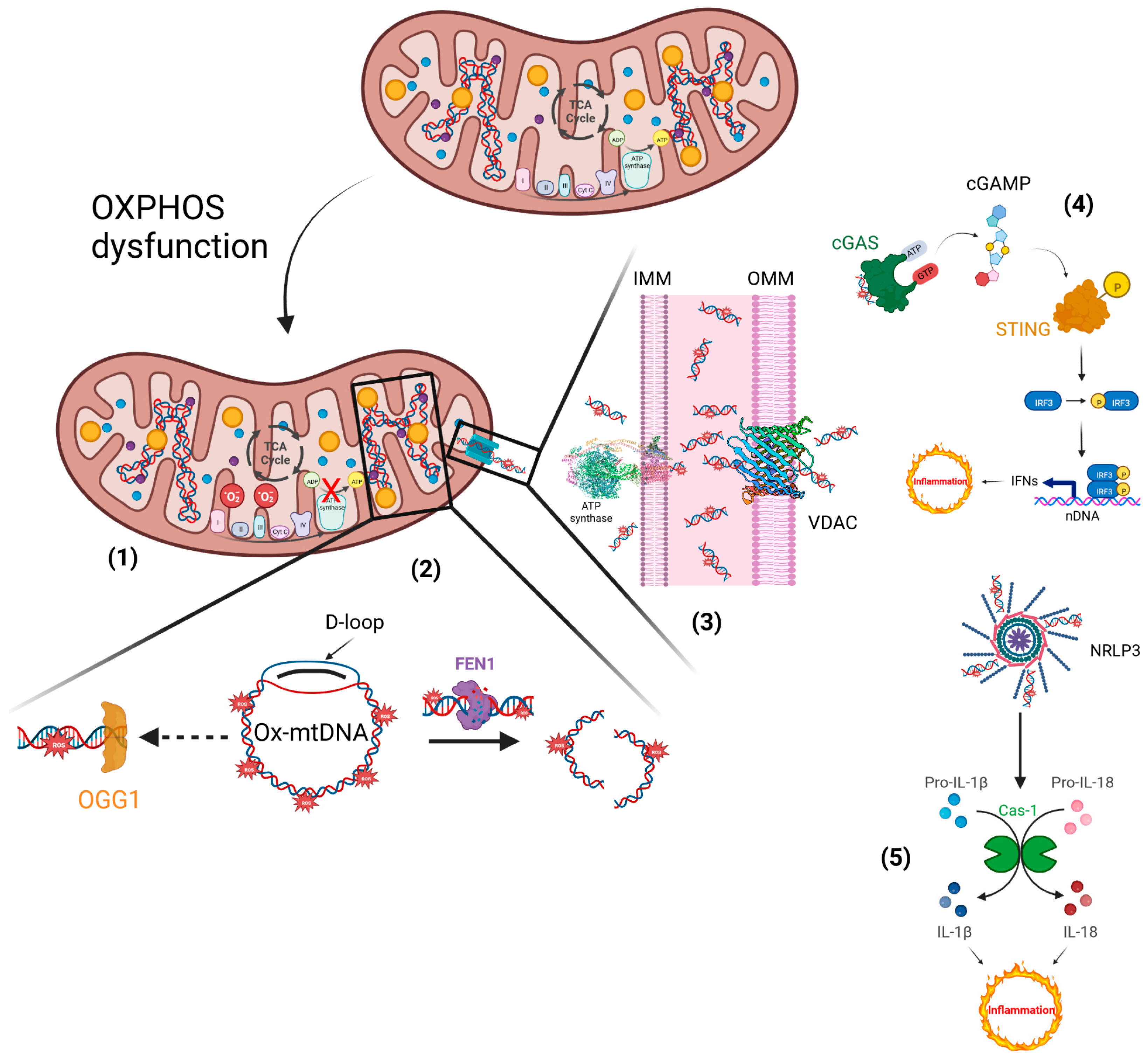
Human diseases are characterized by the perpetuation of an inflammatory condition in which the levels of Reactive Oxygen Species (ROS) are quite high. Excessive ROS production leads to DNA damage, protein carbonylation and lipid peroxidation, conditions that lead to a worsening of inflammatory disorders. In particular, compromised mitochondria sustain a stressful condition in the cell, such that mitochondrial dysfunctions become pathogenic, causing human disorders related to inflammatory reactions. Indeed, the triggered inflammation loses its beneficial properties and turns harmful if dysregulation and dysfunctions are not addressed. Thus, reducing oxidative stress with ROS scavenger compounds has proven to be a successful approach to reducing inflammation. Among these, natural compounds, in particular, polyphenols, alkaloids and coenzyme Q10, thanks to their antioxidant properties, are capable of inhibiting the activation of NF-κB and the expression of target genes, including those involved in inflammation.
- mitochondrial dysfunction
- reactive oxygen species
- inflammatory response
- cytokines
1. Introduction
2. Inflammation
The cellular biological response against aggression, caused by infectious and non-infectious agents (Gram-positive and Gram-negative bacteria, viruses, parasites, toxic substances, or irradiation), is defined as inflammation [2]. Therefore, as a result of an inflammatory process, there is a disruption of or damage to homeostatic processes at the cellular level. The inflammatory process can occur with acute and/or chronic inflammatory responses, thus, involving different organs (heart, liver, kidneys, brain, pancreas, lungs, intestines, etc.). All these events can potentially lead to tissue damage or disease, such as atherosclerosis, Type 2 diabetes, obesity, neurodegenerative diseases, dysbiosis and cancer [2,8][2][8].
