Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Dean Liu and Version 1 by Diana Gabriela Santos.
The syphilis and COVID-19 pandemics have marked a turning point in the history of mankind. The aim of this review is to analyze what two pandemics caused by different diseases have in common.
- syphilis
- COVID-19
- pandemic
- sexually transmitted infections
1. Introduction
Humanity has experienced multiple pandemics throughout history, such as those caused by syphilis and COVID-19. Currently, nursing is bringing its practice closer to concerns related to ecology in order to make care sustainable. At first glance, they may appear to be two different diseases, but neither of them has left our society indifferent. The main objective of this article is to show the reality of two epidemics.
Thus, in the syphilis and COVID-19 pandemics, the emergency to care for a large number of people, the difficulties of accurate diagnoses, and the need for secondary and tertiary care in the short and long term were not met with sustainable plans and were trampled by immediate decisions with little rationality regarding the resources used. It is important to emphasize that public health is responsible for defining its instruments and means of work, considering global initiatives to face pandemics and future policies for control and reduction of harm to patients; at the same time, it must establish targets for early detection of cases in order to reduce or even extinguish contaminations.
Currently, more than one million people contract a sexually transmitted disease every day. Among the group of sexually transmitted diseases, only four are curable, one of which is syphilis [1]. On the other hand, COVID-19 has posed a global threat in which more than six million people have died. Severe acute respiratory syndrome (SARS) has left multiple sequelae in the population, some of them severe, such as erratic pain and depression [2]. Humanity has known about the existence of syphilis since at least 1493 [3]. It is a disease of considerable antiquity, as Hippocrates reported in the “Corpus Hippocraticum” about epidemics [4], like smallpox and syphilis, triggered by the austere conditions of the time [5].
Syphilis is a systemic and infectious disease caused by the bacterium Treponema pallidum, which belongs to the Spirochaete family. This Gram-negative bacterium is transmitted directly via sexual transmission (anal, oral, or vaginal) by the exchange of secretions present in mucous membranes, or by sharing infected objects, blood transfusions or vertical transmission from mother to fetus. This is how it has spread worldwide, affecting only humans [1]. If no curative measures are taken, syphilis can develop in three stages, which follow one after the other if no treatment is administered. Primary syphilis begins with the appearance of an ulcer called a syphilitic chancre at the infected site; it does not cause pain to the individual and presents a serous exudate at the base of the lesion; over a period of 3–6 weeks, it usually heals and disappears. In the case of secondary syphilis, the bacterium has reached the hematogenous pathway, causing a visible maculopapular rash on the hands and feet, mucosal involvement, diffuse alopecia, otitis, and meningitis, among others. If the disease continues to evolve, it results in tertiary syphilis, which usually appears several years after infection; its symptoms are much more accentuated, evidenced by lesions in multiple organs and bones, even leading to the dreaded neurosyphilis. It occurs in periods of latency and exacerbation. Early latent syphilis is usually associated with primary and secondary syphilis if there is a positive serology at the time of consultation or negative serology in the 12 months prior to consultation or positive serology together with having had intimate relations with someone infected. Manifestations of the disease that do not meet these conditions are treated as late latent syphilis [2].
