Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Ronghao Wang and Version 3 by Jessie Wu.
Prostate cancer (PCa) is the most common urological malignancy and brings great health threats to men.
- PCa
- cancer stem cells
- signaling pathway
- tumor
1. Introduction
Cancer cell heterogeneity can result from the differentiation program driven by a subset of unique cancer cells called cancer stem cells (CSCs), which have self-renewal potential and can differentiate into various types of cells in a symmetrical or asymmetrical cell divided manner [1][2][3][30,31,32]. In 2005, with the successful isolation of CD44+/α2β1hi/CD133+ enriched cells from a human prostate tumor, Collins et al. found that this small population of prostate cancer (PCa) cells possessed self-renewal ability and were enabled to differentiate into non-clonal tumor cells [4][33]. Other studies also demonstrated that CD44+ and PSA-/lo PCa cells shared similar properties with CD44+/α2β1hi/CD133+ enriched cells [5][6][7][34,35,36]. With decades of research, scientists have gradually recognized the existence and significance of these fractional cells in PCa using various biomarkers (Table 1) [8][9][10][11][12][13][14][15][16][17][18][19][20][21][22][23][24][25][26][27][28][29][30][31][32][37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61], which have stem cell characteristics and are then referred as prostate cancer stem cells (PCSCs)PCSCs. Now, it is clear that PCSCs are involved in the initiation, progression and therapeutic resistance of PCa.
Table 1.
Biomarkers for prostate cancer stem cells.
| Marker | Function | Reference |
|---|---|---|
| CD44 | CD44 is a glycoprotein involved in cell migration, adhesion and signal transduction | Kalantari E, et al., 2017 [8][37] |
| CD133 | CD133 is a transmembrane glycoprotein involved in cell self-renewal, differentiation and tumor invasion | Kalantari E, et al., 2017 [8][37] |
| CD117 | CD117 is a transmembrane glycoprotein involved in cell self-renewal, differentiation and tumor invasion | Harris KS, et al., 2021 [9][38] |
| α2β1 | α2β1 is associated with tumor invasion and proliferation | Aldahish A, et al., 2019 [10][39] Naci D, et al., 2015 [11][40] |
| EpCAM | EpCAM is a calcium independent adhesion molecule between epithelial cells involved in the process of epithelial cell carcinogenesis | Witte KE, et al., 2021 [12][41] |
| SOX2 | SOX2 plays an important role in maintaining stem cell pluripotency and self-renewal | Lee Y, et al., 2021 [13][42] Vaddi PK, et al., 2019 [14][43] |
| EZH2 | EZH2 is closely related to cell migration and invasion, tumor development and stem cell self-renewal | Huang J, et al., 2021 [15][44] |
| CXCR4 | CXCR4 is a specific receptor involved in physiological mechanisms such as HIV-1, hematopoiesis, embryonic development and tumor migration | Li Y, et al., 2019 [16][45] Chatterjee S, et al., 2014 [17][46] |
| TRA-1-60 | A cell surface epitope of human embryonic, embryonal germline and teratocarcinoma stem cells | Schafer C, et al., 2020 [18][47] |
| CD151 | CD151 is associated with tumor initiation, metastasis, and angiogenesis | Wong AH, et al., 2020 [19][48] |
| OCT-3/4 | OCT-3/4 is an essential transcription factor that maintains the multidirectional differentiation potential of embryonic stem cells and primordial germ cells | Wang X, et al., 2021 [20][49] Fujimura T, et al., 2014 [21][50] |
| Smo | Smo is a transmembrane protein that mediates Hedgehog signaling to the intracellular compartment | Lou H, et al., 2020 [22][51] |
| Nanog | Nanog is a transcription factor with an important role in stem cell self-renewal and maintenance of pluripotency | Verma S, et al., 2020 [23][52] Liu C, et al., 2020 [24][53] |
| Bmi-1 | Bmi-1 is associated with maintenance of self-renewal of prostate stem cells and inhibition of PTEN in PCa | Li Y, et al., 2017 [25][54] Yoo YA, et al., 2016 [26][55] |
| TWIST | TWIST is a transcription factor with a helix-loop-helix structure and associated with tumor invasion and metastasis | Lee Y, et al., 2021 [13][42] |
| CD24 | CD24 is a cell adhesion molecule involved in the regulation of B-cell proliferation and maturation | Costa CD, et al.,2019 [27][56] |
| CD166 | CD166 is a leukocyte adhesion factor associated with cell adhesion and tumor metastasis | Wei GJ, et al., 2019 [28][57] van Lersner A, et al., 2019 [29][58] |
| CD49b | CD49b is also called integrin α2, a cell surface receptor associated with adhesion and lymphocyte activation | Bansal N, et al., 2016 [30][59] Erb HHH, et al., 2018 [31][60] |