However, the inflammatory process, if it occurs in a timely and complete manner, is of paramount importance, because it ensures the survival of the organism during an infection or injury [9]. Its main goals are to neutralize harmful stimuli, allow continued homeostasis of damaged tissues, and initiate the healing process [10]. At the tissue level, inflammation is characterized by five cardinal signs: redness, swelling, heat, pain, and tissue dysfunction (rubor, tumor, calor, dolor et functio laesa). The first four signs were clinically defined in the first century Atopic D ermatitis (AD) by a Roman physician, Cornelius Celsus. The fifth was added centuries later by Rudolph Virchow in 1858 [2]. Such signs then are nothing more than the macroscopic result of the local responses that occur during the inflammatory process (changes in vascular permeability, leukocyte recruitment and accumulation, and the release of inflammatory mediators) as a result of the triggering of a complex and coordinated communication between the different cells of the immune system (neutrophils, monocytes and lymphocytes) and the blood vessels [10]. Regardless of the nature of the stimulus and location in the body, different inflammatory processes all share common mechanisms, which have been extensively discussed and explored in the literature [11], and which are summarized in the text and Figure 1.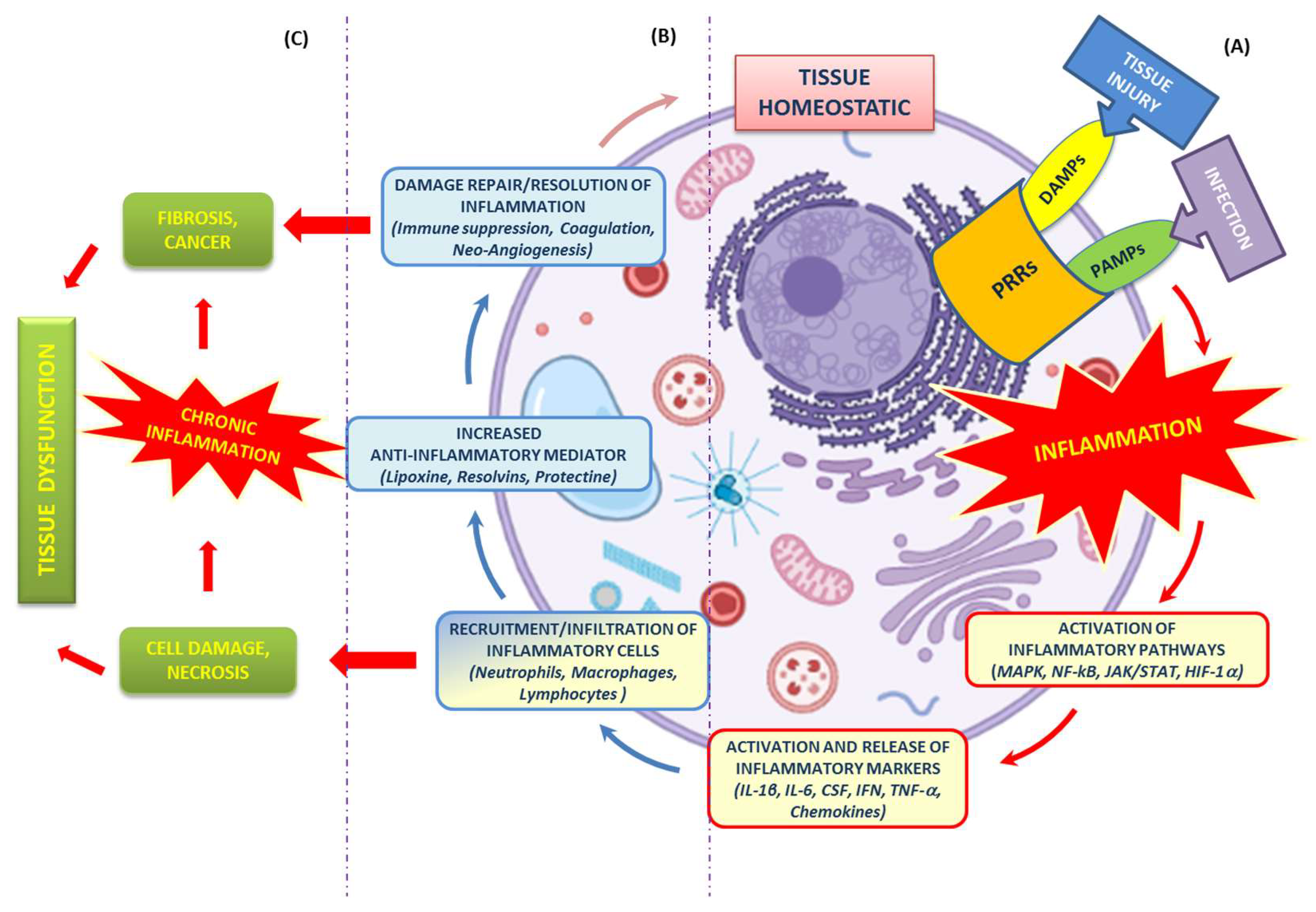
2.1. Recognition of Damaging Stimuli by Cell Surface Receptors: PRRs (Pattern Recognition Receptors)
-
Microbial structures, known as Pathogen Associated Molecular Patterns (PAMPs), expressed by pathogenic microbes [13];
-
Biomolecules, known as Damage-Associated Molecular Patterns (DAMPs), expressed by host cells during cell/tissue damage or cell death [14].
