2. OSA and Inflammation
The continuous stress caused by recurrent snoring and repetitive closure and re-opening of the upper airway in patients with OSA can lead to mucosa inflammation
[25][26][26,27]. Low-grade inflammation causes remodelling of the upper airway, with increased deposition of connective tissue in the mucosa and muscles. Consequently, introducing changes to the morphology of palatopharyngeal muscle, inflammation and denervation contribute to upper airway obstruction during sleep in patients with OSA
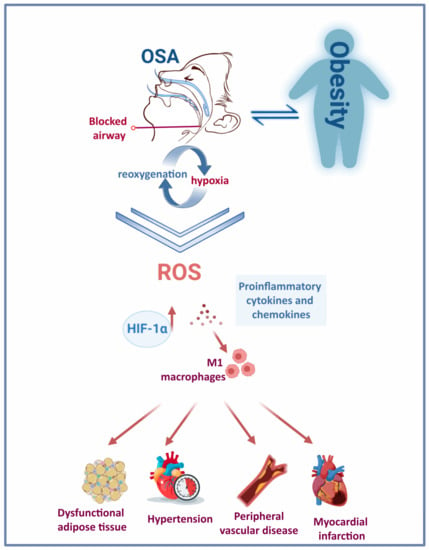
[27][28][28,29]. Therefore, systemic and localised inflammation induced by IH and the repeated cycles of hypoxia and reoxygenation (
Figure 1) features several events: induction of oxidative stress, reactive oxygen species (ROS) production
[29][30], activation of a critical proinflammatory transcription factor (nuclear factor κB (NF-kB))
[30][31], elevated expression of proinflammatory cytokines and chemokines
[31][32][32,33], recruitment and infiltration of the proinflammatory M1 macrophages
[29][33][30,34] in different tissues such as vessels, heart, adipose tissue and liver. Eventually, this contributes to vascular remodelling, metabolic dysfunction
[34][35] and atherosclerosis
[35][36].
Figure 1. Obesity and OSA: a bidirectional interaction. The repetitive cycles of hypoxia-reoxygenation due to frequent blockage of the upper airway in people with OSA triggers the activation of various pathological mechanisms and induces a rise in HIF-1α. The chronic presence of this condition has deleterious consequences on the cardiovascular system.
Indeed, upper airway tissue biopsies from patients with OSA showed subepithelial oedema and increased inflammatory cell infiltration
[27][36][37][38][28,37,38,39]. In addition, some studies have also reported increased levels of exhaled nitric oxide in patients with OSA
[39][40][41][42][40,41,42,43]. However, a recent meta-analysis showed no significant differences in exhaled nitric oxide relative to control groups
[43][44]. Although the association between localised inflammation and OSA is well established, whether systemic inflammation correlates with OSA is debatable. Some studies reported elevated levels of biomarkers of systemic inflammation, including proinflammatory cytokines such as interleukin (IL)-6 and C-reactive protein (CRP) in patients with OSA
[44][45][45,46]. Contrariwise, others found no association between OSA and CRP or IL-6 levels
[46][47][47,48]. In an Icelandic cohort study, OSA severity affected IL-6 levels only in obese subjects, while CRP levels were solely associated with OSA severity in obese men and postmenopausal women
[48][49]. This well-established correlation between obesity, a common OSA risk factor, and levels of IL-6 and CRP makes such molecules potential confounding factors in these studies. More recently, a study proposed Pentraxin-3 (PTX-3) as a biomarker of inflammation in patients with OSA as well as an indicator of disease severity
[49][50].
Studies suggest that OSA-associated systemic inflammation results from the overflow of inflammatory cytokines, which reach the bloodstream from the upper airway mucosa. This mechanism has been proposed in other respiratory conditions such as chronic obstructive pulmonary disease
[50][51]. Vincente et al. explored the possible association between local upper airway and systemic inflammation by assessing the levels of proinflammatory markers—IL-6, IL-8, tumour necrosis factor α (TNF-α) and CRP—and activated leukocytes in both pharyngeal lavage (PHAL) and plasma samples of patients with severe OSA, snorers and healthy control subjects
[38][39]. Though higher levels of IL-6, IL-8 and CD4
+ T-cells were found in the PHAL of severe OSA patients (apnoea–hypopnoea index (AHI) ≥ 30 per h), plasma inflammatory cytokines did not differ between patients with severe OSA and control groups. Thus, these findings do not support a link between local and systemic inflammation in patients with OSA
[38][39].
