 9–15.
- Chassaing, B.; Aitken, J.D.; Malleshappa, M.; Vijay-Kumar, M. Dextran sulfate sodium (DSS)-induced colitis in mice. Curr. Protoc. Immunol. 2014, 104, 15–25.
- Sweeney, M.D.; Sagare, A.P.; Zlokovic, B.V. Blood–brain barrier breakdown in Alzheimer disease and other neurodegenerative disorders. Nat. Rev. Neurol. 2018, 14, 133–150.
- Heneka, M.T.; Carson, M.J.; El Khoury, J.; Landreth, G.E.; Brosseron, F.; Feinstein, D.L.; Jacobs, A.H.; Wyss-Coray, T.; Vitorica, J.; Ransohoff, R.M. Neuroinflammation in Alzheimer’s disease. Lancet Neurol. 2015, 14, 388–405.
- Kouli, A.; Torsney, K.M.; Kuan, W.-L. Parkinson’s disease: Etiology, neuropathology, and pathogenesis. In Parkinson’s Disease: Pathogenesis and Clinical Aspects; Codon Publications: Singapore, 2018.
- Hathaway, C.A.; Appleyard, C.B.; Percy, W.H.; Williams, J.L. Experimental colitis increases blood-brain barrier permeability in rabbits. Am. J. Physiol.-Gastrointest. Liver Physiol. 1999, 276, G1174–G1180.
- Natah, S.S.; Mouihate, A.; Pittman, Q.J.; Sharkey, K.A. Disruption of the blood-brain barrier during TNBS colitis. Neurogastroenterol. Motil. 2005, 17, 433–446.
- Wang, K.; Yuan, C.-P.; Wang, W.; Yang, Z.-Q.; Cui, W.; Mu, L.-Z.; Yue, Z.-P.; Yin, X.-L.; Hu, Z.-M.; Liu, J.-X. Expression of interleukin 6 in brain and colon of rats with TNBS-induced colitis. World J. Gastroenterol. 2010, 16, 2252–2259.
- Villarán, R.F.; Espinosa-Oliva, A.M.; Sarmiento, M.; De Pablos, R.M.; Argüelles, S.; Delgado-Cortés, M.J.; Sobrino, V.; Van Rooijen, N.; Venero, J.L.; Herrera, A.J. Ulcerative colitis exacerbates lipopolysaccharide-induced damage to the nigral dopaminergic system: Potential risk factor in Parkinsons disease. J. Neurochem. 2010, 114, 1687–1700.
- Han, Y.; Zhao, T.; Cheng, X.; Zhao, M.; Gong, S.-H.; Zhao, Y.-Q.; Wu, H.-T.; Fan, M.; Zhu, L.-L. Cortical Inflammation is Increased in a DSS-Induced Colitis Mouse Model. Neurosci. Bull. 2018, 34, 1058–1066.
- Garrido-Gil, P.; Rodriguez-Perez, A.I.; Dominguez-Meijide, A.; Guerra, M.J.; Labandeira-Garcia, J.L. Bidirectional Neural Interaction Between Central Dopaminergic and Gut Lesions in Parkinson’s Disease Models. Mol. Neurobiol. 2018, 55, 7297–7316.
- Do, J.; Woo, J. From Gut to Brain: Alteration in Inflammation Markers in the Brain of Dextran Sodium Sulfate-induced Colitis Model Mice. Clin. Psychopharmacol. Neurosci. 2018, 16, 422.
- Grathwohl, S.; Quansah, E.; Maroof, N.; Steiner, J.A.; Spycher, L.; Benmansour, F.; Duran-Pacheco, G.; Siebourg-Polster, J.; Oroszlan-Szovik, K.; Remy, H.; et al. Experimental colitis drives enteric alpha-synuclein accumulation and Parkinson-like brain pathology. bioRxiv 2018, 505164.
- Sroor, H.M.; Hassan, A.M.; Zenz, G.; Valadez-Cosmes, P.; Farzi, A.; Holzer, P.; El-Sharif, A.; Gomaa, F.A.-Z.M.; Kargl, J.; Reichmann, F. Experimental colitis reduces microglial cell activation in the mouse brain without affecting microglial cell numbers. Sci. Rep. 2019, 9, 20217.