2. Health Professionals: On the Frontline of the Battle against Syphilis and COVID-19
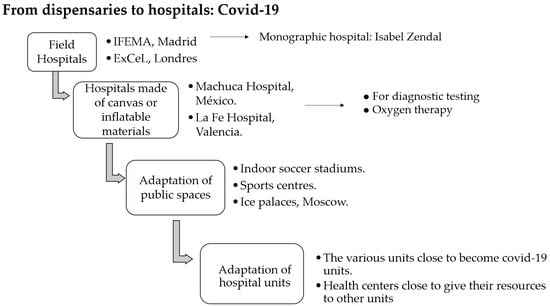
In order to combat diseases throughout history, health professions have evolved in order to provide a response to the sick population. This has been the case with syphilis and COVID-19, two different diseases that have made it necessary to implement similar measures to combat them. The first medical records kept on syphilis speak of cases of syphilis patients. Gaspar Torella did so in 1497 in Tractus cum consiliis (against) Pudendagram, seu morbum Gallicus. In 1502, Juan Almenar, another physician, wrote about the transmission of the disease: coitus, breastfeeding, and air. Gradually, medical evidence increased through the treatises written by different physicians explaining the etiology and treatment of the disease. Another important figure, who also gave the disease its name, was the Veronese physician Girolamo Fracastoro. He is very important in the history of medicine for his contributions to microbiology after describing how contagious diseases are transmitted. In some monographic hospitals, there is a figure of the surgeon and the apothecary. During the 16th century, the physician measured the heart rate of the syphilitic patient and analyzed their urine. He would then dictate to the surgeon which cures to be administered as well as the bleeding and shaving to be performed. Another of his functions was to tell the apothecary what medication to prepare. It was in the 1970s that the nurse became more important and took over most of the care of syphilitic patients. There were also other non-health professionals who took care of these patients, who were considered to be less qualified and worked in exchange for housing and food [26,27,28][6][7][8]. Today, the situation has changed. The disease is usually detected in primary care, where the general practitioner, after an anamnesis, indicates to carry out the relevant tests if he or she suspects that a patient may be infected. Another essential figure is the public health nurse, who not only prevents the disease through sex education but also helps to detect it. In cases of congenital syphilis, they are responsible for neonatal screening using antepartum blood tests to rule out the disease. Therefore, the intervention of the nursing team leads to a decrease in sexually transmitted infections (STIs) in the population. They educate about sexual behavior inside and outside the consulting room (schools, institutes) and in places where the risk is higher. Another function is the control of people who have or are suspected of having syphilis [29,62,63,64,65][9][10][11][12][13]. The health team is in charge of carrying out direct or indirect tests to detect syphilis. In direct tests, samples are taken from primary or secondary lesions. They are then examined using a darkfield microscope, direct immunofluorescence or polymerase chain reaction. Indirect tests look for the presence of antibodies in a serology. They are divided into treponemal and nontreponemal. Treponemal tests measure the amount of antibodies against Treponema pallidum antigens. Nontreponemal tests look for antibodies that are attacking cells affected by the infection, notably the syphilis serology test (VDRL) and rapid rlasma reagin (RPR) [30][14]. The pandemic caused by the coronavirus has marked a turning point in the history of humanity and the health system worldwide. Since the WHO officially declared the COVID-19 pandemic on 15 March, health professionals have been working hard to contain it. During the first waves, due to the uncertainty and the surprise it caused for all countries, a large majority of places had not gathered the material or the human and institutional resources to be able to deal with the disease [31][15]. At the beginning, there were no personal protective equipment (PPE) or tests to detect the disease, so they were faced with an invisible enemy that was becoming more widespread every day; stress was present in every health center, as well as exhaustion after many hours of work. The medical and nursing team was subjected to a situation unthinkable until now. Healthcare practice has to be evidence-based (EBM, EBP), and the pandemic was a setback to this principle, as drugs whose evidence was not strong enough to be used in patients had to be used. One example was hydroxychloroquine, which was even out of stock. It was surprising and demanding that regulatory authorities such as the Food and Drug Administration (FDA) approved treatments with a low level of proven efficacy, albeit on an exceptional basis. This leads uresearchers to reflect on whether we researchers should have a healthcare system that provides quicker and easier responses to trigger clinical trials in these situations. Moreover, at a calamitous time when health care staff had to decide which patients could use a ventilator or go to an intensive care unit, bioethics was affected. This was due to the lack of resources that caused the massive surge of people in hospitals. A difficult decision, as in a way, the Hippocratic principles governing the profession broke down. These had to take on a different meaning in order to comply with justice, beneficence, and nonmaleficence. It is worth mentioning that the mental health of healthcare workers has been severely affected, with many of them suffering from burnout syndrome. Currently, the