3. OSA and Obesity
OSA is intimately associated with obesity, with OSA being diagnosed in more than 30% of people with obesity and 50–98% of people with morbid obesity
[51][73]; thus, a higher BMI score increases the likelihood of developing OSA
[52][74]. Both conditions are associated with severe cardio-metabolic complications. The rising prevalence of OSA in the past 20 years concurred with increasing prevalence of obesity worldwide
[53][75]. Obesity is an established major risk factor for OSA
[52][54][74,76]. Three extensive cohort studies have shown that weight gain is associated with an increased risk of developing moderate to severe OSA and correlated with increased AHI. In contrast, weight loss coalesced with reduced AHI and OSA severity
[11][55][56][11,77,78]. Several reports proposed obesity as a factor contributing to the pathogenesis of OSA by increasing fat deposition in the parapharyngeal fat pads and tongue, thus narrowing the upper airway
[57][58][79,80]. Furthermore, obesity can cause chest and abdominal wall compression, reducing tracheal tension and contributing to a more collapsible upper airway
[54][59][76,81]. Obesity was associated with the severity of blood oxygen desaturation during apnoea and hypopnoea, thus likely aggravating OSA symptoms in these patients
[60][82].
On the other hand, the relationship between OSA and obesity may be reciprocal, as OSA may also contribute to weight gain. Many patients have reported gaining weight on the onset of OSA diagnosis
[61][62][83,84]. Several aspects of OSA may contribute to the development or aggravation of obesity: the fragmented sleep pattern associated with OSA affects dietary habits and sleep duration, leading to hormonal changes that affect satiety and energy expenditure
[63][85]. Increased daytime sleepiness and fatigue also contribute to reduced physical activity, leading to weight gain and increased risk of obesity comorbidities
[51][73]. CPAP therapy may also impact body weight in patients with OSA. Meta-analyses of randomised controlled trials showed that CPAP therapy led to a small but significant increase in body mass index
[34][35], particularly in high-usage patients
[64][86]. However, these analyses involved studies of relatively short duration (median of 3 months). Contrastingly, a post hoc analysis of the Sleep Apnea Cardiovascular Endpoints (SAVE) cohort showed that long-term use of CPAP (>3 years) did not have a significant impact on body weight in patients with comorbid OSA and cardiovascular disease
[65][87].
Notably, both OSA and obesity trigger the secretion of proinflammatory factors. An increasing body of evidence supports the common pathways by which obesity and OSA-associated IH lead to inflammation and dysfunction of adipose tissue (
Figure 1). However, given the similar mechanisms that trigger low-grade inflammation in obesity and OSA, discerning between OSA-specific and obesity-triggered inflammatory biomarkers remains challenging
[66][88]. In addition, proinflammatory cells are targeted at dysfunctional adipose tissue, producing proinflammatory factors such as TNF-α, IL-6, IL-1β, monocyte chemotactic protein (MCP)-1, resistin and leptin
[67]. Levels of the proinflammatory cytokines IL-17 and IL-23 were significantly elevated in paediatric OSA cases
[68][69]. In a study involving children with obesity and OSA, IL-17 was significantly associated with OSA, while IL-23 levels correlated with body fat and liver enzymes. Therefore, studies proposed these proinflammatory cytokines as potential biomarkers of paediatric OSA
[69][70]. Additionally, leptin levels significantly increased in people with sleep disorder breathing. The rise in leptin levels correlated directly with BMI Z-score, AHI
[69][70][71][70,71,72] and fasting insulin
[69][70]. The relationship between OSA and cytokines was corroborated by an observational study showing the diurnal variation of IL-6, IL-8 and TNF-α with the expression of symptoms in patients with mild OSA
[72][68].
Repeated exposure to hypoxia alters gene transcription and posttranslational protein modification, influencing metabolic and cardiovascular processes. OSA and obesity both trigger hypoxia-inducible factor 1 (HIF-1) in adipocytes, ultimately stimulating the expression of downstream angiogenic proteins to increase oxygen and nutrient delivery to adipocytes. Primarily responsible for maintaining stable oxygen metabolism, HIF-1 is an attractive target that is selectively induced by chronic IH and promoted by oxidative stress. The heterodimeric complex comprises two different proteins: HIFα and HIFβ. Both belong to a family of transcription factors constitutively expressed in cells
[73][89]. HIF-1α is oxygen-sensitive and couples with von Hippel-Lindau protein during normoxia to trigger its degradation by proteasomes
[74][90]. The degradation of HIF-1α is inhibited under hypoxic conditions
[75][91]. It is estimated that HIF-1 activates over 100 distinct genes
[76][92]. Consequently, HIF-1 is a critical transcription factor that regulates numerous processes, including the metabolism and cardiovascular system
[76][77][92,93]. However, many signalling pathways in which it participates remain poorly understood. Among numerous others, it stimulates genes associated with angiogenesis or glucose uptake by cells, i.e., glucose transporter 1 and glucose transporter 4
[76][78][92,94].
4. OSA and Cardiovascular Disease
OSA is a recognised independent risk factor for CVD and is associated with metabolic abnormalities that are closely linked to cardiovascular diseases. In accordance with this, OSA is associated with hypertension
[79][80][81][104,105,106], which puts patients with OSA at increased risk of developing cardiovascular complications such as coronary artery disease and stroke
[82][107]. Hypertension affects 36.5–53.6% of patients with OSA, depending on severity of the condition
[83][84][108,109]. Mechanisms driving increased blood pressure in patients with OSA are well described. Obstruction of the upper airways leads to hypoxemia, hypoxia, hypercapnia and changes in intrathoracic pressure, which, combined with frequent arousal from sleep, induces sympathetic system activation, increasing both heart rate and blood pressure. These hemodynamic changes contribute to tachycardia and hypertension, which can develop into left ventricular hypertrophy and heart failure
[82][107].
