Cardioprotective devices such as TandemHeart, Impella family devices, and venoarterial extracorporeal membrane oxygenation (VA-ECMO) have been proven to show significant cardioprotection through mechanical support. However, their use as interventional agents in the prevention of hemodynamic changes due to cardiac surgery or percutaneous interventions has been correlated with adverse effects. This can lead to a rebound increased risk of mortality in high-risk patients who undergo cardiac surgery.
- cardiac surgery
- ventricular assist devices
- ischemia–reperfusion injury
1. Introduction
2. Cardiac Surgery/Percutaneous Procedures-Related Injuries and How They Affect Ventricular Performance
The most common cardiac-surgery-related injuries are supraventricular tachycardia (SVT), atrial fibrillation, bradycardia, atrioventricular block, cardiac arrest, reperfusion injury, and sudden cardiac death [3]. All of these pathologic states lead to altered ventricular performance and may additionally result in cardiogenic shock (CS) or congestive heart failure (CHF). They could also lead to decreased end-organ perfusion which could result in further complications and ultimately patient death [24][25][24,25]. Decreased end-organ perfusion is considered to be one of the major injury pathways related to cardiac-surgery-associated acute kidney injury (CSA-AKI), which is considered the most common clinically important complication following open heart surgery and is associated with high morbidity and mortality [25]. Furthermore, CS and CHF are considered to be the major causes of death in patients undergoing percutaneous coronary intervention (PCI) after ST-elevation myocardial infarction [26]. It is, therefore, imperative to preserve adequate cardiac output and end-organ perfusion by appropriately addressing CS or CFH to reduce patient morbidity and mortality preoperatively, intraoperatively, and postoperatively [25]. In regards to the use of PCI after acute myocardial infarction (AMI), reperfusion of the myocardium may also lead to reperfusion injury [3]. In this setting, reperfusion of the myocardium leads to a diffuse inflammatory response driven by increased oxidative stress, accumulation of cytokines and chemical mediators, complement activation, endothelial nitric oxide release, and induction of NO synthase (Figure 1) [3][24][3,24]. Systemic microvascular injury often follows in the affected ischemic–reperfused (I/R) tissues and other organs [24]. Ventricular malfunction, organ failure, post-surgery pulmonary edema, acute respiratory failure, and sudden patient death are just some of the feared outcomes of reperfusion injury [24][27][24,27].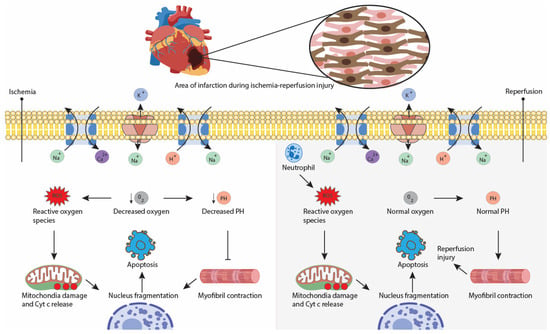
3. Principle of Ventricular Unloading
Ventricular unloading refers to the use of any therapy, maneuver, or intervention that decreases the power expenditure of the ventricle in order to minimize myocardial oxygen consumption (MVO2), and limits the hemodynamic forces that conduct to ventricular remodeling after any injury to the heart [29]. This is based on the concept that MVO2 is directly related to power expenditure and the total amount of work performed by the heart. In other words, the oxygen requirements of the heart depend mostly on total mechanical work and energy necessary for meeting the O2 demand by the body [29][30][29,30]. The harder the heart works to meet this demand, the higher the myocardial oxygen demand and consumption. In a healthy heart, an increase in O2 requirements by the body is adequately met by the activation of compensatory mechanisms, which allow the preservation of an adequate cardiac output and mean arterial pressure (MAP), resulting in a favorable oxygen supply [30]. Conversely, when the heart is injured (i.e., AMI), the functional capacity of the heart to preserve adequate cardiac output (CO) is compromised, as the viable myocardium becomes smaller [29][30][29,30]. The small viable myocardium has to work harder to maintain a favorable end-organ oxygen supply, resulting in higher stress on the heart. If not addressed, the higher myocardial stress inevitably leads to further myocardial damage and fewer viable myocardium. This results in a feedback loop where the burden of maintaining sufficient CO