Depression and anxiety are high incidence and debilitating psychiatric disorders, usually treated by antidepressant or anxiolytic drug administration, respectively. Three main strategies have been used to improve brain drug targeting: the intranasal route of administration, which allows the drug to be directly transported to the brain by neuronal pathways, bypassing the blood–brain barrier and avoiding the hepatic and gastrointestinal metabolism; the use of nanosystems for drug encapsulation, including polymeric and lipidic nanoparticles, nanometric emulsions, and nanogels; and drug molecule functionalization by ligand attachment, such as peptides and polymers. Pharmacokinetic and pharmacodynamic in vivo studies’ results have shown that intranasal administration can be more efficient in brain targeting than other administration routes, and that the use of nanoformulations and drug functionalization can be quite advantageous in increasing brain–drug bioavailability. These strategies could be the key to future improved therapies for depressive and anxiety disorders.
1. Pathophysiology and Treatment of Depression and Anxiety Disorders: Current Aspects and Limitations
Anxiety is a central nervous system (CNS) disorder characterized by tension, restlessness, and increased effort to concentrate, with a persistent depressed mood and lack of interest in activities which pleasure was once taken from. It can consider the existence of several types of anxiety disorders, such as disorders related to separation, social anxiety, panic, specific phobias, and generalized anxiety disorder. These disorders generally begin in childhood, adolescence, or early adulthood. The general physiological mechanism by which these types of disorders arise is related to the γ-aminobutyric acid (GABA), which is inhibited and, hence, does not fulfill its role in the downregulation of neuronal excitability. It is estimated to affect millions of people worldwide, leading to a great loss in a person’s quality of life
[1][2][3][4][5][6][7][1,2,3,4,5,6,7].
In turn, depression is the biggest public health problem, making it a common mental disorder and one of the world’s leading causes of disability. In 2020, this disease affected about 16% of the world’s population
[8]. The etiology of depression has been related to stress. It is usually manifested by a loss of interest, feelings of guilt, depressed mood, sleep disturbance, low energy, and suicidal thoughts and attempts. There are several theories around the origin of depression, but the most accepted is the monoamine theory, which is related to a decrease in serotonin, noradrenaline, and dopamine levels in the CNS. It is caused by decreased excitability on the dopaminergic and/or serotonergic pathway. The markers of oxidative stress may also indicate depression, such as low levels of glutathione (GSH) and other antioxidants, and high levels of thiobarbituric acid (TBARS), F2 isoprostanes, inflammatory cytokines, and reactive oxygen species. Depression has also been associated with low levels of catalase, an enzyme responsible for the degradation of hydrogen peroxide into water and oxygen. In depressive situations, this enzyme is in deficit and, therefore, there is an accumulation of reactive oxygen species and consequently oxidative stress
[6][9][10][11][12][13][14][15][16][17][6,9,10,11,12,13,14,15,16,17].
Nowadays, oral and intravenous (IV) administrations are the most used in patients with depression or anxiety. However, for drugs whose target is the CNS, these routes have many disadvantages. The oral administration of central-acting drugs results in a low drug uptake by the brain and high drug distribution in the peripheral tissues. One of the main reasons for the failure of antidepressants and anxiolytics is the presence of the blood–brain barrier (BBB) and the existence of efflux pumps in the brain capillaries, endothelial cells, luminal membranes, and caveolae. As most antidepressant and anxiolytic drugs are substrates of these transporters, their brain bioavailability is limited, which causes a decrease in their effectiveness. Additionally, drugs that are administered orally can undergo chemical and metabolic degradation in the gastrointestinal tract, have drug–drug or food–drug interactions, have a slower therapeutic action which makes them non-adequate for emergency situations, and are only suitable for patients with the ability to swallow. On the other hand, the IV route is best in cases of emergency or when the patient is unable to swallow. However, it also has many disadvantages, such as invasiveness and the need for patient hospitalization, and difficulties in delivering the drug to the CNS due to the lack of penetration of the BBB
[12][14][18][19][20][21][12,14,18,19,20,21].