Chronic OSA is linked to oxidative stress due to the elevated synthesis of ROS brought on by the frequent episodes of IH and reoxygenation, which contribute to the development of oxidative stress. Several cross-sectional studies have examined different oxidative stress markers in patients with OSA. For example, high-sensitivity CRP, metalloproteinase 9 and copper correlate with higher AHI and lower haemoglobin oxygen saturation
[85][86][110,111]. Similar results were reported with the protein disulfide reductase thioredoxin
[87][88][112,113]. In addition, Malondialdehyde, a common biomarker of lipid peroxidation, has also been associated with OSA, correlating with the duration of nocturnal oxygen desaturation below 85%
[89][90][91][114,115,116].
Furthermore, patients with OSA presented with higher levels of oxidised LDL compared with healthy controls
[92][93][117,118]. Additionally, the presence of OSA concurred with lower ferric-reducing antioxidant power (FRAP) compared with controls, which negatively correlated with AHI
[94][95][119,120]. On the other hand, several oxidative stress biomarkers did not correlate with OSA: 8-isoprostane, thiobarbituric acid-reactive substances, erythrocyte catalase activity, copper-zinc superoxide dismutase (SOD) and total antioxidant capacity
[96][97][121,122]. While the benefit of CPAP therapy in reducing oxidative stress biomarkers in patients with OSA is debatable
[98][99][56,123], antioxidant therapy is effective in reducing oxidative stress and is a potential alternative to CPAP in patients with OSA
[100][101][102][124,125,126]. Several studies have investigated polyphenols as a treatment for OSA. Grebe et al. reported improved endothelial health through measurements of flow-mediated dilation (FMD) of the brachial artery. This study reported lower FMD measurements in a group of patients with OSA after receiving vitamin C intravenously compared with controls
[103][127]. Additionally, vitamins C and E have been studied for their potential to mitigate oxidative stress in laboratory rodents and other animal models. Higher levels of malondialdehyde (MDA) and advanced oxidation protein products (AOPP), both markers of oxidative stress, were found in subjects who experienced intermittent hypoxia caused by tracheal obstruction. Although the levels of MDA were not affected by the administration of antioxidants, AOPP levels were reduced considerably
[104][128]. Antioxidant properties are found in several medications commonly used to treat diseases other than OSA. N-acetylcysteine (NAC) is a well-known mucolytic drug that is used to treat acetaminophen overdose, is required for glutathione synthesis and has antioxidant properties. In a study involving patients with OSA, oral administration of NAC for 30 days caused a significant reduction in lipid peroxidation products and significantly increased glutathione levels
[100][124]. Currently, an ongoing clinical trial (NCT05009901) is examining the effect of using a powerful oral antioxidant (alpha lipoic acid, ALA) to treat patients with OSA by improving their cardiovascular health and reducing systemic inflammation and markers of oxidative stress. Another possible mechanism for the development of hypertension and consequent cardiovascular disease in patients with OSA is the activation of the renin-angiotensin-aldosterone system (RAAS). Meta-analyses of 13 studies assessing the role of OSA on RAAS components have reported higher plasma levels of angiotensin II in patients with OSA compared with controls and that patients with hypertension and OSA had higher aldosterone plasma levels compared with the controls
[105][129].
IH and reoxygenation may also contribute to the development of cardiovascular disease by promoting inflammation, which is strongly associated with endothelial dysfunction, atherosclerosis and coronary artery disease
[106][130]. Numerous animal and cell-based studies have pointed to a strong link between IH and vascular and systemic inflammation development. In mice, IH-induced atherosclerotic changes occurred with increased expression of proinflammatory cytokines, chemokines and adhesion molecules, increased migration of inflammatory cells and expansion of the macrophage population in the arterial wall
[30][35][107][31,36,131]. In addition, the aorta of mice exposed to IH had higher expression of the proinflammatory transcription factor NF-kB, although the levels of NF-kB returned to normal after recovering from normoxia
[31][108][32,132]. In humans, monocytes of patients with severe OSA showed elevated NLRP3 activity compared with monocytes from control subjects and this elevation showed a direct correlation with the AHI score and other hypoxemic indices
[109][57]. This report showed that higher NLRP3 activity triggered inflammatory cytokines, i.e., IL-1β and IL-18, via caspase-1 and increased Gasdermin D, which consequently allowed for tissue factor to be released. As a result, plasma concentrations of tissue factor were higher in patients with OSA and systemic inflammatory comorbidities compared with controls
[109][57]. In a prospective cohort study, the activation of NF-κB coincided with endothelial dysfunction and higher levels of its downstream targets were detected in endothelial cells of patients with OSA
[110][133]. In particular, the effects on endothelial function were reversed after four weeks of CPAP therapy
[111][134].