- Gampierakis, I.-A.; Koutmani, Y.; Semitekolou, M.; Morianos, I.; Polissidis, A.; Katsouda, A.; Charalampopoulos, I.; Xanthou, G.; Gravanis, A.; Karalis, K.P. Hippocampal neural stem cells and microglia response to experimental inflammatory bowel disease (IBD). Mol. Psychiatry 2021, 26, 1248–1263.
- He, X.F.; Li, L.L.; Xian, W.B.; Li, M.Y.; Zhang, L.Y.; Xu, J.H.; Pei, Z.; Zheng, H.Q.; Hu, X.Q. Chronic colitis exacerbates NLRP3-dependent neuroinflammation and cognitive impairment in middle-aged brain. J. Neuroinflamm. 2021, 18, 153.
- Talley, S.; Valiauga, R.; Anderson, L.; Cannon, A.R.; Choudhry, M.A.; Campbell, E.M. DSS-induced inflammation in the colon drives a proinflammatory signature in the brain that is ameliorated by prophylactic treatment with the S100A9 inhibitor paquinimod. J. Neuroinflamm. 2021, 18, 263.
- Gil-Martínez, A.-L.; Estrada, C.; Cuenca, L.; Cano, J.-A.; Valiente, M.; Martínez-Cáceres, C.-M.; Fernández-Villalba, E.; Herrero, M.-T. Local Gastrointestinal Injury Exacerbates Inflammation and Dopaminergic Cell Death in Parkinsonian Mice. Neurotox. Res. 2019, 35, 918–930.
- Houser, M.C.; Caudle, W.M.; Chang, J.; Kannarkat, G.T.; Yang, Y.; Kelly, S.D.; Oliver, D.; Joers, V.; Shannon, K.M.; Keshavarzian, A.; et al. Experimental colitis promotes sustained, sex-dependent, T-cell-associated neuroinflammation and parkinsonian neuropathology. Acta Neuropathol. Commun. 2021, 9, 139.
- Ito, G.; Ariga, H.; Nakagawa, Y.; Iwatsubo, T. Roles of distinct cysteine residues in S-nitrosylation and dimerization of DJ-1. Biochem. Biophys. Res. Commun. 2006, 339, 667–672.
- Kiss, R.; Zhu, M.; Jójárt, B.; Czajlik, A.; Solti, K.; Fórizs, B.; Nagy, É.; Zsila, F.; Beke-Somfai, T.; Tóth, G. Structural features of human DJ-1 in distinct Cys106 oxidative states and their relevance to its loss of function in disease. Biochim. Biophys. Acta (BBA)-Gen. Subj. 2017, 1861, 2619–2629.
- Wilson, M.A. The role of cysteine oxidation in DJ-1 function and dysfunction. Antioxid. Redox Signal. 2011, 15, 111–122.
- Takahashi-Niki, K.; Inafune, A.; Michitani, N.; Hatakeyama, Y.; Suzuki, K.; Sasaki, M.; Kitamura, Y.; Niki, T.; Iguchi-Ariga, S.M.M.; Ariga, H. DJ-1-dependent protective activity of DJ-1-binding compound no. 23 against neuronal cell death in MPTP-treated mouse model of Parkinson’s disease. J. Pharmacol. Sci. 2015, 127, 305–310.
- Zhang, L.; Wang, J.; Wang, J.; Yang, B.; He, Q.; Weng, Q. Role of DJ-1 in Immune and Inflammatory Diseases. Front. Immunol. 2020, 11, 994.
- Canet-Avilés, R.M.; Wilson, M.A.; Miller, D.W.; Ahmad, R.; McLendon, C.; Bandyopadhyay, S.; Baptista, M.J.; Ringe, D.; Petsko, G.A.; Cookson, M.R. The Parkinson’s disease protein DJ-1 is neuroprotective due to cysteine-sulfinic acid-driven mitochondrial localization. Proc. Natl. Acad. Sci. USA 2004, 101, 9103–9108.