The BBB is a physical and metabolic barrier that limits the transport of substances between the blood and the neuronal tissue and is responsible for maintaining the physiological stability of the brain and protecting the CNS from toxic agents and microorganisms. It is made of three layers, but it is the innermost layer that poses a greater problem for drug delivery to the CNS. The BBB is essentially made up of endothelial cells in the capillary walls and tight junctions that prevent the transport of drugs through the paracellular pathway between adjacent endothelial cells in the inner layer. The BBB also has a biochemical layer with high levels of efflux transport proteins, such as P-glycoprotein (P-gp) and multidrug-resistant protein-1, as well as the expression of many metabolic enzymes, which limit brain-drug uptake
[22][23][22,23]. Despite all these limitations, small (molecular weight below 500 Da) and hydrophobic molecules, and some cells (such as monocytes, macrophages, and neutrophils) can be selectively transported to the brain
[21][22][23][24][25][21,22,23,24,25].
Additionally, although currently a lot of different treatment strategies exist, including pharmacological treatments, psychotherapies, and brain stimulation techniques, less than half of patients achieve a complete remission with the first treatment
[17][26][27][17,26,27]. For these reasons, several solutions have been studied to fight depression and anxiety in a more effective and safe way.
2. Potential Strategies for Enhancing Brain Drug Targeting and Bioavailability
2.1. Intranasal Administration
The nasal cavity has three main regions: the vestibular, respiratory, and olfactory regions. The vestibular region measures approximately 0.6 cm
2 and is located directly at the entrance of the nostrils. It contains nasal hairs (responsible for filtering inhaled particles), squamous epithelial cells, and some ciliated cells
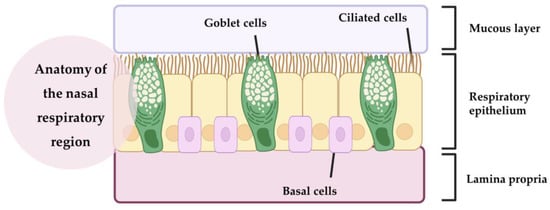
[28][29][30][31][28,29,30,31]. Next to it is the respiratory region (
Figure 1), which corresponds to the largest nasal area, at 150 cm
2 [21][28][21,28]. It is the most vascularized region with the greatest variety of cells, containing goblet, ciliated, non-ciliated, and basal cells
[28][31][32][28,31,32]. Goblet cells are responsible for secreting mucin, water, salts, a small group of proteins and lipids, and, together with some nasal glands, form the mucus layer. The mucus forms a layer in the respiratory epithelium and can trap inhaled molecules and send them to the pharynx, where they pass through to the gastrointestinal tract
[21][28][29][21,28,29]. Basal cells are the key cells of the nasal cavity and have the ability to differentiate into another type of epithelial cell, if necessary. These cells also help to attach the ciliated and goblet cells to the lamina propria
[21][29][21,29]. Ciliated cells, as the name suggests, have cilia that increase their surface area. They help to move the mucus toward the nasopharynx, resulting in mucociliary clearance
[21][32][21,32]. Together with a high degree of vascularization, this makes the nasal respiratory region a site of high drug transport into the systemic circulation. However, the respiratory region is also innervated by the maxillary and ophthalmic branches of the trigeminal nerve (V1, V2), which originate in the brainstem fossa and have been suggested as a possible target for drug transport to the CNS
[28][30][28,30].
Figure 1.
Anatomy of the nasal respiratory region (produced with BioRender).
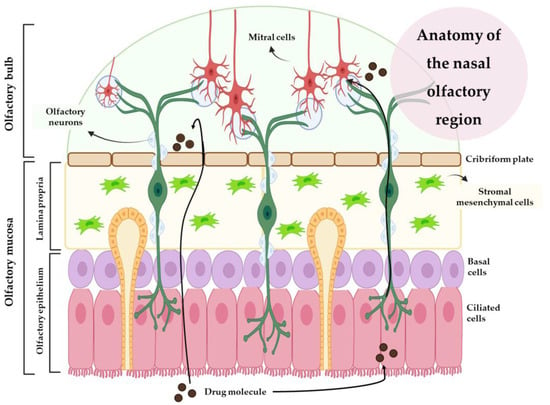
In turn, the olfactory region is made up of olfactory receptors, the olfactory epithelium, and lamina propria (
Figure 2). Olfactory receptors are unmyelinated neurons located in the nasal epithelium. In the lamina propria, each olfactory receptor forms thick bundles of axons that become olfactory nerves and innervate the cribriform plate, forming synaptic connections with the glomeruli of mitral cells in the olfactory bulb. There are two types of basal cells in this region: horizontal basal cells and spherical basal cells. In addition to horizontal basal cells, multipotent progenitor cells, and globular basal cells, this region also contains structural support cells that encase the olfactory receptors in the olfactory region, maintaining the structural integrity and ionization of the olfactory receptors. Drugs with small sizes can be transported through the axons, by the olfactory bulb, to the olfactory cortex, reaching the cerebellum
[21][32][33][21,32,33].
