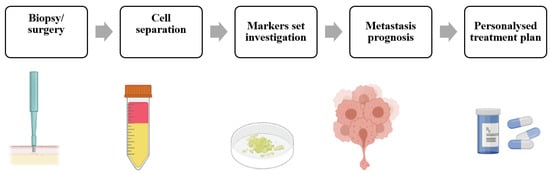
The major cause (more than 90%) of all cancer-related deaths is metastasis, thus its prediction can critically affect the survival rate. Metastases are predicted by lymph-node status, tumor size, histopathology and genetic testing. The identification of new potential prognostic factors will be an important source of risk information for the practicing oncologist, potentially leading to enhanced patient care through the proactive optimization of treatment strategies. Mechanobiology, as a branch of biomechanics and/or a branch of biology, has reached a mature stage mainly because of the significant technological and methodological advances at the cellular, subcellular, and molecular levels and the need to disclose the mechanical basis of biology. The application of mechanobiology to medicine (mechanomedicine) may help advance human health and improve diagnostics, treatment, and therapeutics of cancer.
Over the last few decades, mechanobiology, as a branch of biomechanics and/or a branch of biology, has reached a mature stage mainly because of the significant technological and methodological advances at the cellular, subcellular, and molecular levels and the need to disclose the mechanical basis of biology. The application of mechanobiology to medicine (mechanomedicine) may help advance human health and improve diagnostics, treatment, and therapeutics of cancer.
- cancer
- metastasis
- endocytosis
- mechanobiology
- mechanomedicine
- tumor cell softness/deformability
- extracellular matrix stiffness
- fluid shear stress
- cytoskeletal/intermediate filament stress
- extracellular vesicles
1. A Need for Identification of New Potential Prognostic Markers
2. Tumor Biomarkers
3. Mechanobiology of Metastasis
Altered mechanotype is an emerging hallmark of cancer cells that is linked to invasive phenotype and treatment resistance. Mechanotype also influences crosstalk between tumor cells and their environment and may thus have a critical role in cancer progression. Tumor cell mechanotype appears to relate to invasive status [26][27][28]. Demonstration that the invasive potential of cells correlates with their deformability, where softer or more deformable cells are more invasive, sounds plausible, since more deformable cells can move more easily through tight gaps, which could assist their escape from a primary tumor and invasion into surrounding ECM [26][28]. In vitro experiments have shown that malignant cancer cells are softer than benign cells. This can be shown through experiments on human cell lines derived from various tissues using different mechanotyping methods. Atomic force microscopy [29][30], deformability cytometry [31] and parallel microfiltration [27] are among the mostly widely used. Many of these methods measure the displacement or change in shape of a cell or protein network. Atomic force microscopy is used to measure the viscoelastic properties of a single cell or protein network with displacements down to 1 nm. Other methods can probe mechanical properties over length scales of 1–10 um, such as magnetic twisting cytometry and micropipette aspiration. The deformability of whole cells can also be measured by forcing cells to pass through smaller pores than cell size. As such, the parallel microfiltration method, where air pressure forces a cell suspension to pass through a porous membrane, can measure the relative deformability of different cell samples [27]. Microfluidic deformability cytometry measures whole-cell deformability by applying stretching extensional flow to single cells [31]. Active forces generated by the cell can be probed by traction force microscopy, where displacements of the substrate that result from contractile forces of the cell are measured. Cell deformability is associated with the aggressiveness of tumor cells. Indeed, overexpression of key epithelial-to-mesenchymal transition transcription factors (Snail, Slug and Zeb1) makes ovarian cancer cells softer [27]. Human MCF-7 cells are more deformable than their non-malignant mammary epithelial counterparts, MCF-10 cells. Metastatic MCF-7 (modMCF-7) cells are even more deformable than the less-invasive MCF-7 cells [26]. Human lung adenocarcinoma cells with greater metastatic potential are also more deformable than their less-metastatic counterparts [28]. Human bladder epithelial cancer cells are more deformable than normal cells [32]. Similarly, transformed fibroblasts are significantly more deformable than normal untransformed fibroblasts [26][33]. Taken together, malignant cells across various types of cancers are more deformable than normal cells. Moreover, more-invasive tumor cells are softer or more tissue-compliant than less-invasive ones. It is a complex and challenging task to understand the molecular roots of malignant cells’ altered mechanotypes. Mechanotypes can change through multiple factors including proteins, signaling pathways and other factors. Changes to cytoskeleton network structure and organization can alter