- Nagakubo, D.; Taira, T.; Kitaura, H.; Ikeda, M.; Tamai, K.; Iguchi-Ariga, S.M.M.; Ariga, H. DJ-1, a Novel Oncogene Which Transforms Mouse NIH3T3 Cells in Cooperation withras. Biochem. Biophys. Res. Commun. 1997, 231, 509–513.
- Maita, C.; Tsuji, S.; Yabe, I.; Hamada, S.; Ogata, A.; Maita, H.; Iguchi-Ariga, S.M.M.; Sasaki, H.; Ariga, H. Secretion of DJ-1 into the serum of patients with Parkinson’s disease. Neurosci. Lett. 2008, 431, 86–89.
- Jin, W. Novel Insights into PARK7 (DJ-1), a Potential Anti-Cancer Therapeutic Target, and Implications for Cancer Progression. J. Clin. Med. 2020, 9, 1256.
- He, X.Y.; Liu, B.Y.; Yao, W.Y.; Zhao, X.J.; Zheng, Z.; Li, J.F.; Yu, B.Q.; Yuan, Y.Z. Serum DJ-1 as a diagnostic marker and prognostic factor for pancreatic cancer. J. Dig. Dis. 2011, 12, 131–137.
- Zhou, J.; Liu, H.; Zhang, L.; Liu, X.; Zhang, C.; Wang, Y.; He, Q.; Zhang, Y.; Li, Y.; Chen, Q.; et al. DJ-1 promotes colorectal cancer progression through activating PLAGL2/Wnt/BMP4 axis. Cell Death Dis. 2018, 9, 865.
- Antipova, D.; Bandopadhyay, R. Expression of DJ-1 in Neurodegenerative Disorders. In DJ-1/PARK7 Protein; Ariga, H., Iguchi-Ariga, S., Eds.; Springer: Berlin/Heidelberg, Germany, 2017.
- Inden, M.; Kitamura, Y.; Takahashi, K.; Takata, K.; Ito, N.; Niwa, R.; Funayama, R.; Nishimura, K.; Taniguchi, T.; Honda, T.; et al. Protection Against Dopaminergic Neurodegeneration in Parkinson’s Disease–Model Animals by a Modulator of the Oxidized Form of DJ-1, a Wild-type of Familial Parkinson’s Disease–Linked PARK7. J. Pharmacol. Sci. 2011, 117, 189–203.
- Sajjad, M.U.; Green, E.W.; Miller-Fleming, L.; Hands, S.; Herrera, F.; Campesan, S.; Khoshnan, A.; Outeiro, T.F.; Giorgini, F.; Wyttenbach, A. DJ-1 modulates aggregation and pathogenesis in models of Huntington’s disease. Hum. Mol. Genet. 2014, 23, 755–766.
- Marras, C.; Lang, A.; van de Warrenburg, B.P.; Sue, C.M.; Tabrizi, S.J.; Bertram, L.; Mercimek-Mahmutoglu, S.; Ebrahimi-Fakhari, D.; Warner, T.T.; Durr, A.; et al. Nomenclature of genetic movement disorders: Recommendations of the international Parkinson and movement disorder society task force. Mov. Disord. 2016, 31, 436–457.
- Li, W.; Fu, Y.; Halliday, G.M.; Sue, C.M. PARK Genes Link Mitochondrial Dysfunction and Alpha-Synuclein Pathology in Sporadic Parkinson’s Disease. Front. Cell Dev. Biol. 2021, 9, 1755.
- Ariga, H.; Takahashi-Niki, K.; Kato, I.; Maita, H.; Niki, T.; Iguchi-Ariga, S.M.M. Neuroprotective Function of DJ-1 in Parkinson’s Disease. Oxid. Med. Cell. Longev. 2013, 2013, 683920.
- Martinat, C.; Shendelman, S.; Jonason, A.; Leete, T.; Beal, M.F.; Yang, L.; Floss, T.; Abeliovich, A. Sensitivity to Oxidative Stress in DJ-1-Deficient Dopamine Neurons: An ES- Derived Cell Model of Primary Parkinsonism. PLoS Biol. 2004, 2, e327.
- Taira, T.; Saito, Y.; Niki, T.; Iguchi-Ariga, S.M.M.; Takahashi, K.; Ariga, H. DJ-1 has a role in antioxidative stress to prevent cell death. EMBO Rep. 2004, 5, 213–218.