2.2. Activation of Inflammatory Pathways
2.3. Activation and Release of Inflammatory Markers
2.4. Recruitment of Inflammatory Cells
All cells involved in the inflammatory process are recruited to sites of tissue injury by factors released by damaged epithelial and endothelial cells, and trigger an inflammatory cascade, along with chemokines and growth factors. The first cells attracted to an injury site are neutrophils, followed by monocytes/macrophages, dendritic cells, lymphocytes, NK cells, T cells, B cells), and mast cells [34][22].2.5. Resolution of Inflammation
The process of resolution of inflammation is of fundamental importance, because it serves to limit both the development of further tissue damage and the onset of persistent chronic inflammation. The presence of mediators (lipoxin, resolvins, protectin, etc.) [36][23], even at this final stage of the inflammatory process, plays a key role, since their presence drives, both locally and systemically, a process of reduction in chemokine gradients over time.3. Mitochondrial Bioenergetics and Dysfunction
The mitochondria have always been considered the powerhouse of the cell. During aerobic metabolism, mitochondria are the primary source of ATP production. The chemiosmotic hypothesis explains the bioenergetic concept that governs the Oxidative Phosphorylation (OXPHOS) system in mitochondria [39,40][24][25] (Figure 2). OXPHOS activity relies on the inner mitochondrial membrane (IMM)-embedded enzyme (super)complexes [41][26]. As a key mechanism of energy production in cells, they are composed of respiratory machinery, which is responsible for substrate oxidation, working in concert towards the goal of producing ATP by the way of ADP phosphorylation. Mitochondrial respiration is sustained by the electron transfer chain (ETC) that drives the flow of electrons to the final acceptor, oxygen (O2), by four respiratory complexes. These are named as follows: NADH:ubiquinone oxidoreductase, or Complex I; succinate dehydrogenase, or Complex II; cytochrome bc1 oxidoreductase, or dimeric Complex III2; cytochrome c oxidase, or Complex IV. Moreover, to sustain the electron flow from NADH-dependent Complex I oxidation, or succinate-dependent Complex II oxidation, to O2-dependent Complex IV reduction, two mobile electron carriers complete the ETC, i.e., the membrane-embedded hydrophobic coenzyme Q10 (CoQ10) and the soluble cytochrome c. CoQ10 is the electron shuttle between either Complex I or Complex II and Complex III2, whereas cytochrome c facilitates the exchange of electrons from Complex III2 to Complex IV [42][27].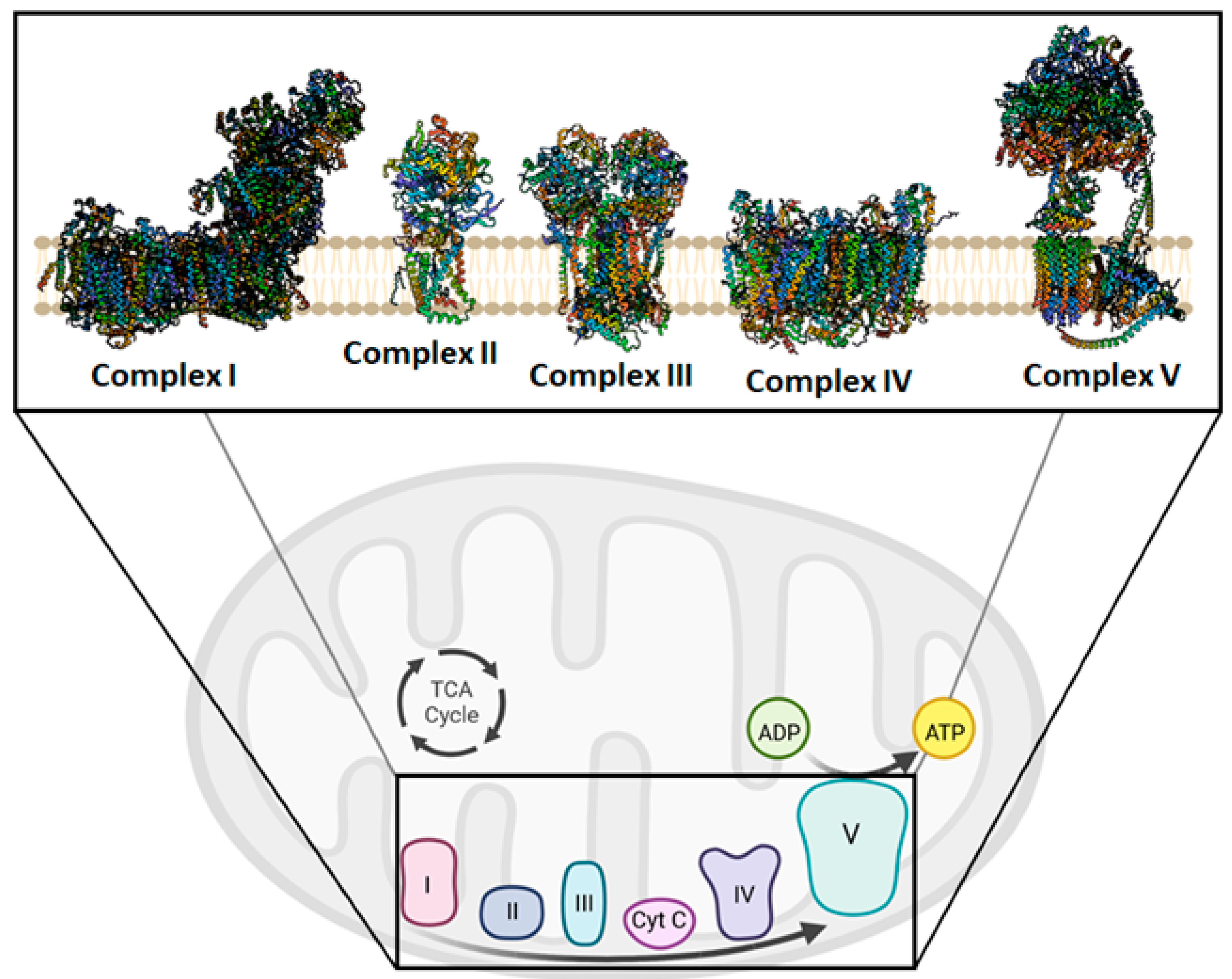
4. Mitochondria Are Potentially a New Target of Natural Compounds to Counteract Inflammation
5. Phytosome and Pathologies
5.1. Curcumin Phytosome
It is known that human exposure to Aluminum Chloride (AlCl3) causes hepatotoxicity, which can be counteracted by the Curcumin Phytosome (CP). Curcumin is a polyphenolic compound extracted from Curcuma longa. In studies conducted in rats, Al-Kahtani et al. demonstrated that treatment with AlCl3 increases the concentrations of Aspartate Aminotransferase (AST), Alanine Aminotransferase (ALT), Alkaline Phosphatase (ALP), Lactate dehydrogenase (LDH), total bilirubin, and Lipid Peroxidation (LPO), reducing, in addition, the stores of albumin, Reduced Glutathione (GSH), Superoxide Dismutase (SOD) and Glutathione Peroxidase (GPx). Histological lesions have also been reported. All of this results in an increased expression of caspase-3 and a decreased expression of Bcl-2. On the contrary, in the presence of CP, the endogenous antioxidant status is favored; therefore, caspase-3 expression is decreased and Bcl-2 expression increases, with an improvement in liver dysfunction [108][47]. The antioxidant and anti-inflammatory properties of curcumin and its nano-phytosome were also tested in mice that exhibited acute inflammation following the administration of carrageenan. In particular, the mice were treated, for 7 days, with an oral dose equal to 15 mg/Kg of indomethacin, curcumin and its nano-phytosome. After 7 days of treatment, the mice were administered carrageenan (1%) at the level of the subplantar region of the left paw, to induce the inflammatory process. A serum antioxidant enzyme assay found that carrageenan reduced the antioxidant activities of SOD, catalase (CAT), GPx, and glutathione reductase (GRx). Conversely, these activities increased in the presence of the curcumin nano-phytosome, both separately and in combination with indomethacin, demonstrating that curcumin nano-phytosome could enhance inflammatory-related antioxidant responses [109][48].5.2. Silybin Phytosome