| ABCG-2 | ABCG-2 contributes to the resistance to chemotherapeutic drugs | Kim WT, et al., 2017 [32][61] |
2. The Role of Prostate Cancer Stem CellSCs in Prostate CancerCa Initiation
A number of literature studies have highlighted cancer stem cells as the origin of tumor initiation, including PCa. In the prostate gland, a small population of prostate stem cells (PSCs) undergo an oncogenic transformation to PCSCs when the external environment is unfavorable (Figure 1). Then, the omnipotent PCSCs give rise to various sub-types of prostate cancer cells, either AR-dependent or -independent, forming PCa heterogeneity. It seems that luminal-like PCa originates from progenitor cells in luminal epithelial cells. However, α2β1hi/CD133+ prostate stem cells were previously identified to be located in the basal layer [33][62]. Moreover, Witte et al. impressively found that it was the basal epithelial cells, but not luminal epithelial cells, growing to the prostate gland structure when they were subcutaneously implanted into nonobese diabetic scid gamma (NSG) mice [34][63]. Another study revealed that only basal epithelial cells with oncogenic induction led to prostatic intraepithelial neoplasia (PIN) and PCa in NSG mice [35][64]. All these findings together suggest that PCSCs in basal epithelial cells are the origin of PCa.
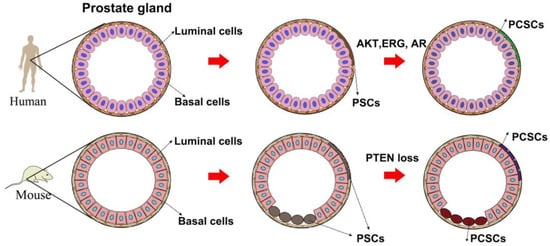
Figure 1.
A model of the origin of prostate cancer stem cells.
However, the origin of PCa in mice is different from that in humans. Studies by lineage tracing system elucidated that PSCs can be found in both the luminal and basal layers [36][37][65,66]. Further investigation illuminated that phosphatase and tensin homolog (PTEN) loss in either the basal layer or luminal layer led to PCa development. In the view of a CSCs-based hypothesis, PSCs in either the luminal layer or basal layer will transform to PCSCs when suffering from genetic alteration such as PTEN loss [38][67]. Although there is a little discrepancy between mouse PCa and human PCa regarding their origin (Figure 1), the concept of PCSCs as PCa origin has been widely acknowledged by many scientists: PSCs in the prostate epithelial cells undergo genomic instability to give rise to PCSCs when the environment is unfavorable, finally leading to PCa development.
3. The Role of Prostate Cancer Stem CellSCs in Prostate CancerCa Progression and Anti-Androgen Resistance
PCa with 2–3 years androgen deprivation therapy (ADT) treatment will eventually develop to castration-resistant disease, a lethal stage owing to its metastatic potential. By bypassing this systemic androgen suppression, AR signaling hijacks several means in order to efficiently respond to the castrated androgen level. AR amplification, AR mutation and selective up-regulation of AR co-regulators are the more frequently observed biological processes in castration-resistant prostate cancer (CRPC)CRPC as compared with primary tumors [39][40][41][42][12,68,69,70].
Growing evidence also illustrates that ADT treatment expands the population of PCSCs [43][44][45][29,71,72], which have no response to androgenic sources. Continuous AR signaling inhibition of CRPC is fulfilled by the treatment of FDA approved anti-androgen enzalutamide [46][47][23,26], which competes androgen to bind AR and suppresses AR nuclear imports [48][73]. However, it only benefits CRPC by extending to a five month survival [49][74]. One popular mechanism responsible for the acquired enzalutamide resistance is the selective expression of truncated AR variants. For example, ARv7, which lacks an androgen responsive domain, is a crucially causal factor controlling enzalutamide resistance [50][51][52][75,76,77]. Another important mechanism responsible for anti-androgen resistance is lineage plasticity [53][78], which is possibly driven by PCSCs. Accumulative evidence suggests that AR-targeted therapies including ADT and anti-androgen treatment considerably enrich the population of PCSCs by facilitating the transition of AR-dependent PCa cells to AR-independent cells with stem-cell-like states or multi-lineage stages [54][55][79,80]. PCSCs then re-differentiate into AR-therapy-resistant sub-clones such as neuroendocrine PCa cells or other lineage sub-clones inherently resistant to enzalutamide treatment. In this regard, PCSCs play critical roles in PCa progression and anti-androgen resistance.