- Yanagisawa, D.; Kitamura, Y.; Inden, M.; Takata, K.; Taniguchi, T.; Morikawa, S.; Morita, M.; Inubushi, T.; Tooyama, I.; Taira, T.; et al. DJ-1 Protects against Neurodegeneration Caused by Focal Cerebral Ischemia and Reperfusion in Rats. J. Cereb. Blood Flow Metab. 2007, 28, 563–578.
- Sun, S.-Y.; An, C.-N.; Pu, X.-P. DJ-1 protein protects dopaminergic neurons against 6-OHDA/MG-132-induced neurotoxicity in rats. Brain Res. Bull. 2012, 88, 609–616.
- Miyazaki, S.; Yanagida, T.; Nunome, K.; Ishikawa, S.; Inden, M.; Kitamura, Y.; Nakagawa, S.; Taira, T.; Hirota, K.; Niwa, M.; et al. DJ-1-binding compounds prevent oxidative stress-induced cell death and movement defect in Parkinson’s disease model rats. J. Neurochem. 2008, 105, 2418–2434.
- Yanagida, T.; Kitamura, Y.; Yamane, K.; Takahashi, K.; Takata, K.; Yanagisawa, D.; Yasui, H.; Taniguchi, T.; Taira, T.; Honda, T.; et al. Protection Against Oxidative Stress-Induced Neurodegeneration by a Modulator for DJ-1, the Wild-Type of Familial Parkinson’s Disease-Linked PARK7. J. Pharmacol. Sci. 2009, 109, 463–468.
- Angeloni, C.; Zambonin, L.; Hrelia, S. Role of Methylglyoxal in Alzheimer’s Disease. BioMed Res. Int. 2014, 2014, 238485.
- Shaikh, S.; Nicholson, L.F.B. Advanced glycation end products induce in vitro cross-linking of α-synuclein and accelerate the process of intracellular inclusion body formation. J. Neurosci. Res. 2008, 86, 2071–2082.
- Cheng, L.; Zhang, W. DJ-1 affects oxidative stress and pyroptosis in hippocampal neurons of Alzheimer’s disease mouse model by regulating the Nrf2 pathway. Exp. Med. 2021, 21, 557.
- Chaudhuri, J.; Bains, Y.; Guha, S.; Kahn, A.; Hall, D.; Bose, N.; Gugliucci, A.; Kapahi, P. The Role of Advanced Glycation End Products in Aging and Metabolic Diseases: Bridging Association and Causality. Cell Metab. 2018, 28, 337–352.
- Lee, J.-Y.; Song, J.; Kwon, K.; Jang, S.; Kim, C.; Baek, K.; Kim, J.; Park, C. Human DJ-1 and its homologs are novel glyoxalases. Hum. Mol. Genet. 2012, 21, 3215–3225.
- Finkbeiner, S. Huntington’s Disease. Cold Spring Harb. Perspect. Biol. 2011, 3, a007476.
- Aleyasin, H.; Rousseaux, M.W.; Phillips, M.; Kim, R.H.; Bland, R.J.; Callaghan, S.; Slack, R.S.; During, M.J.; Mak, T.W.; Park, D.S. The Parkinson’s disease gene DJ-1 is also a key regulator of stroke-induced damage. Proc. Natl. Acad. Sci. USA 2007, 104, 18748–18753.
- Molcho, L.; Ben-Zur, T.; Barhum, Y.; Offen, D. DJ-1 based peptide, ND-13, promote functional recovery in mouse model of focal ischemic injury. PLoS ONE 2018, 13, e0192954.
- Yamane, K.; Kitamura, Y.; Yanagida, T.; Takata, K.; Yanagisawa, D.; Taniguchi, T.; Taira, T.; Ariga, H. Oxidative Neurodegeneration Is Prevented by UCP0045037, an Allosteric Modulator for the Reduced Form of DJ-1, a Wild-Type of Familial Parkinson’s Disease-Linked PARK7. Int. J. Mol. Sci. 2009, 10, 4789–4804.