Among the research related to the application of phytosomes, a very interesting study was conducted to improve the bioavailability of silybin, a natural compound known for its anticancer, antioxidant and hepatoprotective properties. Silybin is one of the main polyphenols found in silymarin, which is a complex of seven flavonolignans and polyphenols extracted from milk thistle (Silybum marianum). In particular, Chi et al. tested the phytosome-nanosuspensions formulation for silybin, defined as SPCs-NPs, in a mouse model of oxyhepatitis, induced by treatment with Carbon Tetrachloride (CCl4). CCl4 causes liver damage, following lipid peroxidation, a lower activity of antioxidant enzymes and increased generation of free radicals and ROS. The choice of silybin was dictated by the known properties of this natural compound, which is capable of protecting the liver from oxidative stress and inflammation, linked to ROS and secondary cytokine production. The CCl4-induced liver injury resulted in an increased presence of ALT, AST and ALP in the bloodstream, inducing centrilobular necrosis, ballooning degeneration and cellular infiltration. Only in the group of mice treated with SPCs-NPs was a significant reduction in ALT, AST and ALP levels recorded, while no significant changes in these parameters were reported in mice treated with silybin alone compared to the positive control.5.3. Quercetin Phytosome
An interesting flavanol for human health is quercetin, which cannot be produced by man, but is present in abundance in foods such as fruit, especially citrus fruits, green leafy vegetables, broccoli, olive oil, cherries, and blueberries. Similar to the other flavanols, however, quercetin has a low bioavailability, due to its poor solubility in water, even if it is quite soluble in alcohol and lipids. Therefore, the quercetin-loaded phytosome nanoparticles (QP) have made it possible to overcome this difficulty, increasing the bioavailability for humans of orally administered quercetin in this formulation by about 20 times. This turns out to be very interesting, given the known antiviral, anti-atopic, pro-metabolic, and anti-inflammatory properties of quercetin. Moreover, quercetin has a protective effect on mPTP opening [114][49].5.4. Berberine Phytosome
The efficacy of another natural product, such as berberine, was tested in women affected by Polycystic Ovary Syndrome (PCOS), an endocrine pathology characterized by hormonal imbalances, dysmetabolism and inflammation. In particular, berberine is an alkaloid used to fight infections, Type 2 diabetes and cancer, but also dyslipidemia in subjects intolerant to statins, and has been shown to enhance the expression of antioxidant enzyme activity. In the study, patients were treated with two daily oral doses of the Berberine Phytosome (BBR-PP) and evaluations were performed at baseline and after 60 days of treatment. The recorded data report a reduction in insulin resistance and acne, and an improvement in lipid metabolism and body composition, but also indicate a reduction in inflammation, with lower levels of CRP and TNF-α.5.5. Mulberry and Ginger Phytosome
Phytosomes have also been used in the treatment of Metabolic Syndrome (MetS), characterized by visceral adiposity, insulin resistance, hypertension, high triglyceride levels, and low High-Density Lipoprotein Cholesterol (HDL-C) levels. Patients with MetS have an increased risk of developing Type 2 Diabetes Mellitus (T2DM) and Atherosclerotic Cardiovascular Disease (ASCVD). Both genetic and acquired factors generate oxidative stress, cellular dysfunction and the systemic inflammation process responsible for the pathogenesis of MetS [120][50]. In particular, the phytosome containing the combined extracts of mulberry (Morus alba Linn. Var. Chiangmai) and ginger (Zingiber officinale Roscoe) (PMG) was tested in an animal model of MetS. Specifically, male Wistar rats were fed a high-carbohydrate, high-fat diet for 16 weeks, to induce MetS. In the following 21 days, rats with MetS signs were subjected to daily oral treatment with three different doses of PMG, equal to 50, 100 and 200 mg/Kg. Data analysis demonstrated that PMG has a positive effect on body weight gain, and lipid and glucose values, as well as improving Homeostasis Model Assessment of Insulin Resistance (HOMA-IR) and Angiotensin-Converting Enzyme (ACE) levels. Even the parameters relating to the density and size of the adipocytes, to the weight of the adipose tissue, have undergone an improvement after this treatment. At the adipose tissue level, PMG also reduced inflammatory cytokines such as IL-6 and TNF-α, as well as reducing oxidative stress and Histone Deacetylase 3 (HDAC3) expression, while simultaneously increasing PPAR-γ expression.5.5. Eufortyn