incidence of this illness has decreased, so that situations of this dimension do not arise. However, conditions should be improved as these workers are still often overwhelmed [32,33,34][16][17][18]. The Food and Drug Administration (FDA) has approved two tests for the detection of the disease. The reverse transcription polymerase chain reaction (PCR) test involves obtaining a nasopharyngeal or oropharyngeal sample by inserting a swab through the nose or mouth to detect the presence or absence of nucleic acids from the virus. On the other hand, antigen testing consists of introducing a nasal swab to detect certain proteins of the virus. The presence of antibodies can also be measured using a serological test, which indicates immunity after passing COVID-19 or after vaccination. In SARS-CoV-2-infected patients with symptoms of pneumonia, a CT scan of the chest can be used; in positive cases, bilateral parenchymal ground-glass opacities and unilateral lung with subpleural lesions are observed [35][19]. The importance of healthcare professionals in making differential diagnoses should be emphasized. Syphilis has long been confused with leprosy, among other diseases, due to the dermatological lesions present in both. In the case of COVID-19, it is not only necessary to differentiate between influenza and other bacterial pneumonias, as well as syphilis, when presenting skin alterations such as erythema multiforme, vesicular rashes, palmoplantar pulpitis, and urticaria, there have been errors in the diagnosis until it was discovered that it was this condition. WReserache rs are dealing with two diseases that simulate skin diseases [36][20]. Just as the role of nursing became more important during the syphilis pandemic, the same occurred during the COVID-19 pandemic: the rise of professions that had previously been less well known. Nursing, physiotherapy, and psychology became more visible. The psychological consequences of confinement and the development of the syndemic itself left their mark on the population and on the professionals who had to continue working during quarantine. The intervention of psychologists was fundamental as a therapy for anxiety, anguish, and fear. Physiotherapy maintains an essential role in airway management when airway difficulties occur. Their presence in intensive care units has been paramount, as they provide therapy to improve lung function and capacity even for patients leaving the hospital [37,38][21][22].2. From Clinics to Hospitals
Since 1870, syphilis has been rife in hospitals, infirmaries, and surgeries. Already in World War I, the rise of this disease meant that thousands of soldiers were infected by sex workers who had not passed through health controls. France, a country with a high incidence of syphilis among its troops, created “washing stations”, where the soldier would go after having had sexual relations, if no more than three hours had passed. There, a professional would look for the presence of the disease. If nothing was found, he would go to another room where he was washed with hot water and soap, where a solution of protargol was injected into the urethra and held for 3–5 min. The name of the soldier and the day and time of the visit were recorded for a three-month follow-up. If the soldier subsequently tested positive for syphilis, he was not punished, as he was considered to have followed the treatment guidelines. In 1918, the presence of syphilis was still strong among the population, which led to the creation of “venereal treatment stations for soldiers and civilians” as a prophylactic measure, providing sex education and attempting to regulate the conditions of prostitution [40,41][23][24]. World War I marked a setback in the prevention of venereal diseases, which had been controlled since the 19th century. As early as 1623, Philip IV, King of Spain, banned prostitution to prevent the further spread of these diseases. Thus, legal brothels disappeared, and prostitution began to be practiced in the streets, which caused an uproar in society. At the end of the 18th century, proposals arose to regulate prostitution once again, and at the end of the 19th century, the creation of a doctor in charge of inspecting sex workers and their brothels was approved. As a result, in 1910, a team of medical hygienists was formed to take sex workers to antivenereal dispensaries. From then on, multiple dispensaries were set up to combat syphilis, offering their services to men and women if they came at separate times. These dispensaries were not sufficient, so numerous monographic hospitals were created, such as the Hospital San Juan de Dios and the General Hospital of Valencia in Spain. The first was founded in 1552 and was run by the brothers of the Order of St. John of God. This hospital achieved worldwide fame and was considered one of the best health centers for the mercurial treatments applied to treat syphilis [40,41][23][24]. The General Hospital of Valencia allocated up to four rooms for syphilitic patients, two for women and two for men. Infected people went there of their own free will, except in the case of sex workers, who were obliged to do so if they showed any signs or symptoms. This hospital acquired a great reputation for the treatments it used (Figure 31).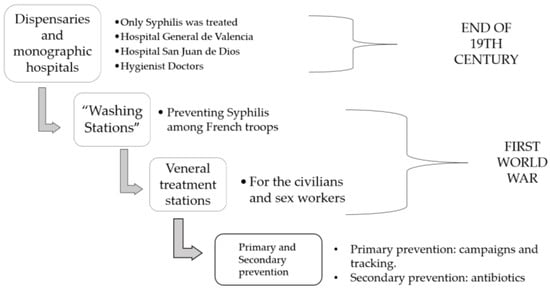
Figure 31. Dispensaries and hospitals where syphilis was treated. Source: authors’ elaboration.