cell differentiation or deformability. Such structural changes are also linked to malignant phenotypes. Higher grade colon and ovarian cancer cells have more actin and microtubule content than lower grade cancer cells [34][35]. Differences in the cytoskeletal architecture are also involved in variations in the deformability of melanoma cells; these structural alterations are associated with in vivo metastatic potential in mouse models [36]. However, the cytoskeleton changes in a cancer cell do not always correlate with the softer mechanotype. Even though softer mesenchymal-type ovarian cancer cells are often found less readily than their epithelial-type counterparts, there is no uniform pattern of actin distribution or microtubule organization that can explain the softer mechanotype [27]. Thus, the cell mechanotype provides unique information about the malignant status of a cell, being a good candidate for a physical biomarker of malignancy. Metastatic invasion through tissue is a critical step in metastases formation. The most widely used measure of cancer aggressiveness is cell invasiveness, or the ability of a cell to invade its surroundings. Migration is often used to describe any directed cell movement within the body, while invasion is defined as the penetration of tissue barriers [37]. In vitro methods enable the study of confined cell migration in environments of known physical and chemical composition [38]. A simple method for the migration measurement of single cells is colloidal gold particle-coated surfaces, with areas of clearing in the gold-colloid corresponding to phagokinetic cell tracks [39][40]. Microfluidic and nanofluidic assays, with relatively rigid or compliant channels fabricated from silicon or poly(dimethyl siloxane) (PDMS), were also employed to simulate the flow of single cells through blood or lymph vessels [41][42] or transition effects across mechanical barriers [43]. The enhanced pliability of the metastatic cancer cells facilitates their migration through small pores, as was evaluated by in vitro Boyden chamber migration/invasion experiments [44][45]. Boyden chambers were previously evaluated as a commonly employed migration assay that measures the capacity of cell motility and invasiveness toward a chemo-attractant gradient through a porous matrix [45][46]. However, the experiments last at least 24h and there is dependence on Matrigel batches: for example, it was found that in the same experiment MDA-MB-231 cells seeded on two different batches of Matrigel resulted in, respectively, 23 ± 2% and 15 ± 2% invasion [47]. It was previously shown by example of Boyden chambers (matrix membranes with different mesh sizes), that the structure and mechanics of cancer cells are linked directly to their metastatic potential [44][45]. However, the results are affected by the thickness and composition of membranes, and the invasion capacity of cells with different phenotypes cannot be universally correlated to metastatic potential [47]. Therefore, before each experiment, the chosen standard should be checked. There are some complex 3D invasion gel assays for in vitro invasion; they usually utilize a degradable collagen [48] or gelatin [49][50] matrix and most faithfully mimic the situation in vivo, however, they require complex equipment such as a confocal microscope or fixation and sectioning [37]. The novel, mechanobiology-based, simple 2D gel-invasion assay provides relatively fast (one day), quantitative results, with very high accuracy [51][52][53]. Recently, rwesearchers have shown the direct connection of the ability of metastatic cells to invade with their propensity to endocytosis, and have linked the efficiency of short-time (1 h) encapsulation of nanoparticles to the metastatic potential [54][55]. However, those approaches are still far away from clinical implementation, due to the required manipulations for cancer cell extraction from tumor samples. The definition of specific protein markers, reflecting the direct mechanobiological properties of cancer cells (i.e., invasive and migration properties), will allow the detection of metastatic potential with no need for intact cell extraction from the tumor sample, and therefore will provide an important input in the prognosis of metastasis [56]. The scope of current Entry will be to expand the current knowledge and advances in understanding the impact of forces and mechanics on functions and fate of cancer stem cells. The pathways of mechanotransduction in tumor and tumor microenvironment cells are also at interest. Approaches for treating patients using mechanobiology-derived strategies are just emerging. The mechanomedicine, including mechanobiology-based tools and strategies needed for diagnosing and treating patients. It can be developed by outside-the-box thinking that is supposed to best come in theour Entry.References
- Yang, J.; Weinberg, R.A. Epithelial-Mesenchymal Transition: At the Crossroads of Development and Tumor Metastasis. Dev. Cell 2008, 14, 818–829.