- Mukherjee, D.; Chander, V.; Bandyopadhyay, A. PARIS-DJ-1 Interaction Regulates Mitochondrial Functions in Cardiomyocytes, Which Is Critically Important in Cardiac Hypertrophy. Mol. Cell. Biol. 2020, 41, e00106-20.
- Shimizu, Y.; Nicholson, C.K.; Polavarapu, R.; Pantner, Y.; Husain, A.; Naqvi, N.; Chin, L.S.; Li, L.; Calvert, J.W. Role of DJ-1 in Modulating Glycative Stress in Heart Failure. J. Am. Heart Assoc. 2020, 9, e014691.
- Wang, J.; Zhang, H.; Du, A.; Li, Y. DJ-1 alleviates anoxia and hypoglycemia injury in cardiac microvascular via AKT and GSH. Mol. Cell. Probes 2020, 53, 101600.
- Amatullah, H.; Maron-Gutierrez, T.; Shan, Y.; Gupta, S.; Tsoporis, J.N.; Varkouhi, A.K.; Teixeira Monteiro, A.P.; He, X.; Yin, J.; Marshall, J.C.; et al. Protective function of DJ-1/PARK7 in lipopolysaccharide and ventilator-induced acute lung injury. Redox Biol. 2021, 38, 101796.
- Liu, X.-W.; Ma, T.; Cai, Q.; Wang, L.; Song, H.-W.; Liu, Z. Elevation of Serum PARK7 and IL-8 Levels Is Associated With Acute Lung Injury in Patients With Severe Sepsis/Septic Shock. J. Intensive Care Med. 2017, 34, 662–668.
- Vörös, P.; Sziksz, E.; Himer, L.; Ónody, A.; Pap, D.; Frivolt, K.; Szebeni, B.; Lippai, R.; Győrffy, H.; Fekete, A.; et al. Expression of PARK7 is increased in celiac disease. Virchows Arch. 2013, 463, 401–408.
- Veres-Székely, A.; Bernáth, M.; Pap, D.; Rokonay, R.; Szebeni, B.; Takács, I.M.; Lippai, R.; Cseh, Á.; Szabó, A.J.; Vannay, Á. PARK7 Diminishes Oxidative Stress-Induced Mucosal Damage in Celiac Disease. Oxid. Med. Cell. Longev. 2020, 2020, 4787202.
- Zhang, J.; Xu, M.; Zhou, W.; Li, D.; Zhang, H.; Chen, Y.; Ning, L.; Zhang, Y.; Li, S.; Yu, M.; et al. Deficiency in the anti-apoptotic protein DJ-1 promotes intestinal epithelial cell apoptosis and aggravates inflammatory bowel disease via p53. J. Biol. Chem. 2020, 295, 4237–4251.
- Singh, Y.A.-O.; Trautwein, C.; Dhariwal, A.; Salker, M.A.-O.X.; Alauddin, M.; Zizmare, L.A.-O.; Pelzl, L.; Feger, M.; Admard, J.; Casadei, N.A.-O.; et al. DJ-1 (Park7) affects the gut microbiome, metabolites and the development of innate lymphoid cells (ILCs). Sci. Rep. 2020, 10, 16131.
- Anderson, C.A.; Boucher, G.; Lees, C.W.; Franke, A.; D’Amato, M.; Taylor, K.D.; Lee, J.C.; Goyette, P.; Imielinski, M.; Latiano, A.; et al. Meta-analysis identifies 29 additional ulcerative colitis risk loci, increasing the number of confirmed associations to 47. Nat. Genet. 2011, 43, 246–252.
- Cheng, Y.-T.; Ho, C.-Y.; Jhang, J.-J.; Lu, C.-C.; Yen, G.-C. DJ-1 plays an important role in caffeic acid-mediated protection of the gastrointestinal mucosa against ketoprofen-induced oxidative damage. J. Nutr. Biochem. 2014, 25, 1045–1057.
- Di Narzo, A.F.; Brodmerkel, C.; Telesco, S.E.; Argmann, C.; Peters, L.A.; Li, K.; Kidd, B.; Dudley, J.; Cho, J.; Schadt, E.E.; et al. High-Throughput Identification of the Plasma Proteomic Signature of Inflammatory Bowel Disease. J. Crohns Colitis 2019, 13, 462–471.