3. Treatments Applied to Combat Two Pandemics and Notification of New Cases
To talk about treatments for syphilis, wresearche rs must go back to the year 1517. At that time, the wood of the guaiac tree that existed in America was used because it was thought that “God had put the remedy next to the disease”. After this, mercury began to be used, a method that spread over the decades and that was applied in various ways: by means of active rubbing or by means of sweating vats. In these tubs, the patient was placed inside the tub and the head was left outside. Mercury is a diuretic element that was thought to eliminate the toxins that caused syphilis, but it was not without side effects such as hypersalivation, loss of teeth, or intoxication. In 1907, Paul Ehrlich discovered a compound consisting mainly of arsenic. He called it product 606 or salvarsan. It was administered as a painful hypodermic injection, which caused it to have to be combined with morphine. Some healing of the chancre was observed, but it was highly toxic, even causing the death of some people. In 1917, Julius Waggner-Jauregg developed an innovative treatment that consisted of provoking fever in the syphilitic patient who was paralyzed. The fever could reach up to 41°C and had to be maintained for a few hours. Subsequently, the combination of iodine and mercury was tried, but it had many adverse reactions such as nephritis and pneumonia. Between 1922 and 1932, bismuth and sulphonamides were introduced, finally replacing the much used mercury [47][30]. COVID-19 has also posed a challenge to health professionals because, as a new disease, there was no drug approved for its use; in fact, there is currently no consensus on a drug that has specificity to treat this condition. As with syphilis, several treatments had to be tried before an effective one was found. The star treatment for syphilis came in 1943, when penicillin began to be used. Discovered by Alexander Fleming in 1928, this antibiotic began to be used by injection. The results were so astonishing that it is now the first line of treatment for syphilis. A single dose of penicillin G benzathine is effective in treating primary, secondary, and tertiary syphilis; in fact, it is the only approved treatment that pregnant women can receive. However, currently, the treatment of syphilis can be disparate, as it presents different forms of administration. In some countries, not only penicillin G benzathine is used, but also other oral antibiotics; leaving the intramuscular route of administration as hospital treatment, dosage depends on the stage of the disease [48,49][31][32]. The most common adverse reaction to this treatment is what is called a Jarisch–Herxheimer reaction, which causes fever, chills, nausea, and headache, lasting about 24 h. For those allergic to penicillin, there are alternatives, although it must be taken into account that the efficacy is not the same. They usually undergo a desensitization process. As a second option, ceftriaxone is the most commonly used, although other antibiotics are also known, but azithromycin is under study as it is considered a good candidate for treatment [47][30]. Unfortunately, wresearchers do not have an infinite supply of penicillin, and this has led to shortages in many countries. It has even resulted in many people not being able to receive this treatment. There are only four global suppliers of this antibiotic, so there is currently very little production of this treatment. The active ingredient is obtained by producers other than the suppliers, so when the suppliers fail, the amount of drug they can produce is directly affected. At present, to supply the health system with this drug, we researchers have to turn to China, which controls the market there, having three of the four companies that manufacture penicillin. This fact does not occur only in the present, as the first consignments of penicillin arrived legally in Spain in 1944. They came from Brazil and consisted of 12 injections, a ridiculous quantity for the demand that existed. At that time, the United States controlled the antibiotic market, and Spain had to sign an agreement to supply the country. Even so, the administration of this drug was far from simple, as the patient had to go before the National Penicillin Committee with a series of medical tests proving the need to be treated with penicillin. It was the committee that considered whether it was necessary and provided