is placed on a lower and lower viable myocardium [30]. Thus, compensatory mechanisms such as heart rate and heart contractility are strongly activated, resulting in a higher MVO2 that ultimately will result in heart tissue remodeling [30]. However, compensatory mechanisms including heart tissue remodeling are limited, and depending on the extent of the AMI injury, this will ultimately lead to heart failure or even cardiogenic shock. Studies have shown that ventricular unloading before, during, or after an AMI can significantly improve cardiac function post-infarction by reducing infarct size [30][31][32][30,31,32].4. Benefits of Left Ventricular Unloading
The cardioprotective benefit of left ventricular (LV) unloading has particularly been documented in percutaneous coronary intervention for acute treatment of AMI. Studies strongly suggest that unloading the left ventricle before reperfusion (conversely to primary reperfusion) after an AMI can significantly limit infarct size [33]. More specifically, primary LV unloading 30 min before reperfusion has been proposed to significantly decrease infarct size in contrast to reperfusion alone and LV unloading 15 min before reperfusion. In biological terms and consistent with that result, LV unloading before reperfusion has been shown to downregulate the expression of genes involved in mitochondrial function and cellular respiration, thus lowering myocardial damage [32]. Moreover, stromal cell-derived factor-1α (SDF-1) and its receptor CXCR4 appear to be more elevated when LV unloading 30 min before reperfusion, compared with reperfusion alone or with LV unloading 15 min before reperfusion [32][34][32,34]. SDF-1 is a cardioprotective chemokine expressed in myocardial tissues after AMI. Finally, LV unloading lessens proapoptotic signaling by lowering proapoptotic proteins such as BAX and active caspase-3, and increasing anti-apoptotic proteins like BCL-2 and BCL-XL [32]. By minimizing myocardial scar formation after AMI and preventing ventricular remodeling through LV unloading, heart failure can be managed or even prevented [29]. While the principle of unloading has been principally used in the treatment and prevention of acute AMI and its complications, it has also been shown to be beneficial in the management of other cardiomyopathies such as peripartum cardiomyopathy, microvascular obstruction, and reperfusion-induced arrhythmias among others [29][35][29,35].5. Cardioprotective Devices That Unload the Heart:
Although the principle of LV unloading had been proposed to be beneficial for MVO2 lowering 40 years ago, it was not clinically possible to implement until the early-2000s when percutaneous ventricular assist devices for LV unloading started to develop [30]. Using a swine model of AMI and reducing LV workload with a TandemHeart device, Kapur et al. demonstrated for the first time that myocardial infarct size could be decreased by over 40% compared to reperfusion only [36]. Although there are currently many mechanical support devices (ECMO, IABP, surgical BiAVD), only two of them known as percutaneous ventricular assist devices (pVADs) are currently based on the LV unloading principle. These are TandemHeart (Livanova Inc., London, UK) and Impella (Abiomed Inc., Danvers, MA, USA) family devices. The mechanism by which pVADs work involves placing a catheter into the left ventricle LV, which draws blood and pumps it directly into circulation. This allows the reduction of workload on the heart without reducing the CO, thus preserving end-organ perfusion [29]. The use of pVADs in the setting of high-risk surgery holds various advantages, including preservation of end-organ perfusion, increasing time for decision-making regarding the best steps in management, and diminishing the burden and wear of the heart [37]. Although pVADS were originally used primarily for treating cardiogenic shock or heart failure, they are now used in surgical procedures, including ventricular tachycardia ablation and percutaneous procedures [38]. The main advantages and disadvantages of pVADS and other mechanical devices in PCI and cardiac surgery are comparatively described in Table 1.|
Uses in PCI and Cardiac Surgery |
||||
|---|---|---|---|---|
|
Ventricular Support |
