Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Cesare Maino and Version 3 by Dean Liu.
Gastric cancer represents one of the most common oncological causes of death worldwide. In order to treat patients in the best possible way, the staging of gastric cancer should be accurate. In this regard, endoscopy ultrasound (EUS) has been considered the reference standard for tumor (T) and nodal (N) statuses in recent decades. However, thanks to technological improvements, computed tomography (CT) has gained an important role, not only in the assessment of distant metastases (M status) but also in T and N staging.
- stomach neoplasms
- positron emission tomography computed tomography
- tomography
- magnetic resonance imaging
1. Endoscopic Ultrasonography (EUS)
EUS is a combined technique used for endoscopy and high-frequency ultrasound (5–12 Hz) that provides high-resolution images with a limited penetration depth (between 1 and 6 cm). Dilatation of the lumen (200–400 mL) with water may contribute to a better assessment of the gastric walls.
The normal gastric wall is presented as a 5- to 9-layered structure [1][17], according to the high resolution of the probes: not all layers correspond to the histological ones, since some of them can present echoes due to interfaces. The two inner layers (hyper and hypo-echoic, respectively) represent the superficial mucosa and the muscularis mucosa. The 3rd (hyperechoic) layer corresponds to the submucosa, the 4th (hypoechoic) to the muscularis propria, and the 5th (hyperechoic) to the serosa, which is usually not easily distinguishable from the surrounding hyperechoic adipose tissue.
Nowadays, there is no consensus on the normal thickness of the gastric wall, but 2–4 mm should be considered the normal range [2][18].
GC usually presents as inhomogeneous hypoechoic wall thickening that is focal or diffuse, affects one or more layers, has possible growth outside the wall and eventually infiltrates other structures [1][17].
T and N Staging
The overall accuracy of EUS for T staging ranges from 65 to 92.1%. In particular, the sensitivity and specificity for serosa involvement range from 77.8 to 100% and from 67.9% to 100%, respectively [3][9]. By grouping GC according to the WHO classification, the sensitivity for more invasive tumors increases and ranges from 88.1% for T1 to 99.2% for T4 [4][19].
Although EUS is considered the imaging modality of choice for locoregional staging of GC, it has several limitations. First, it is an operator-dependent technique that is invasive and is associated with sedation-related complications. In addition, not all gastric regions can be easily assessed, and special attention is paid to the lesser curvature, subcardiac region and gastroesophageal junction. The same problems occur with extensive ulceration and with large lesions [5][20].
Nodal metastases are visualized on EUS as roundish, hyperechoic metastases located in perigastric zones. The overall accuracy of EUS in N staging generally ranges from 66 to 90% [6][7][21,22] with low sensitivity values for stages N2 and N3 [6][21]. One of the most important advantages of EUS in N staging is the possibility of fine needle aspiration (EUS-FNA), which contributes to the improvement of the overall accuracy. In this regard, the sensitivity, specificity and positive predictive value of EUS-FNA increase to 92%, 98% and 97%, respectively [8][23].
In addition, EUS has a limited depth of penetration and is therefore of limited use in the evaluation of distant metastases, which are usually investigated by other diagnostic methods [8][23].
Table 1. Details of the most important papers regarding the usefulness of EUS in the staging of GC patients.
| Ref # | Manuscript Type | Main Findings |
|---|---|---|
| [4][19] | Meta-analysis |
|
TNM Staging
As mentioned above, CT can be considered a useful tool for the staging of GC patients. However, MRI should also be considered for these purposes. In fact, a meta-analysis [17][44] comparing the diagnostic value of the most common imaging modalities for the staging of GC was published in 2012. This showed that the overall accuracy in the T-stage assessment of MRI was statistically better than that of CT (82.9% ± 3.7% vs. 71.5% ± 2.7%). MRI also appeared to be better than CT in terms of sensitivity in assessing the N parameter of GC (85.3% and 77.2%, respectively). Another meta-analysis [18][45] showed that the pooled sensitivity of MRI in diagnosing GC stages T1, T2, T3 and T4 was 66%, 85%, 86% and 88%, respectively, and it was 86% for correctly assessing the N parameter. When analyzing the diagnostic values according to the T stage, some authors [19][46] reported that CT and MRI had accuracy levels of 37.5% and 50% for the T1 stage and 81.2% and 88.7% for the T2 stage, respectively; moreover, they showed no significant differences in accuracy in the evaluation of T3 and T4 lesions, suggesting that MRI may be more suitable for identifying EGC. These aspects were confirmed in a similar study [20][47], which reported that MRI was superior for detecting T1 lesions compared with CT (50% vs. 