- Sleeman, J.P.; Nazarenko, I.; Thiele, W. Do All Roads Lead to Rome? Routes to Metastasis Development. Int. J. Cancer 2011, 128, 2511–2526.
- Cairns, R.A.; Khokha, R.; Hill, R.P. Molecular Mechanisms of Tumor Invasion and Metastasis: An Integrated View. Curr. Mol. Med. 2003, 3, 659–671.
- Weigelt, B.; Peterse, J.L.; van ’t Veer, L.J. Breast Cancer Metastasis: Markers and Models. Nat. Rev. Cancer 2005, 5, 591–602.
- Riihimaki, M.; Thomsen, H.; Hemminki, A.; Sundquist, K.; Hemminki, K.; Riihimäki, M.; Thomsen, H.; Hemminki, A.; Sundquist, K.; Hemminki, K.; et al. Comparison of Survival of Patients with Metastases from Known versus Unknown Primaries: Survival in Metastatic Cancer. BMC Cancer 2013, 13, 36.
- Lynch, J.A.; Venne, V.; Berse, B. Genetic Tests to Identify Risk for Breast Cancer. Semin. Oncol. Nurs. 2015, 31, 100–107.
- Vaidyanathan, K.; Vasudevan, D.M. Organ Specific Tumor Markers: What’s New? Indian J Clin Biochem 2012, 27, 110–120.
- Gurcan, M.N.; Boucheron, L.E.; Can, A.; Madabhushi, A.; Rajpoot, N.M.; Yener, B. Histopathological Image Analysis: A Review. IEEE Rev. Biomed. Eng. 2009, 2, 147–171.
- Wei, J.W.; Tafe, L.J.; Linnik, Y.A.; Vaickus, L.J.; Tomita, N.; Hassanpour, S. Pathologist-Level Classification of Histologic Patterns on Resected Lung Adenocarcinoma Slides with Deep Neural Networks. Sci. Rep. 2019, 9, 3358.
- Lang, E.V.; Berbaum, K.S.; Lutgendorf, S.K. Large-Core Breast Biopsy: Abnormal Salivary Cortisol Profiles Associated with Uncertainty of Diagnosis. Radiology 2009, 250, 631–637.
- Yankaskas, C.L.; Thompson, K.N.; Paul, C.D.; Vitolo, M.I.; Mistriotis, P.; Mahendra, A.; Bajpai, V.K.; Shea, D.J.; Manto, K.M.; Chai, A.C.; et al. A Microfluidic Assay for the Quantification of the Metastatic Propensity of Breast Cancer Specimens. Nat. Biomed. Eng. 2019, 3, 452–465.
- Murugan, A.K. MTOR: Role in Cancer, Metastasis and Drug Resistance. Semin. Cancer Biol. 2019, 59, 92–111.
- Wu, L.; Qu, X. Cancer Biomarker Detection: Recent Achievements and Challenges. Chem. Soc. Rev. 2015, 44, 2963–2997.
- Narayan Bhatt, A.; Farooque, A.; Verma, A. Cancer Biomarkers-Current Perspectives Role of Tumor Microenvironment in Treatment of Lymphoma and Myeloma View Project Metabolic Signaling Approaches for Anticancer Drug Target Discovery View Project. Artic. Indian J. Med. Res. 2010, 132, 129–149.
- Wang, F.; Fang, Q.; Ge, Z.; Yu, N.; Xu, S.; Fan, X. Common BRCA1 and BRCA2 Mutations in Breast Cancer Families: A Meta-Analysis from Systematic Review. Mol. Biol. Rep. 2012, 39, 2109–2118.
- De, P.; Mukhopadhyay, M.J. Study of the Chromosomal Abnormalities and Associated Complex Karyotypes in Hematological Cancer in the Population of West Bengal: A Prospective Observational Study. Indian J. Med. Paediatr. Oncol. 2021, 42, 261–267.