Figure 2.
Anatomy of the nasal olfactory region (produced with BioRender).
Nasal secretions are composed of approximately 95% water, 2% mucin, 1% salts, 1% other proteins (albumin, immunoglobulins, lysozymes, and lactoferrin), and <1% lipids. They move through the nose at a rate of approximately 5 to 6 mm/min, resulting in particles being cleared from the nose every 15 to 20 min. In addition, enzymes such as isoforms of the cytochrome P450 (CYP1A, CYP2A, and CYP2E), carboxylesterases, and glutathione S-transferases can also be found in the nasal cavity Therefore, the residence time of the formulation (and, consequently, the drug) in the nasal cavity will also be affected by these enzymes’ metabolism. To prolong the residence time of the formulation in the nasal cavity, and consequently increase the amount of drug that will be absorbed, biologically adhesive (mucoadhesive) excipients such as gelatin, chitosan, carbopol, and cellulose derivatives can be used
[28][34][28,34].
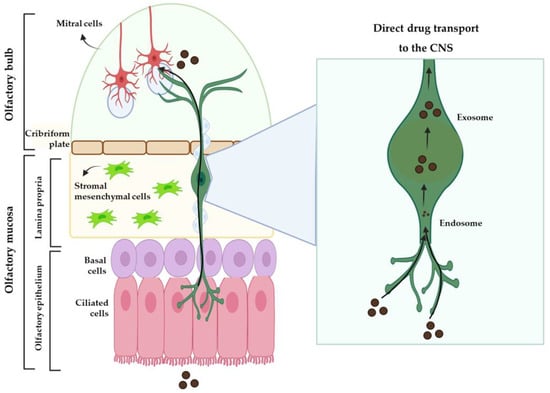
IV drug delivery to the brain is largely influenced by the drug’s plasma half-life, the extent of the metabolism, the degree of non-specific binding to plasma proteins, and the permeability of the compound across the BBB and into the peripheral tissues. Due to these issues, intranasal (IN) administration has been presented as a promising alternative to the IV route, having gained increasing interest over the past few years. After IN administration, the drug can take three different routes to the brain: one intracellular route and two extracellular routes (
Figure 2 and
Figure 3). The intracellular route is activated after drug endocytosis by the olfactory sensory cells, and the drug is consequently transported through the neuronal axon to the synaptic clefts in the olfactory bulb, where it is released through exocytosis. Drugs are delivered by endocytosis to the olfactory sensory neurons and peripheral trigeminal neurons, and then transported intracellularly from the olfactory sensory nerve to the olfactory bulb, and from the trigeminal nerve to the brainstem. This is an extremely slow pathway and it can take hours for the drug to reach the olfactory bulb
[28][33][35][36][28,33,35,36]. In the extracellular mechanism (
Figure 3), the drug can follow two different routes: it can cross the gaps between the olfactory neurons and then be transported to the olfactory bulb, or it can be transported along the trigeminal nerve to avoid the BBB. Once the drug has reached the olfactory bulb or the trigeminal region, it can be transported to other areas of the brain by diffusion, which is facilitated by a perivascular pump that is activated by arterial pulsation
[28][32][35][28,32,35].
Figure 3.
Extracellular mechanism of drug transport to the brain from the nasal cavity (produced with BioRender).
2.2. Nanosystems
The currently marketed nasal preparations exist mainly in the form of solutions or suspensions, but labile, poorly soluble, poorly permeable, and/or less potent drugs may require a formulation that promotes drug bioavailability and, preferably, direct delivery to the brain. To this end, nanotechnology has emerged to fill the existing gaps. All nanosystems are characterized by their small size, which makes them suitable for transporting drugs to the target tissues and cells, where they are ideally released
[20][37][38][20,37,38].