Advantages |
Disadvantages/Limitations |
||
|
Devices that provide cardioprotection by improving hemodynamics or providing circulatory support |
Left ventricular support |
Hemodynamics improvement before and during PCI |
No significant improvement in mortality Data limited to observational studies Need of anticoagulant therapy before placement Invasive device: need of interatrial communication |
|
|
Left ventricular support Impella RP: right ventricular support |
Hemodynamics improvement before and during PCI Small size cannula Approved by the US Food and Drug Administration for high-risk PCI |
No significant improvement in mortality Significant major bleeding complications Need of anticoagulant therapy before placement May induce right heart failure |
||
|
Biventricular support |
Provides circulatory and respiratory support, ideal for patients undergoing biventricular failure Some studies show procedural success and no difference in outcomes compared to Impella family devices when used in high-risk PCI |
More research is needed to conclude its efficacy in high-risk PCI |
||
|
Right ventricular support |
Safe and feasible treatment in patients with acute right heart failure resulting from implementing a left ventricular assist device. In conjunction with TandemHeart, may offer up to a month of circulatory support. Minimal invasive percutaneous full right heart support ProtekDuo as a bridge to lung transplant and heart-lung transplant |
Efficacy and safety data on this device are limited. Drains only from the superior vena cava, making it harder to place it correctly in shorter patients. More expensive than a standard ECMO cannula (> USD 20,000) |
||
|
Left ventricular support |
Cost-effective method No need for anticoagulant therapy before placement |
Poor performance in patients with poor left ventricular function undergoing artery bypass surgery and cardiogenic shock |
||
|
Biventricular support |
Good outcomes when used in patients with chronic or acute biventricular failure as a bridge to transplant or recovery Beneficial in patients undergoing right-sided heart failure |
Need of sternotomy Ventricular arrhythmias after device placement More research needed to assess its efficacy in high-risk PCI |
||
|
IABP+ ECMO [20] |
Biventricular support |
May reduce mortality when treating profound cardiogenic shock (CS) Hemodynamics improvement before and during PCI |
Only small observational studies available, not enough for concluding efficacy. Poor data concerning IABP+ECMO in PCI |
|
|
Impella + VA-ECMO [21] |
Biventricular support |
May reduce mortality when treating profound CS Hemodynamics improvement before and during PCI |
Only small observational studies are available, which is not enough to conclude efficacy. Poor data concerning Impella+ECMO in PCI |
|
|
Devices that provide cardioprotection by the preservation of myocardial properties |
NA |
Used in people after induced cardiac arrest following surgery. May minimize ischemia–reperfusion injury, thereby improving cardiac surgery outcomes after cardiac arrest. Efficacious and easy to use in all pediatric cardiac surgeries. Key therapy in patients undergoing cardiopulmonary bypass surgery requiring cardiac arrest |
Risk of widespread intravascular crumpling Although it has been shown to have good results in clinical trials, more research is needed to show the same results in human trials |
|
|
Other approaches |
NA |
Non-invasive therapy Can induce intermittent cardiac asystole and can be used as an “on-off” switch for performing cardiac surgeries |
More research is needed to assess all the advantages and risks for its use in cardiac surgery [57] |
|
|
Pressure controlled intermittent coronary sinus occlusion [58][59][60][58,59,60] |
NA |
Increases the mean coronary sinus pressure and coronary sinus pulse pressure after a PCI PiCSO-assisted PCI has demonstrated smaller infarct size after 6 months |
Limited to treating anterior ST-elevated myocardial infarction More research needed |
|
|
NA |
Reduces infarct size. Improves reperfusion injury. Reduces endothelial edema and capillary vasodilation. Can be started 5 min after successful revascularization, without delaying primary PC |
Relatively new therapy with unknown long-term outcomes |
||