®
Colesterolo Plus
Recently, the ANEMONE study was conducted, involving 60 healthy subjects with moderate polygenic hypercholesterolemia, treated with Eufortyn® Colesterolo Plus. This nutraceutical consists of the standardized bergamot polyphenolic fraction phytosome (Vazguard®), as well as artichoke extract (Pycrinil®), artichoke dry extract (Cynara scolymus L.), zinc and CoQ10 phytosome (Ubiqosome®).5.7. Naringenin Phytosome
5.6. Naringenin Phytosome
Furthermore, a few years ago, Yu et al. studied the effect of Naringenin (NG) on acute lung injury. This is a respiratory pathology in which the lung undergoes an important inflammatory process. NG is a plant bioflavonoid found in citrus fruits such as bergamot, grapefruit, tangerine, known for its antioxidant, anti-inflammatory, antiproliferative and anticancer properties. In the study, rats with acute lung injury were treated with Dipalmitoylphosphatidylcholine (DPPC) phytosomes NG-loaded for dry powder inhalation (NPDPIs); in particular, NPDPIs, consisting of mannitol/DPPC/NG in a 4:2:1, w/w/w ratio, were found to be effective.5.8. Centella Asiatica Phytosome
5.7. Centella Asiatica Phytosome
In a mouse model of phthalic anhydride-induced Atopic Dermatitis (AD), the anti-inflammatory effect of the Centella Asiatica phytosome (CA phytosome) was investigated;it is a medicinal herb used in Ayurvedic, traditional African and Chinese medicine for the treatment of venous insufficiency of legs and diabetes wounds. Following the onset of AD, lesions on the dorsal skin and ear of mice were treated by applying the CA phytosome three times a week for 4 weeks. As a result, inhibition of hyperkeratosis, mast cell proliferation and inflammatory cell infiltration has been reported. The data obtained demonstrated that the CA phytosome inhibits the NF-κB signaling pathway, the release of TNF-α, IL-1β, and IgE, as well as inhibiting the expression of iNOS and COX-2 and the production of NO, resulting in it being a good treatment for AD [125][51].5.9. Leucoselect Phytosome
5.8. Leucoselect Phytosome
A few years ago, an open-label phase I lung cancer chemoprevention study was conducted on smokers and ex-smokers to test the chemoprotective effects of the leucoselect phytosome. This phytosome consisted of Grape Seed procyanidin Extract (GSE) complexed with soy phospholipids. At the end of the first month of treatment with leucoselect phytosome, an increase in the levels of omega-3 Polyunsaturated Fatty Acids (n-3 PUFAs) was reported, in particular of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), known for their anticancer properties. Three months after the start of the administration of the leucoselect phytosome, an increase in the serum levels of prostaglandin E3 (PGE3) was also recorded. The latter represents a metabolite of EPA, which, in addition to having antineoplastic properties, is also an anti-inflammatory molecule. Thus, the leucoselect phytosome represents a good chemopreventive agent for lung cancer [126][52].5.10. CoQ10 Phytosome
5.9. CoQ10 Phytosome
Moreover, in humans, the effect of CoQ10 deficiency is known. CoQ10 is a natural compound known for its antioxidant properties, its ability to prevent damage caused by free radicals, as well as its ability to inhibit inflammation signaling pathways. The CoQ10 deficiency can be of a primary or secondary form, and determines the onset of serious diseases, such as encephalomyopathy, cerebellar ataxia and cardiovascular disease. Therefore, maintaining correct concentrations of CoQ10 is important from a therapeutic point of view, even if it is very difficult to achieve this result given its high molecular weight, high lipophilicity, light sensitivity and thermolability [128][53]. To solve these problems, over the years, studies have been conducted on various formulations of CoQ10 that could increase its oral bioavailability. One such study is by Rizzardi et al., published in 2021. In this in vitro study, the authors evaluated the effects of the CoQ10 phytosomal formulation (UBIQSOME, UBQ) on the bioenergetic and antioxidant status of human intestinal epithelial cells (I407) and rat cardiomyoblasts (H9c2). In thise formulation, CoQ10 was administered in association with lecithin.5.11. Phytosomes and Cytotoxicity