vouchers that could be used in pharmacies. This meant that most of the drug was obtained by smuggling. Therefore, in 1948, the possibility for Spain to make its own penicillin was approved [50,51,52][33][34][35]. For syphilis, there is still no vaccine, but there are studies trying to develop one; so far, Lithgow et al. have identified Tp0751, a vascular adhesin involved in the transmission of Treponema pallidum, but it has only been tested in animals with good results. If any-thing else, this pandemic has broken records in vaccine development at an unthinkable pace, with 184 vaccines in preclinical trials and 104 in clinical development by 2021. Vaccines come in four types: whole viruses, protein-based, viral vectors, and nucleic acids. At the end of 2020, vaccination campaigns were conducted, and the following vaccines were approved by the European Medicines Agency: Comirnaty® from Pfizer-BionTech, Spikevax® from Moderna, Vaxzetria® from Astra Zeneca, and COVID-19 Vaccine® from Janssen [35,53,54,55][19][36][37][38]. For COVID-19, different lines of treatment are being pursued. There are drugs that inhibit RNA-dependent RNA polymerase such as remdesivir. This drug is in trials for the treatment of Ebola, and the FDA had to approve its use as a matter of urgency as it is still in phase 3 studies. This preparation was applied to the first US patient and provided good results. In the same vein is favipiravir, an antiviral approved in Japan to treat influenza A, B, and C. It is in clinical trials for use in the US. It is in a clinical trial for use in patients with COVID-19 but shows a lower viral load in the upper respiratory tract and lungs. On the other hand, there are protease inhibitors, such as lopinavir/ritonavir, which is used in combination with other antivirals to treat human immunodeficiency virus. COVID-19 has shown low to moderate efficacy, so better results are expected with nelfinavir, the first choice for HIV treatment. There are also viral entry inhibitors such as hydroxychloroquine, a drug used for autoimmune diseases that is beneficial for the thrombotic events that frequently occur in COVID-19 infection. APNO1, used for pulmonary hypertension, reduces lung damage caused by the virus. Immune modulators and monoclonal antibodies are also available, among which tocilizumab stands out for its promising results in critically ill patients. Finally, Janus kinase inhibitors are used to reduce SARS-CoV-2 symptoms such as pulmonary oedema, liver damage, and kidney damage, as well as nutritional supplements such as vitamin C, vitamin D, and folic acid [35][19]. It is worth mentioning that, during the pandemic, there was almost daily reporting of cases on media platforms. One of them was Johns Hopkins University. The Spanish Ministry of Health also issued a survey to keep track of confirmed cases at the state level. In addition, Spain has a system of obligatory notifiable diseases that includes mandatory reporting of the incidence of syphilis and COVID-19 usually on a weekly basis [35,56,57,58,59,60][19][39][40][41][42][43]. The reporting and diagnosis of sexually transmitted diseases during the pandemic suffered a large decline [61][44].References
- Lasagabaster, M.A.; Maider; Guerra, L.G. Sífilis. Enferm. Infecc. Y Microbiol. Clínica 2019, 37, 398–404.
- Instituto de Salud Carlos III—ISCIII. Available online: https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Documents/PROTOCOLOS/Protocolo%20de%20Vigilancia%20de%20Sífilis.pdf#search=sifilis (accessed on 10 August 2022).
- World Health Organization (WHO). Infecciones de Transmisión Sexual. Available online: https://www.who.int/es/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis) (accessed on 10 August 2022).
- Pan American Health Organization/World Health Organization (OPS/OMS). Sífilis. Available online: https://www3.paho.org/hq/index.php?option=com_content&view=article&id=14869:sti-syphilis&Itemid=3670&lang=es#:~:text=Se%20trata%20de%20una%20infección,transmisión%20maternoinfantil%20durante%20el%20embarazo (accessed on 10 August 2022).
- Ministerio de Sanidad. Available online: https://www.sanidad.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/20220113_MICROBIOLOGIA.pdf (accessed on 10 August 2022).
- Ventura, D. Migrações Internacionais e a Pandemia de COVID-19. 2020. Available online: https://repositorio.usp.br/directbitstream/04b3ca3e-828a-4f43-bd0f-cb4b3fdaa279/miginternacional.pdf#page=95 (accessed on 11 August 2022).
