Previous studies showed that the cell-surface expression and function of the 5-HT transporter (SERT) in co-transfected cells are negatively modulated by α-Syn in a non-Abeta-amyloid component (NAC) domain-dependent manner
[71][115]. In addition, pioneering reports also showed direct interactions of α-Syn-SERT and γ-Syn-SERT proteins in cultured cells and in rat brain tissue, assessed by immunoprecipitation
[71][77][115,121]. α-Syn-induced modulation of SERT trafficking is microtubule-dependent, as the microtubule-destabilizing agent nocodazole disrupts the effects of α-Syn on SERT function, reversing the inhibition of uptake in co-transfected cells
[72][116]. More recently, in vivo studies indicated that down-regulation of α-Syn expression in raphe 5-HT neurons induced by an antisense oligonucleotide (ASO) leaves an increased synaptic 5-HT concentration, which was dependent on the reduction of SERT activity, as assessed by the selective SERT inhibitor citalopram
[74][118]. The overexpression of α-Syn in raphe nuclei produced the opposite effects, with mice exhibiting a drop in extracellular 5-HT levels that was dependent on SERT function
[78][110].
Moreover, α-Syn is also involved in the vesicular storage of monoamine neurotransmitters by the vesicular monoamine transporter 2 (VMAT
2). VMAT
2 mobilizes monoamines from the neuronal cytoplasm into vesicles, where they are repackaged for release at synapses
[79][80][122,123]. VMAT
2 co-localizes with α-Syn protein in the Lewy bodies from PD brains
[81][124], and overexpression of α-Syn negatively impairs VMAT
2 expression/function, leading to increased levels of cytosolic monoamine in presynaptic terminals, which in turn induce neurotoxicity
[69][113]. These findings suggest that α-Syn may maintain high VMAT
2 activity to protect monoamine neurons form cell death
[82][125].
4. Dysfunction of the 5-HT System in PD Patients
The investigation of premotor pathology presents one of the most difficult problems in PD research. Although Braak and colleagues
[26][83][26,126] proposed a significant premotor phase that may last as long as the symptomatic period, the identification of this phase in clinical practice is elusive. In fact, the profile of PD patients is also associated with diverse symptoms and clinical phenotypes
[84][127]. Cumulative evidence indicates the existence of ongoing pre-SNc DA neurodegeneration during the premotor phase leading to non-motor symptoms, mainly constipation, anxiety and depression, smell loss, and rapid-eye-movement (REM) sleep behavior disorder
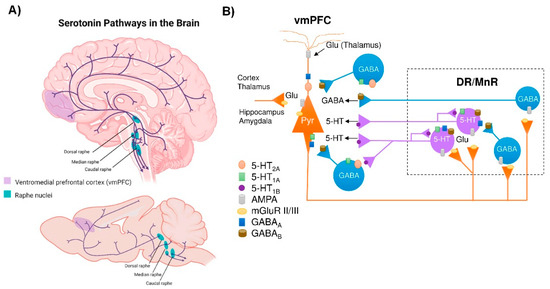
[85][128]. A dysfunctional 5-HT system is generally regarded as a risk factor for depression. Consistent with this view, several reports suggest a positive correlation between decreased 5-HT neurotransmission and the severity of depression and anxiety symptoms in PD, most likely caused by pathological changes of the 5-HT neurons in the midbrain raphe nuclei
[86][87][88][89][90][39,41,43,129,130].
By evaluating SERT availability with positron emission tomography (PET) and single photon emission computed tomography (SPECT) scans using various radioactive ligands, one can assess the integrity of the 5-HT system. The non-specific ligands [
123I]β-CIT and [
123I]FP-CIT have mostly been employed in in vivo SPECT imaging. Although these ligands have similar affinities for DAT and SERT, their thalamic and midbrain binding are considered to be SERT-specific
[91][131]. Hence, SPECT studies using [
123I]β-CIT and [
123I]FP-CIT found decreased binding in the thalamus and midbrain of PD patients
[92][93][94][95][96][132,133,134,135,136]. The PET ligands [
11C]-DASB and [
11C](+)McN5652 are highly specific for SERT. Using these ligands, several reports indicated reduced binding in different brain regions including the frontal cortex, striatum, and raphe nuclei
[97][98][99][137,138,139].