5.10. Phytosomes and Cytotoxicity
Much evidence points to the efficacy of phytosomal formulations in increasing the cytotoxicity of certain natural compounds. Specifically, Alhakamy et al. conducted a study on treating ovarian cancer cells, OVCAR-3, with the phytosome Icariin (ICA). ICA is a flavonol glycoside found in Epimedium grandiflorum. It is best known for its efficacy in treating atherosclerosis and neurodegenerative disorders. It also possesses antioxidant, anti-inflammatory, cardioprotective and hepatoprotective activities. In addition, the antitumor activity of ICA has been demonstrated through its cytotoxicity, apoptotic activity, and regulation of cell cycle protein expression against different cell types. ICA also has anti-angiogenic, anti-metastatic, and immunomodulatory effects, explicitly enhancing the chemosensitivity of ovarian cancer cells. The limitation of ICA treatments is related to its pharmacokinetic properties; it has poor bioavailability due to its chemical structure and a short half-life when administered orally (3.15 h) and intravenously (0.56 h). Therefore, the phytosomal formulation seems to have many advantages for the cytotoxic efficacy of ICAs, particularly for ovarian cancer. This pathology represents a very serious and widespread gynecologic neoplasm worldwide, being fatal in most cases, as it has no early symptoms or adequate treatment. In the study by Alhakamy et al. an increase in the cytotoxic activity of the ICA phytosome on OVCAR-3 cells was demonstrated. Specifically, there was an increase in ICA phytosome-treated cells in the G2/M and pre-G1 phases of the cell cycle. Furthermore, Annexin V staining demonstrated an increase in early, late, and total apoptotic cells.References
- Serhan, C.N.; Savill, J. Resolution of inflammation: The beginning programs the end. Nat. Immunol. 2005, 6, 1191–1197.
- Medzhitov, R. Inflammation 2010: New Adventures of an Old Flame. Cell 2010, 140, 771–776.
- Nesci, S.; Lenaz, G. Impaired Mitochondrial Bioenergetics under Pathological Conditions. Life 2022, 12, 205.
- Marchi, S.; Guilbaud, E.; Tait, S.W.G.; Yamazaki, T.; Galluzzi, L. Mitochondrial control of inflammation. Nat. Rev. Immunol. 2022, 23, 159–173.
- Picard, M.; Wallace, D.C.; Burelle, Y. The rise of mitochondria in medicine. Mitochondrion 2016, 30, 105–116.
- Kotas, M.E.; Medzhitov, R. Homeostasis, Inflammation, and Disease Susceptibility. Cell 2015, 160, 816–827.
- Pérez-Torres, I.; Castrejón-Téllez, V.; Soto, M.E.; Rubio-Ruiz, M.E.; Manzano-Pech, L.; Guarner-Lans, V. Oxidative Stress, Plant Natural Antioxidants, and Obesity. Int. J. Mol. Sci. 2021, 22, 1786.
- Kunnumakkara, A.B.; Sailo, B.L.; Banik, K.; Harsha, C.; Prasad, S.; Gupta, S.C.; Bharti, A.C.; Aggarwal, B.B. Chronic diseases, inflammation, and spices: How are they linked? J. Transl. Med. 2018, 16, 14.
- Nathan, C.; Ding, A. Nonresolving Inflammation. Cell 2010, 140, 871–882.
- Kulkarni, O.P.; Lichtnekert, J.; Anders, H.-J.; Mulay, S.R. The Immune System in Tissue Environments Regaining Homeostasis after Injury: Is “Inflammation” Always Inflammation? Mediat. Inflamm. 2016, 2016, 2856213.
- Shen, H.; Kreisel, D.; Goldstein, D.R. Processes of Sterile Inflammation. J. Immunol. 2013, 191, 2857–2863.
- Li, D.; Wu, M. Pattern recognition receptors in health and diseases. Signal Transduct. Target. Ther. 2021, 6, 291.
- Eletto, D.; Mentucci, F.; Voli, A.; Petrella, A.; Porta, A.; Tosco, A. Helicobacter pylori Pathogen-Associated Molecular Patterns: Friends or Foes? Int. J. Mol. Sci. 2022, 23, 3531.
- Moriyama, K.; Nishida, O. Targeting Cytokines, Pathogen-Associated Molecular Patterns, and Damage-Associated Molecular Patterns in Sepsis via Blood Purification. Int. J. Mol. Sci. 2021, 22, 8882.
- Kaminska, B. MAPK signalling pathways as molecular targets for anti-inflammatory therapy—From molecular mechanisms to therapeutic benefits. Biochim. Biophys. Acta (BBA)-Proteins Proteom. 2005, 1754, 253–262.
- Huh, J.Y.; Park, Y.J.; Ham, M.; Kim, J.B. Crosstalk between Adipocytes and Immune Cells in Adipose Tissue Inflammation and Metabolic Dysregulation in Obesity. Mol. Cells 2014, 37, 365–371.
- Turner, M.D.; Nedjai, B.; Hurst, T.; Pennington, D.J. Cytokines and chemokines: At the crossroads of cell signalling and inflammatory disease. Biochim. Biophys. Acta (BBA)-Mol. Cell Res. 2014, 1843, 2563–2582.