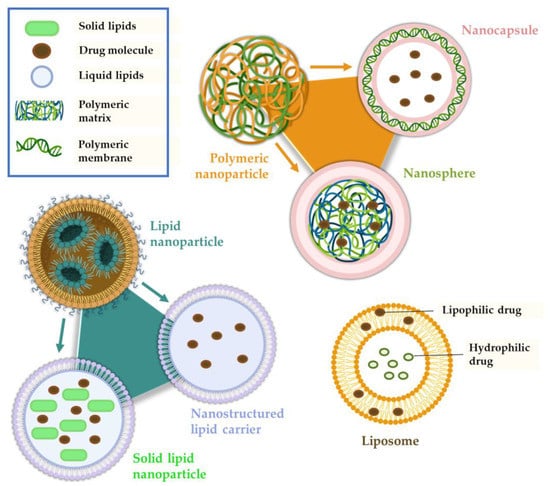
In terms of nanosystems that are meant to be administered by the IN route, these are designed to provide a longer residence time in the nasal cavity, overcome nasal mucociliary clearance, and facilitate rapid drug transport across the nasal mucosa. Independently of the intended administration route, there are several types of nanosystems (
Figure 4), with the main being: polymeric nanoparticles (NP), which are divided into nanocapsules and nanospheres; lipid nanoparticles, namely solid lipid nanoparticles and nanostructured lipid carriers; liposomes; nanometric emulsions, such as nanoemulsions and microemulsions; and nanoemulgels
[20][38][39][40][41][20,38,39,40,41].
Figure 4.
Main therapeutic nanosystem types (produced with BioRender).
Polymeric Nanoparticles
Polymeric nanoparticles are compact colloidal systems with a variable size range within the nanometric scale and can be composed of natural or synthetic polymers. They are composed of a dense core of polymeric matrix, suitable for encapsulating lipophilic drugs, and a hydrophilic crown that provides stability to the nanoparticles. The drug can be incorporated into the nanosystem in several ways: dissolved in the matrix, encapsulated within it, or adsorbed to it
[20][39][42][20,39,42].
There are two main types of polymeric NP: nanocapsules (a reservoir system) and nanospheres (a matrix system). Nanocapsules consist of an oily core in which the drug is dissolved, surrounded by a polymeric shell that controls the drug release from the core. Nanospheres are based on a continuous polymeric network, and in these systems the drug is either retained inside the nanosphere or adsorbed onto its surface. Although NP can be presented in a variety of ways, they have common characteristics that make them advantageous formulations, such as biocompatibility, biodegradability, high drug loading, the possibility of controlled drug release, and stability during storage
[43][44][45][43,44,45].
Several polymers can be used to produce NP for drug delivery. One of these is chitosan, a linear, natural, and biocompatible polysaccharide derived from the deacetylation of chitin from crustacean shells. It is a polymer that has some of the properties we need for effective and direct drug delivery to the brain, since it has the capacity to reduce mucociliary clearance and transiently opens tight junctions (protein kinase C pathway interaction), facilitating paracellular drug transport across the nasal mucosa to the brain
[21][35][36][46][21,35,36,46]. Chitosan is insoluble at neutral and basic pH values, but forms salts with inorganic or organic acids, such as hydrochloric acid and glutamic acid, which are soluble in water up to about pH 6.3 (depending on the molecular weight and deacetylation degree and, therefore, pKa). To further improve the mucoadhesive properties of chitosan, derivatives with thiol groups have been developed. These groups provide enhanced ciliary mucoadhesion, by forming covalent bonds between the polymer and the mucus layer that are stronger than non-covalent bonds
[21][35][47][21,35,47].
Another polymer of interest is alginic acid, a natural polysaccharide found in the cell walls of brown algae. Alginate (AG) is a derivative of alginic acid, and it is usually used in formulations in salt form (sodium or calcium). It is a hydrophilic polymer that, when in the presence of divalent cations, forms a gel that allows a controlled drug release
[21][46][48][21,46,48].
Poly lactic-co-glycolic acid (PLGA) is a synthetic polymer that is one of the most widely used polymers in controlled/directed drug delivery systems. This is due to its properties, such as biodegradability (hydrolysis to lactic acid and glycolic acid, which are metabolized by the body through the Krebs cycle), biocompatibility, and the ease of encapsulation of different types of drugs
[21][49][50][21,49,50].
Lipid Nanoparticles
We can consider two categories of lipid nanoparticles: solid lipid nanoparticles (SLN) and nanostructured lipid carriers (NLC). SLN are matrix nanoparticles made of solid lipids dispersed in water or an aqueous surfactant solution. They have high physical stability, no organic solvents used in their manufacture, good biocompatibility and tolerability, and also allow a controlled drug release and prolong the nasal retention time due to their occlusive effect and adhesion to the mucosa. Despite these advantages, SLN have some drawbacks. These include a limited ability to solubilize hydrophilic molecules, low drug encapsulation efficiency (due to their crystalline structure), possible drug expulsion during storage due to the crystallization process, and an undesirable increase in particle size by agglomeration, which can lead to an immediate and unwanted drug release
[33][36][42][33,36,42]. To improve some of these aspects, such as low stability, surfactants such as polyethylene glycol (PEG) can be used. PEG is a hydrophilic and biocompatible polymer that stabilizes nanoparticles and acts as a mucus penetration enhancer
[21][51][21,51].