- Mendizábal, D.A. Analogía Filosófica. 2021. Available online: https://www.uv.mx/personal/ramlopez/files/2018/04/ANALOGIAXXXVa.pdf#page=117 (accessed on 11 August 2022).
- Paixão, G.; Silva, R.; Carneiro, F.; Lisbôa, L. The Pandemic of the New Coronavirus (SARS-CoV-2) and Its Repercussions on Stigmatization and Prejudice. 2021. Available online: https://pesquisa.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/pt/covidwho-1328345 (accessed on 10 August 2022).
- Iommi Echeverría, V. Girolamo Fracastoro y la Invención de la Sífilis. 2008. Available online: https://www.redalyc.org/pdf/3861/386138051002.pdf (accessed on 10 August 2022).
- UNESCO. La Discriminación y el Estigma Relacionados con el COVID-19: ¿un Fenómeno Mundial? 2022. Available online: https://es.unesco.org/news/discriminacion-y-estigma-relacionados-covid-19-fenomeno-mundial (accessed on 10 August 2022).
- Mendoza, D.A.; Bedoya, W.A. 2 Seguimiento de Enfermería a Neonatos con Sífilis Congénita: Una Revisión Narrativa de la Literatura, 2015–2020. 2020. Available online: https://repositorio.unicordoba.edu.co/bitstream/handle/ucordoba/4230/Acosta%20Mendoza%2c%20Danna%20Marcela%20Anaya%20Bedoya%2c%20Wendy%20Jhoana.pdf?sequence=1&isAllowed=y (accessed on 11 August 2022).
- López Terrada, M. El Tratamiento de la Sífilis en un Hospital Renacentista: La sala del mal de Siment del Hospital General de Valencia. 1989. Available online: https://digital.csic.es/handle/10261/26239 (accessed on 12 August 2022).
- Almady Sánchez, E. Sífilis Venérea: Realidad Patológica, Discurso Médico y Construcción Social. Siglo xvi. 2021. Available online: https://www.scielo.org.mx/pdf/cuicui/v17n49/v17n49a10.pdf (accessed on 11 August 2022).
- García Ruiz, A.; Pablo Gormaz, R.; Marro Hernández, D.; Ezpeleta Esteban, L.; Bellostas Muñoz, P.; Coll Ercilla, M. Actuación Enfermera en la Prevención de Enfermedades de Transmisión Sexual. Una Revisión Bibliográfica. Revista Sanitaria de Investigación. 2022. Available online: https://revistasanitariadeinvestigacion.com/actuacion-enfermera-en-la-prevencion-de-enfermedades-de-transmision-sexual-una-revision-bibliografica/ (accessed on 10 August 2022).
- Pan American Health Organization (PAHO). Available online: https://iris.paho.org/bitstream/handle/10665.2/12060/v37n2p193.pdf?sequence=1&isAllowed=y (accessed on 10 August 2022).
- Revista Medica Sinergia. Vista de Sífilis: Abordaje Clínico y Terapéutico en Primer Nivel de Atención. Available online: https://revistamedicasinergia.com/index.php/rms/article/view/559/925 (accessed on 10 August 2022).
- Atención Primaria Práctica. Sífilis, a Propósito del Aumento de Casos en la Consulta. Elsevier|Una Empresa de Análisis de la Información|Empowering Knowledge. Available online: https://www.elsevier.es/es-revista-atencion-primaria-practica-24-articulo-sifilis-proposito-del-aumento-casos-S2605073019300604 (accessed on 10 August 2022).
- Berdasquera Corcho, D.; Rodríguez Gonzalez, I. El Médico de Familia y el Control de la Sífilis Después de una Estrategia de Intervención. 2006. Available online: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0864-21252006000300008#:~:text=Despu%C3%A9s%20de%20finalizada%20la%20intervenci%C3%B3n,muestran%20en%20la%20tabla%202 (accessed on 10 August 2022).