- Wang, C.; Bai, F.; Zhang, L.Z.; Scott, A.; Li, E.; Pei, X.H. Estrogen Promotes Estrogen Receptor Negative BRCA1-Deficient Tumor Initiation and Progression. Breast Cancer Res. 2018, 20, 74.
- Huang, J.; Duran, A.; Reina-Campos, M.; Valencia, T.; Castilla, E.A.; Müller, T.D.; Tschöp, M.H.; Moscat, J.; Diaz-Meco, M.T. Adipocyte P62/SQSTM1 Suppresses Tumorigenesis through Opposite Regulations of Metabolism in Adipose Tissue and Tumor. Cancer Cell 2018, 33, 770–784.e6.
- Szablewski, L. Glucose Transporters as Markers of Diagnosis and Prognosis in Cancer Diseases. Oncol. Rev. 2022, 16, 561.
- Pouliquen, D.; Boissard, A.; Coqueret, O.; Guette, C. Biomarkers of Tumor Invasiveness in Proteomics (Review). Int. J. Oncol. 2020, 57, 409–432.
- Wilt, T.J.; Scardino, P.T.; Carlsson, S.V.; Basch, E. Prostate-Specific Antigen Screening in Prostate Cancer: Perspectives on the Evidence. J. Natl. Cancer Inst. 2014, 106, 10.
- Brufsky, A.M.; Mayer, M.; Rugo, H.S.; Kaufman, P.A.; Tan-Chiu, E.; Tripathy, D.; Tudor, I.C.; Wang, L.I.; Brammer, M.G.; Shing, M.; et al. Central Nervous System Metastases in Patients with HER2-Positive Metastatic Breast Cancer: Incidence, Treatment, and Survival in Patients from RegistHER. Clin. Cancer Res. 2011, 17, 4834–4843.
- Kuba, S.; Ishida, M.; Nakamura, Y.; Yamanouchi, K.; Minami, S.; Taguchi, K.; Eguchi, S.; Ohno, S. Treatment and Prognosis of Breast Cancer Patients with Brain Metastases According to Intrinsic Subtype. Jpn. J. Clin. Oncol. 2014, 44, 1025–1031.
- Molinie, N.; Rubtsova, S.N.; Fokin, A.; Visweshwaran, S.P.; Rocques, N.; Polesskaya, A.; Schnitzler, A.; Vacher, S.; Denisov, E.V.; Tashireva, L.A.; et al. Cortical Branched Actin Determines Cell Cycle Progression. Cell Res. 2019, 29, 432–445.
- Geiger, T.; Cox, J.; Mann, M. Proteomic Changes Resulting from Gene Copy Number Variations in Cancer Cells. PLoS Genet. 2010, 6, e1001090.
- Guck, J.; Schinkinger, S.; Lincoln, B.; Wottawah, F.; Ebert, S.; Romeyke, M.; Lenz, D.; Erickson, H.M.; Ananthakrishnan, R.; Mitchell, D.; et al. Optical Deformability as an Inherent Cell Marker for Testing Malignant Transformation and Metastatic Competence. Biophys. J. 2005, 88, 3689–3698.
- Qi, D.; Gill, N.K.; Santiskulvong, C.; Sifuentes, J.; Dorigo, O.; Rao, J.; Taylor-Harding, B.; Wiedemeyer, W.R.; Rowat, A.C. Screening Cell Mechanotype by Parallel Microfiltration. Sci. Rep. 2015, 5, 17595.
- Byun, S.; Son, S.; Amodei, D.; Cermak, N.; Shaw, J.; Kang, J.H.; Hecht, V.C.; Winslow, M.M.; Jacks, T.; Mallick, P.; et al. Characterizing Deformability and Surface Friction of Cancer Cells. Proc. Natl. Acad. Sci. USA 2013, 110, 7580–7585.
- Paszek, M.J.; Zahir, N.; Johnson, K.R.; Lakins, J.N.; Rozenberg, G.I.; Gefen, A.; Reinhart-King, C.A.; Margulies, S.S.; Dembo, M.; Boettiger, D.; et al. Tensional Homeostasis and the Malignant Phenotype. Cancer Cell 2005, 8, 241–254.