In turn, instead of having only solid lipids in their composition, NLC have a mixture of solid and liquid lipids that form an imperfect crystalline matrix into which drugs can be incorporated. This imperfect matrix increases the drug-loading capacity of the system and minimizes/avoids its immediate and undesired release during storage, thus overcoming these disadvantages of SLN. NLC are biodegradable and generally composed of physiological lipids, and therefore have low toxicity to the body and good tolerability. With this nanosystem, it is possible to achieve a higher drug encapsulation efficiency (compared to SLN), as hydrophobic molecules have a higher solubility in liquid lipids than in solid lipids. Nevertheless, the solubilization capacity of hydrophilic drugs is still low, which is a drawback of NLC
[20][21][33][20,21,33].
Nanometric Emulsions
Regarding the nature of the external and internal phase(s), it can distinguish four types of nanometric emulsions: oil-in-water or water-in-oil (two phases) or oil-in-water-in-oil or water-in-oil-in-water (three phases). Oil-in-water nanometric emulsions, which are the most common, can solubilize and encapsulate hydrophobic drugs. A nanometric emulsion can improve drug stability and solubility and provide greater absorption due to the large surface area created by the small and numerous droplets
[40][42][52][40,42,52].
Nanometric emulsions can also be classified according to other characteristics in microemulsions or nanoemulsions. Microemulsions (ME) are isotropic and thermodynamically stable colloidal dispersions. They are generally composed of oil, water, and surfactants, and have droplet sizes between 10 and 100 nm. The IN administration of an oil-in-water ME may allow direct transport to the brain due to its small droplet size and lipophilic nature. In turn, nanoemulsions are also colloidal systems of nanometric size, with droplet sizes between 20 and 200 nm, but they are thermodynamically unstable, which can lead to poor stability and drug release during storage. Similar to microemulsions, they also have an oil phase, an aqueous phase, and a surfactant. However, the latter is usually present in smaller quantities
[21][38][41][21,38,41].
Nanogels
Nanogels are non-fluid colloidal or polymeric networks that increase their volume when in contact with a fluid, producing homogeneous solutions with low viscosity. These are defined as gel particles with a diameter of less than 100 nm. The use of nanogels is more effective than free drug administration (solution or other simple dispersion), since they have reported reduced toxicity, increased drug cellular uptake, high drug loading, and controlled drug release. This delivery system is effective for brain targeting as it leads to fast brain-drug absorption and has high biodegradability, biocompatibility, and hydrophilicity. It offers some advantages over other structures, such as the ability to encapsulate multiple molecules with different characteristics (both hydrophilic or hydrophobic) in the same formulation, leading to controlled drug release
[53][54][53,54].
Liposomes
Liposomes are biocompatible and biodegradable vesicles composed of layers of phospholipids and cholesterol, enclosing one or more aqueous compartments. They may be unilamellar (smaller size) or multilamellar (larger size). Liposomes can transport hydrophilic and hydrophobic molecules due to their structural properties: hydrophilic drugs can be stored in the aqueous nucleus, whereas hydrophobic molecules can be dissolved in the lipid membrane. They have an overall good permeation capacity, including through the nasal mucosa, and can protect drugs from enzymatic degradation. Nevertheless, immunogenicity is a problem that needs to be solved, along with low encapsulation efficiency, to reduce the need for frequent administration. Compared to bigger liposomes, the smaller ones (generally neutral or positively charged) have a longer circulation time. Additionally, unmodified liposomes have a short circulation time and, therefore, are rapidly cleared, via systemic circulation, by the smooth endoplasmic reticulum cells
[33][42][55][33,42,55].
Thus, to improve the circulation time of liposomes, modifications are made to their surface, such as coating them with PEG chains. In addition to PEG, it is common to use poloxamers, which are water-soluble, non-ionic polymers consisting of a triblock copolymer: a hydrophobic polypropylene glycol chain and two hydrophilic PEG chains. Suitable examples are poloxamer 407 and poloxamer 188, which have a high PEG content. Additionally, PEG reduces the viscosity of the nasal mucus and increases the penetration into the mucosa by interacting with lipid membranes and occlusion junctions, which is quite favorable for intranasal administration
[21][42][54][21,42,54].