- Tranche Iparraguirre, S.; Martín Álvarez, R.; Párraga Martínez, I.; Tranche Iparraguirre, S.; Martín Álvarez, R.; Párraga Martínez, I. El Reto de la Pandemia de la COVID-19 Para la Atención Primaria. 2021. Available online: https://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1699-695X2021000200008 (accessed on 10 August 2022).
- Sacristán, J.; Millan, J. El Médico Frente a la COVID-19: Lecciones de una Pandemia. Educación Médica. 2020. Available online: https://www.elsevier.es/es-revista-educacion-medica-71-avance-resumen-el-medico-frente-covid-19-lecciones-S1575181320300747 (accessed on 10 August 2022).
- Zárate Grajales, R.; Ostiguín Meléndez, R.; Rita Castro, A.; Blas Valencia Castillo, F. Available online: https://www.scribd.com/document/510824689/Enfermeria-y-Covid# (accessed on 10 August 2022).
- Ugarte Gurrutxaga, M.; Gomez Cantarino, M.; Molina Gallego, B. Nursing Care in the COVID-19 Pandemic in the Spanish Health System. 2020. Available online: https://ruidera.uclm.es/xmlui/bitstream/handle/10578/28108/Nursing%20Care%20in%20the%20Covid-19%20Pandemic%20in%20the%20Spanish%20Health%20System.pdf?sequence=1&isAllowed=y (accessed on 10 August 2022).
- Revista de Patologia Respiratoria. Available online: https://repositorio.uta.edu.ec/bitstream/123456789/36760/1/Martinez%20Escobar%20Karla%20Estefania.pdf (accessed on 10 August 2022).
- Rodríguez Cebeiro, M. Psicólogos en el Frente: La Atención Durante la Crisis del COVID-19. De las Emociones Tóxicas a la Salud Psicológica. Arch. Med. 2021, 21, 225–241.
- CDC. COVID-19. Available online: https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html (accessed on 3 February 2023).
- Cunha-Oliveira, A.; Silva, M.; Afonso, M.; Peres, M.; Santos, T.; Queirós, P. Organización de los Servicios de Salud en Portugal a Principios del Siglo XX: El Caso de la Sífilis. Dialnet. 2022. Available online: https://dialnet.unirioja.es/servlet/articulo?codigo=8452263 (accessed on 10 August 2022).
- Cunha-Oliveira, A. Para uma História do VIH/Sida em Portugal e os 30 Anos da Epidemia (1983–2013); Coleção Ciências e Culturas; Imprensa da Universidade de Coimbra: Coimbra, Portugal, 2018; Volume 23, 122p.
- Fonseca, E.; Fernadez Flores, A.; Mones, A.; Moreno, J.C. III Seminario de Historia de la Dermatología. 2018. Available online: https://www.researchgate.net/profile/Eduardo-Fonseca-2/publication/336041338_III_Seminario_de_Historia_de_la_Dermatologia_Siguenza_Guadalajara_6_de_noviembre_de_2018/links/5d8bd65ca6fdcc25549a424e/III-Seminario-de-Historia-de-la-Dermatologia-Sigueenza-Guadalajara-6-de-noviembre-de-2018.pdf#page=57 (accessed on 10 August 2022).
- Candel, F.; Canora, J.; Zapatero, A.; Barba, R.; González del Castillo, J.; García-Casasola, G.; San-Román, J.; Gil-Prieto, R.; Barreiro, P.; Fragiel, M.; et al. Temporary hospitals in times of the COVID pandemic. An example and a practical view. Rev. Española Quimioter. 2021, 34, 280–288.
- Comunidad de Madrid. Hospital de Emergencias Enfermera Isabel Zendal. 2022. Available online: https://www.comunidad.madrid/centros/hospital-emergencias-enfermera-isabel-zendal (accessed on 10 August 2022).
- Nuño González, A.; Magaletskyy, K.; Martín Carrillo, P.; Lozano Masdemont, B.; Mayor Ibarguren, A.; Feito Rodríguez, M.; Herranz Pinto, P. ¿Son las alteraciones en la mucosa oral un signo de COVID-19? Estudio transversal en un Hospital de Campaña. Actas Dermosifiliogr 2021, 112, 640–644.