Importantly, neuropathological studies have demonstrated the presence of LBs (α-Syn positive staining) in raphe 5-HT neurons in the early stages of the disease
[100][101][102][103][148,149,150,151]. Previous studies on the propagation of α-Syn proposed that PD begins in the medulla oblongata with LB pathology in the dorsal motor nuclei of the glossopharyngeal and vagal nerves and the adjacent intermediate reticular zone
[83][104][126,152]. As PD progresses, it is proposed that the LB pathology spreads up the brainstem in an upward direction, affecting the raphe nuclei before reaching the SNc. In late stages, LBs are also found in limbic and cortical brain areas. The caudal groups of the raphe nuclei (e.g., raphe major, raphe obscure, and raphe pallidus) have been widely shown to contain LB-related lesions in the early stages of PD or even before the onset of motor symptoms
[83][104][105][126,152,153]. The 5-HT neurons found in the caudal raphe nuclei play a role in a number of autonomic processes, including pain and decreased gastrointestinal motility, which are recognized non-motor symptoms in PD.
5. Dysfunction of the 5-HT System in Animal Models with Overexpression of α-Syn
Abundant evidence suggests that the development of PD may comprise three main phases. The onset of α-Syn buildup in the CNS or PNS/ENS, in the absence of observable clinical symptoms, is referred to as the “preclinical PD” phase. The second phase, often known as the “pre-motor” or “prodromal,” can last for more than 10 years before the disease is clinically diagnosed. It is usually accompanied by the appearance of non-motor symptoms caused in part by pre-SNc abnormalities. During this phase, PD patients may display increased anxiety as early as 16 years prior to disease diagnosis; and depression becomes significantly prevalent among PD patients in the last 3–4 years preceding diagnosis. The third phase is the “motor phase of PD”, which is the one that is clinically visible and easiest to diagnose
[106][107][159,160]. Understanding the pathophysiological mechanisms underlying non-motor symptoms in PD is important, but requires relevant preclinical animal models. In this sense, one of the main shortcomings of current PD-like animal models is that they focus on DA pathways, which probably do not reflect the complexity underlying the occurrence of these symptoms in patients
[108][109][161,162].
In addition to the toxin-induced and genetic animal models of PD
[109][110][111][112][113][114][162,163,164,165,166,167], in recent decades, an alternative approach to modulate the disease based on the forced expression of wild-type or mutant human α-Syn using (1) transgenic techniques, (2) viral vector mediated transfer of α-Syn, or (3) injection of pathogenic pre-formed α-Syn fibrils (PFFs) has been presented. Thus, an intracellular accumulation of α-Syn in raphe 5-HT neurons and in hippocampal 5-HT fibers, without loss of 5-HT neurons in 12-week-old transgenic mice overexpressing mutant A53T α-Syn, was reported
[115][168]. In parallel, mice showed a reduced 5-HT release and compromised increase in doublecortin+ neuroblasts in the dentate gyrus (DG), indicating a differential neurogenic response
[115][168].
Recently, the adeno-associated virus (AAV)-α-Syn and PFFs models have been specifically adapted for study of α-synucleinopathies using stereotaxic delivery into different brain areas, making them useful tools
[116][171]. Therefore, a model of AAV-induced α-synucleinopathy selectively in 5-HT neurons of rats resulted in progressive degeneration of the 5-HT axon terminals in hippocampus, without the loss of raphe 5-HT neurons
[117][172].
In addition, some studies using cell cultures overexpressing α-Syn showed that 5-hydroxyindoleacetaldehyde (5-HIAL), a 5-HT metabolite product generated by monoamine oxidase (MAO-A), increases α-Syn oligomerization, which may explain the dysfunction of 5-HT neurons in PD
[118][176]. Recent studies also showed the importance of maintaining the integrity of 5-HT systems, as 5-HT itself can affect the growth of amyloid-forming protein fibrils. Indeed, 5-HT or selective serotonin reuptake inhibitors (e.g., escitalopram) activate signaling that alters the processing of α-Syn fibrils as well as amyloid precursor proteins into β-amyloid (Aβ) to prevent protein aggregation by direct binding, and could be beneficial to PD and other neurodegenerative disorders
[119][120][121][177,178,179].
6. Conclusions
The frequent occurrence of depression in PD is a prevalent and complex issue. Although often overlooked or underestimated, depression can seriously influence the course of PD and the quality of life of patients. In addition to dopaminergic depletion, several findings highlight the importance of serotonergic degeneration in PD. Thus, changes in 5-HT biochemical markers, LB pathology (α-Syn-positive staining) in raphe nuclei, and structural and functional alterations in the serotonergic system have been described, and it has been shown that these alterations in the serotonergic connectome are mainly associated with the expression of neuropsychiatric symptoms at disease onset. In support of this, the few available animal models demonstrating α-Syn-induced deficits in the serotonergic system recapitulate the mechanisms and early premotor stages of the disease. Altogether, measuring serotonergic integrity might be a useful in vivo tool to use in routines to guide the choice of the pharmacological arsenal in order to alleviate PD-related neuropsychiatric symptoms. Thus, such a measurement could serve as a sensitive marker of PD burden.