- Dubois, P.C.A.; Trynka, G.; Franke, L.; Hunt, K.A.; Romanos, J.; Curtotti, A.; Zhernakova, A.; Heap, G.A.R.; Adány, R.; Aromaa, A.; et al. Multiple common variants for celiac disease influencing immune gene expression. Nat. Genet. 2010, 42, 295–302.
- Moschen, A.R.; Gerner, R.R.; Wang, J.; Klepsch, V.; Adolph, T.E.; Reider, S.J.; Hackl, H.; Pfister, A.; Schilling, J.; Moser, P.L. Lipocalin 2 protects from inflammation and tumorigenesis associated with gut microbiota alterations. Cell Host Microbe 2016, 19, 455–469.
- Vasseur, S.; Afzal, S.; Tomasini, R.; Guillaumond, F.; Tardivel-Lacombe, J.; Mak, T.W.; Iovanna, J.L. Consequences of DJ-1 upregulation following p53 loss and cell transformation. Oncogene 2012, 31, 664–670.
- Qin, L.-X.; Tan, J.-Q.; Zhang, H.-N.; Rizwana, K.; Lu, J.-H.; Tang, J.-G.; Jiang, B.; Shen, X.-M.; Guo, J.-F.; Tang, B.-S.; et al. BAG5 Interacts with DJ-1 and Inhibits the Neuroprotective Effects of DJ-1 to Combat Mitochondrial Oxidative Damage. Oxid. Med. Cell. Longev. 2017, 2017, 5094934.
- Choi, D.-H.; Hwang, O.; Lee, K.-H.; Lee, J.; Beal, M.F.; Kim, Y.-S. DJ-1 cleavage by matrix metalloproteinase 3 mediates oxidative stress-induced dopaminergic cell death. Antioxid. Redox Signal. 2011, 14, 2137–2150.
- Lippai, R.; Veres-Székely, A.; Sziksz, E.; Iwakura, Y.; Pap, D.; Rokonay, R.; Szebeni, B.; Lotz, G.; Béres, N.J.; Cseh, Á.; et al. Immunomodulatory role of Parkinson’s disease 7 in inflammatory bowel disease. Sci. Rep. 2021, 11, 14582.
- Guo, X.L.; Wang, H.B.; Yong, J.K.; Zhong, J.; Li, Q.H. MiR-128-3p overexpression sensitizes hepatocellular carcinoma cells to sorafenib induced apoptosis through regulating DJ-1. Eur. Rev. Med. Pharm. Sci. 2018, 22, 6667–6677.
- Xiong, R.; Wang, Z.; Zhao, Z.; Li, H.; Chen, W.; Zhang, B.; Wang, L.; Wu, L.; Li, W.; Ding, J.; et al. MicroRNA-494 reduces DJ-1 expression and exacerbates neurodegeneration. Neurobiol. Aging 2014, 35, 705–714.
- Du, S.L.; Xu, L.Y.; Gao, P.; Liu, Q.S.; Lu, F.F.; Mo, Z.H.; Fan, Z.Z.; Cheng, X.L.; Dong, Z.H. MiR-203 regulates DJ-1 expression and affects proliferation, apoptosis and DDP resistance of pancreatic cancer cells. Eur. Rev. Med. Pharm. Sci. 2019, 23, 8833–8840.
- Cholez, E.; Debuysscher, V.; Bourgeais, J.; Boudot, C.; Leprince, J.; Tron, F.; Brassart, B.; Regnier, A.; Bissac, E.; Pecnard, E.; et al. Evidence for a protective role of the STAT5 transcription factor against oxidative stress in human leukemic pre-B cells. Leukemia 2012, 26, 2390–2397.
- Tanti, G.K.; Goswami, S.K. SG2NA recruits DJ-1 and Akt into the mitochondria and membrane to protect cells from oxidative damage. Free Radic. Biol. Med. 2014, 75, 1–13.
- Tanti, G.K.; Pandey, S.; Goswami, S.K. SG2NA enhances cancer cell survival by stabilizing DJ-1 and thus activating Akt. Biochem. Biophys. Res. Commun. 2015, 463, 524–531.