37.5% accuracy for MRI and CT, respectively) [21][37], with overall accuracy levels of 60% and 48% for the T stage and 68% and 72% for the N stage, respectively. Finally, a 2017 systematic review [22][48] found that both the specificity and sensitivity of MRI were greater than those of CT (86% vs. 83% and 88% vs. 86%, respectively), although without statistical significance. Advances in imaging techniques, such as the introduction of diffusion-weighted imaging (DWI), may provide important data for the definitive diagnosis of various pathologic entities. In this context, DWI can help to distinguish T4 from the lower stages of GC with a high reliability [23][49]. The authors reported a sensitivity of 92.1%, specificity of 75%, and accuracy of 89.1% for ≤T2 vs. ≥T3 lesions and a sensitivity of 75%, specificity of 88.5%, and accuracy of 82.6% for ≤T3 vs. T4 lesions in 46 patients (Figure 19).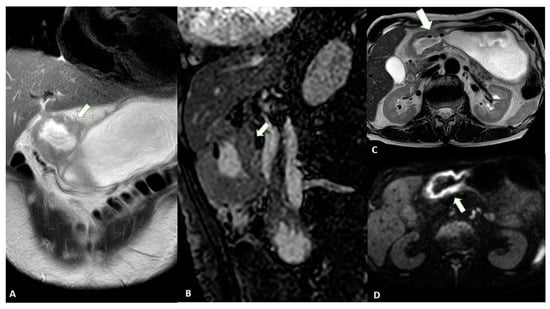
Figure 19. MRI images of a T3 gastric cancer of the gastric antrum in a 79-year-old male patient. (A) Coronal 2D image and (C) Axial 2D image of the Turbo Spin Echo (TSE) T2 sequence showing a circumferential lesion (arrow) invading the subserosa layer with an intermediate signal intensity; (B) Coronal 2D Balance Fast Field Echo (BFFE) sequence showing a circumferential lesion (arrow) with a low signal intensity; (D) Axial Diffusion Weighted Image (DWI) showing an area of signal restriction (arrow) corresponding to the tumor.
Table 24.
Details of the most important papers regarding the usefulness of MRI in the staging of GC patients.
| Ref # | Manuscript Type | Main Findings |
|---|---|---|
| [17][44] | Meta-analysis |
|
| [5][20] | Original study |
|
| [6][21] | Original study |
|
| [7][22] | Original study |
|
2. Computed Tomography (CT)
Before performing CT, the patient must be fasting for at least 6 h, and pharmacological hypotonization is achieved with 10–20 mg of butylscopolamine bromide administered intramuscularly or intravenously 10 to 15 min before the examination [9][24]. To achieve optimal gastric distension, negative (air) or neutral (water or methylcellulose) contrast agents are usually used to better visualize the enlargement of each layer of the gastric wall [10][25]. The administration of intravenous contrast medium is mandatory for the examination of the gastric walls. CT images should be acquired at least in the unenhanced phase and approximately 70 s after injection, the optimal time for GC enhancement. To assess the presence of vascular variants of the stomach, arterial phase imaging can be added [11][26]. Finally, postprocessed reconstructions (multiplanar reconstructions—MPR) in the coronal and sagittal planes can provide a better assessment of the tumor location and depth. Virtual gastroscopy (VG) is a CT-reconstructed three-dimensional (3D) endoluminal image set that simulates an endoscopic view. For VG, air is the preferred oral contrast agent. Limitations of this technique include the additional time (10 to 20 min) required to process the images and the higher level of technical expertise needed. Normal gastric walls show a multilayered pattern with an inner enhancing layer that histologically corresponds to the gastric mucosa. The intervening hypoattenuating layer represents the submucosa, and the outer, slightly hyperattenuating layer of variable thickness corresponds to the muscularis propria and serosa layer [12][27]. Gastric cancer presents as focal or diffuse wall thickening characterized by inhomogeneous enlargement that destroys normal gastric wall structures [12][27]. Therefore, the size of the gastric wall thickening and the degree of enhancement may affect the detection rate and accuracy of T-staging. In particular, focal thickening of greater than 5 mm in a well-expanded stomach is considered a neoplastic lesion [13][28].3. Magnetic Resonance Imaging (MRI)
In the past, MRI had a limited role in the evaluation of GC, especially because of the presence of motion artifacts, the long examination time, and the high cost [14][41]. However, in recent decades, major advances have been made in MRI technology that have improved the diagnostic performance in many areas of medicine, including oncology. These improvements include rapid breath-hold imaging techniques, abdominal bandage placement, the administration of anti-inflammatory drugs, and the use of phased array coils. MRI has the great advantage of providing superior soft tissue contrast and multiple imaging sequences without radiation-related risks. In addition, the high quality soft tissue imaging achieved with MRI allows the visualization of the anatomic wall layers [15][42]. However, the guidelines for the treatment of GC do not specify MRI as a possible imaging modality for staging. In addition, the most recent TNM guidelines do not recommend the use of MRI for the imaging assessment of T, N or M parameters in GC [16][43].| [18][45] | Meta-analysis |
|
| [19][46] | Original study |
|
| [22][48] | Meta-analysis |
|
| [23][49] | Original study |
|
| [24][50] | Original study |
|
| [25][51] | Original study |
|