- Hevia, V.; Lorca, J.; Hevia, M.; Domínguez, A.; López-Plaza, J.; Artiles, A.; Álvarez, S.; Sánchez, Á.; Fraile, A.; López-Fando, L.; et al. Pandemia COVID-19: Impacto y reacción rápida de la Urología. Actas Urológicas Españolas 2020, 44, 450–457.
- Pereira Afonso, M.; Silva, M.; Aparecida Peres, A.; Dominguez Isabel, P.; Espina Jerez, B.; Cunha-Oliveira, A. Preparados Curativos Aplicados por Sanitarios al Sifilítico: Un Recorrido Histórico (s. XVI-XXI). Temperamentvm. 2022. Ciberindex.com. Available online: http://ciberindex.com/index.php/t/article/view/e18038d/e18038d (accessed on 10 August 2022).
- Pestoni Porvén, C.; Lado Lado, F.; Cabarcos Ortíz de Barrón, A.; Sánchez Aguilar, D. Sífilis: Perspectivas terapéuticas actuales. An. Med. Interna 2002, 19, 47–53.
- Peralta, R. Vista de Sifilis y Penicilina. 1945. Available online: https://revistas.unal.edu.co/index.php/revfacmed/article/view/26359/26694 (accessed on 10 August 2022).
- Guimaraes, K. El Desabastecimiento de Penicilina Pone en Jaque a la Salud Mundial. 2022. Available online: https://www.saludyfarmacos.org/lang/es/boletin-farmacos/boletines/ago201702/20_desa/ (accessed on 10 August 2022).
- Rodriguez Nozal, R. El Despacho de Penicilina en la España de las Restricciones y el Estraperlo. 2015. Available online: https://www.researchgate.net/publication/271824004_El_despacho_de_penicilina_en_la_Espana_de_las_restricciones_y_el_estraperlo (accessed on 10 August 2022).
- Ren, M.; Dashwood, T.; Walmsley, S. The Intersection of HIV and Syphilis: Update on the Key Considerations in Testing and Management. Curr. HIV/AIDS Rep. 2021, 18, 280–288.
- Hernández-Coronado, M.; Jaime-Pérez, J.; Villarreal-Martínez, A.; Ocampo-Candiani, J.; Gómez-Almaguer, D. Successful second outpatient autologous hematopoietic cell transplant for relapsed POEMS syndrome in a patient with coexisting HIV, HBV and syphilis infections during the COVID-19 pandemic. Transpl. Immunol. 2021, 67, 101412.
- Ndwandwe, D.; Wiysonge, C. COVID-19 vaccines. Curr. Opin. Immunol. 2021, 71, 111–116.
- Ministério de Sanidad. Centro de Coordinación de Alertas y Emergencias Sanitarias. Available online: https://www.sanidad.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/20211015_INMUNIDAD_y_VACUNAS.pdf (accessed on 10 August 2022).
- Ullrich, A.; Schranz, M.; Rexroth, U.; Hamouda, O.; Schaade, L.; Diercke, M.; Boender, T. Impact of the COVID-19 pandemic and associated non-pharmaceutical interventions on other notifiable infectious diseases in Germany: An analysis of national surveillance data during week 1–2016—Week 32–2020. Lancet Reg. Health Eur. 2021, 19, 100103.
- Bellmunt, J.; Caylà, J.; Millet, J. Estudio de contactos en infectados por SARS-CoV-2. El papel fundamental de la Atención Primaria y de la Salud Pública. COVID-19 En Atención Primaria 2020, 46, 55–64.
- Ministerio de Sanidad; Consumo y Bienestar Social; Portal Estadístico del SNS; Sistema de Información Sanitaria del SNS; Nivel de Salud y Estilos de vida. Enfermedades de Declaración Obligatoria. 2022; Sanidad.gob.es. Available online: https://www.sanidad.gob.es/estadEstudios/estadisticas/estadisticas/estMinisterio/declarObligatoria.htm (accessed on 10 August 2022).
More