- Conti, P.; Ronconi, G.; Caraffa, A.; Gallenga, C.E.; Ross, R.; Frydas, I.; Kritas, S.K. Induction of pro-inflammatory cytokines (IL-1 and IL-6) and lung inflammation by Coronavirus-19 (CoV-19 or SARS-CoV-2): Anti-inflammatory strategies. J. Biol. Regul. Homeost. Agents 2020, 34, 327–331.
- Ragab, D.; Salah Eldin, H.; Taeimah, M.; Khattab, R.; Salem, R. The COVID-19 Cytokine Storm; What We Know So Far. Front. Immunol. 2020, 11, 1446.
- Park, J.; Min, J.-S.; Kim, B.; Chae, U.-B.; Yun, J.W.; Choi, M.-S.; Kong, I.-K.; Chang, K.-T.; Lee, D.-S. Mitochondrial ROS govern the LPS-induced pro-inflammatory response in microglia cells by regulating MAPK and NF-κB pathways. Neurosci. Lett. 2015, 584, 191–196.
- Lopresti, A.L.; Maker, G.L.; Hood, S.D.; Drummond, P.D. A review of peripheral biomarkers in major depression: The potential of inflammatory and oxidative stress biomarkers. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2014, 48, 102–111.
- Stramer, B.M.; Mori, R.; Martin, P. The Inflammation–Fibrosis Link? A Jekyll and Hyde Role for Blood Cells during Wound Repair. J. Investig. Dermatol. 2007, 127, 1009–1017.
- Serhan, C.N.; Chiang, N.; Van Dyke, T.E. Resolving inflammation: Dual anti-inflammatory and pro-resolution lipid mediators. Nat. Rev. Immunol. 2008, 8, 349–361.
- Mitchell, P. Coupling of Phosphorylation to Electron and Hydrogen Transfer by a Chemi-Osmotic type of Mechanism. Nature 1961, 191, 144–148.
- Mitchell, P. Keilin’s Respiratory Chain Concept and Its Chemiosmotic Consequences. Science 1979, 206, 1148–1159.
- Vercellino, I.; Sazanov, L.A. The assembly, regulation and function of the mitochondrial respiratory chain. Nat. Rev. Mol. Cell Biol. 2021, 23, 141–161.
- Saraste, M. Oxidative Phosphorylation at the Fin de Siècle. Science 1999, 283, 1488–1493.
- Nesci, S.; Pagliarani, A.; Algieri, C.; Trombetti, F. Mitochondrial F-Type ATP Synthase: Multiple Enzyme Functions Revealed by the Membrane-Embedded FO Structure. Crit. Rev. Biochem. Mol. Biol. 2020, 55, 309–321.
- Rampelt, H.; Wollweber, F.; Licheva, M.; de Boer, R.; Perschil, I.; Steidle, L.; Becker, T.; Bohnert, M.; van der Klei, I.; Kraft, C.; et al. Dual role of Mic10 in mitochondrial cristae organization and ATP synthase-linked metabolic adaptation and respiratory growth. Cell Rep. 2022, 38, 110290.
- Blum, T.B.; Hahn, A.; Meier, T.; Davies, K.M.; Kühlbrandt, W. Dimers of mitochondrial ATP synthase induce membrane curvature and self-assemble into rows. Proc. Natl. Acad. Sci. USA 2019, 116, 4250–4255.
- Daum, B.; Walter, A.; Horst, A.; Osiewacz, H.D.; Kühlbrandt, W. Age-dependent dissociation of ATP synthase dimers and loss of inner-membrane cristae in mitochondria. Proc. Natl. Acad. Sci. USA 2013, 110, 15301–15306.
- Nesci, S.; Trombetti, F.; Pagliarani, A.; Ventrella, V.; Algieri, C.; Tioli, G.; Lenaz, G. Molecular and Supramolecular Structure of the Mitochondrial Oxidative Phosphorylation System: Implications for Pathology. Life 2021, 11, 242.
- Lenaz, G.; Strocchi, P. Reactive Oxygen Species in the Induction of Toxicity. In General, Applied and Systems Toxicology; American Cancer Society: Atlanta, GA, USA, 2011; ISBN 978-0-470-74430-7.
- Lenaz, G. Mitochondria and Reactive Oxygen Species. Which Role in Physiology and Pathology? Adv. Exp. Med. Biol. 2012, 942, 93–136.
- Kelley, N.; Jeltema, D.; Duan, Y.; He, Y. The NLRP3 Inflammasome: An Overview of Mechanisms of Activation and Regulation. Int. J. Mol. Sci. 2019, 20, 3328.
- Paik, S.; Kim, J.K.; Silwal, P.; Sasakawa, C.; Jo, E.-K. An update on the regulatory mechanisms of NLRP3 inflammasome activation. Cell. Mol. Immunol. 2021, 18, 1141–1160.
- Huang, L.S.; Hong, Z.; Wu, W.; Xiong, S.; Zhong, M.; Gao, X.; Rehman, J.; Malik, A.B. mtDNA Activates cGAS Signaling and Suppresses the YAP-Mediated Endothelial Cell Proliferation Program to Promote Inflammatory Injury. Immunity 2020, 52, 475–486.e5.
- Wu, Z.; Sainz, A.G.; Shadel, G.S. Mitochondrial DNA: Cellular genotoxic stress sentinel. Trends Biochem. Sci. 2021, 46, 812–821.
- Algieri, C.; Bernardini, C.; Oppedisano, F.; La Mantia, D.; Trombetti, F.; Palma, E.; Forni, M.; Mollace, V.; Romeo, G.; Troisio, I.; et al. The Impairment of Cell Metabolism by Cardiovascular Toxicity of Doxorubicin Is Reversed by Bergamot Polyphenolic Fraction Treatment in Endothelial Cells. Int. J. Mol. Sci. 2022, 23, 8977.
- Wang, Y.; Yang, J.; Yi, J.; Olguín-Albuerne, M.; Morán, J.; Hornsveld, M.; Dansen, T.B.; Genova, M.L.; Lenaz, G.; Nunes, P.; et al. Redox Sensing by Proteins: Oxidative Modifications on Cysteines and the Consequent Events. Antioxid. Redox Signal. 2012, 16, 649–657.
- Cheng, K.C.; Cahill, D.S.; Kasai, H.; Nishimura, S.; Loeb, L.A. 8-Hydroxyguanine, an abundant form of oxidative DNA damage, causes G-T and A-C substitutions. J. Biol. Chem. 1992, 267, 166–172.
- Russo, M.T.; De Luca, G.; Degan, P.; Parlanti, E.; Dogliotti, E.; Barnes, D.E.; Lindahl, T.; Yang, H.; Miller, J.H.; Bignami, M. Accumulation of the Oxidative Base Lesion 8-Hydroxyguanine in DNA of Tumor-Prone Mice Defective in Both the Myh and Ogg1 DNA Glycosylases. Cancer Res. 2004, 64, 4411–4414.
- Rakha, A.; Umar, N.; Rabail, R.; Butt, M.S.; Kieliszek, M.; Hassoun, A.; Aadil, R.M. Anti-inflammatory and anti-allergic potential of dietary flavonoids: A review. Biomed. Pharmacother. 2022, 156, 113945.
- Wang, Y.; Ning, X.; Gao, P.; Wu, S.; Sha, M.; Lv, M.; Zhou, X.; Gao, J.; Fang, R.; Meng, G.; et al. Inflammasome Activation Triggers Caspase-1-Mediated Cleavage of cGAS to Regulate Responses to DNA Virus Infection. Immunity 2017, 46, 393–404.
- Xian, H.; Watari, K.; Sanchez-Lopez, E.; Offenberger, J.; Onyuru, J.; Sampath, H.; Ying, W.; Hoffman, H.M.; Shadel, G.S.; Karin, M. Oxidized DNA fragments exit mitochondria via mPTP- and VDAC-dependent channels to activate NLRP3 inflammasome and interferon signaling. Immunity 2022, 55, 1370–1385.e8.
- Kim, J.; Gupta, R.; Blanco, L.P.; Yang, S.; Shteinfer-Kuzmine, A.; Wang, K.; Zhu, J.; Yoon, H.E.; Wang, X.; Kerkhofs, M.; et al. VDAC oligomers form mitochondrial pores to release mtDNA fragments and promote lupus-like disease. Science 2019, 366, 1531–1536.
- Al-Kahtani, M.; Abdel-Daim, M.M.; Sayed, A.A.; El-Kott, A.; Morsy, K. Curcumin phytosome modulates aluminum-induced hepatotoxicity via regulation of antioxidant, Bcl-2, and caspase-3 in rats. Environ. Sci. Pollut. Res. 2020, 27, 21977–21985.
- Baradaran, S.; Hajizadeh Moghaddam, A.; Khanjani Jelodar, S.; Moradi-Kor, N. Protective Effects of Curcumin and its Nano-Phytosome on Carrageenan-Induced Inflammation in Mice Model: Behavioral and Biochemical Responses. J. Inflamm. Res. 2020, 13, 45–51.
- Algieri, C.; Trombetti, F.; Pagliarani, A.; Ventrella, V.; Bernardini, C.; Fabbri, M.; Forni, M.; Nesci, S. Mitochondrial Ca2+-activated F1FO-ATPase hydrolyzes ATP and promotes the permeability transition pore. Ann. N. Y. Acad. Sci. 2019, 1457, 142–157.
- Carresi, C.; Gliozzi, M.; Musolino, V.; Scicchitano, M.; Scarano, F.; Bosco, F.; Nucera, S.; Maiuolo, J.; Macrì, R.; Ruga, S.; et al. The Effect of Natural Antioxidants in the Development of Metabolic Syndrome: Focus on Bergamot Polyphenolic Fraction. Nutrients 2020, 12, 1504.
- Ho, P.J.; Sung, J.J.; Cheon, K.K.; Tae, H.J. Anti-inflammatory effect of Centella asiatica phytosome in a mouse model of phthalic anhydride-induced atopic dermatitis. Phytomedicine 2018, 43, 110–119.
- Mao, J.T.; Xue, B.; Fan, S.; Neis, P.; Qualls, C.; Massie, L.; Fiehn, O. Leucoselect Phytosome Modulates Serum Eicosapentaenoic Acid, Docosahexaenoic Acid, and Prostaglandin E3 in a Phase I Lung Cancer Chemoprevention Study. Cancer Prev. Res. 2021, 14, 619–626.
- Cicero, A.F.G.; Fogacci, F.; Di Micoli, A.; Veronesi, M.; Borghi, C. Noninvasive instrumental evaluation of coenzyme Q10 phytosome on endothelial reactivity in healthy nonsmoking young volunteers: A double-blind, randomized, placebo-controlled crossover clinical trial. Biofactors 2022, 48, 1160–1165.