- Guck, J.; Ananthakrishnan, R.; Mahmood, H.; Moon, T.J.; Cunningham, C.C.; Käs, J. The Optical Stretcher: A Novel Laser Tool to Micromanipulate Cells. Biophys. J. 2001, 81, 767.
- Gossett, D.R.; Tse, H.T.K.; Lee, S.A.; Ying, Y.; Lindgren, A.G.; Yang, O.O.; Rao, J.; Clark, A.T.; Di Carlo, D. Hydrodynamic Stretching of Single Cells for Large Population Mechanical Phenotyping. Proc. Natl. Acad. Sci. USA 2012, 109, 7630–7635.
- Lekka, M.; Laidler, P.; Gil, D.; Lekki, J.; Stachura, Z.; Hrynkiewicz, A.Z. Elasticity of Normal and Cancerous Human Bladder Cells Studied by Scanning Force Microscopy. Eur. Biophys. J. 1999, 28, 312–316.
- Mak, M.; Spill, F.; Kamm, R.D.; Zaman, M.H. Single-Cell Migration in Complex Microenvironments: Mechanics and Signaling Dynamics. J. Biomech. Eng. 2016, 138, 021004.
- Pachenari, M.; Seyedpour, S.M.; Janmaleki, M.; Shayan, S.B.; Taranejoo, S.; Hosseinkhani, H. Mechanical Properties of Cancer Cytoskeleton Depend on Actin Filaments to Microtubules Content: Investigating Different Grades of Colon Cancer Cell Lines. J. Biomech. 2014, 47, 373–379.
- Ketene, A.N.; Schmelz, E.M.; Roberts, P.C.; Agah, M. The Effects of Cancer Progression on the Viscoelasticity of Ovarian Cell Cytoskeleton Structures. Nanomedicine 2012, 8, 93–102.
- Ochalek, T.; Nordt, F.J.; Tullberg, K.; Burger, M.M. Correlation between Cell Deformability and Metastatic Potential in B16-F1 Melanoma Cell Variants. Cancer Res. 1988, 48, 5124–5128.
- Kramer, N.; Walzl, A.; Unger, C.; Rosner, M.; Krupitza, G.; Hengstschläger, M.; Dolznig, H. In Vitro Cell Migration and Invasion Assays. Mutat. Res.—Rev. Mutat. Res. 2013, 752, 10–24.
- Paul, C.D.; Mistriotis, P.; Konstantopoulos, K. Cancer Cell Motility: Lessons from Migration in Confined Spaces. Nat. Rev. Cancer 2017, 17, 131–140.
- Van Golen, K.L.; Wu, Z.F.; Xiao, X.T.; Bao, L.W.; Merajver, S.D. RhoC GTPase, a Novel Transforming Oncogene for Human Mammary Epithelial Cells That Partially Recapitulates the Inflammatory Breast Cancer Phenotype. Cancer Res. 2000, 60, 5832–5838.
- Lin, M.; DiVito, M.M.; Merajver, S.D.; Boyanapalli, M.; van Golen, K.L. Regulation of Pancreatic Cancer Cell Migration and Invasion by RhoC GTPase and Caveolin-1. Mol. Cancer 2005, 4, 21.
- Shelby, J.P.; White, J.; Ganesan, K.; Rathod, P.K.; Chiu, D.T. A Microfluidic Model for Single-Cell Capillary Obstruction by Plasmodium Falciparum-Infected Erythrocytes. Proc. Natl. Acad. Sci. USA 2003, 100, 14618–14622.
- Lautscham, L.A.; Kämmerer, C.; Lange, J.R.; Kolb, T.; Mark, C.; Schilling, A.; Strissel, P.L.; Strick, R.; Gluth, C.; Rowat, A.C.; et al. Migration in Confined 3D Environments Is Determined by a Combination of Adhesiveness, Nuclear Volume, Contractility, and Cell Stiffness. Biophys. J. 2015, 109, 900–913.
- Mak, M.; Reinhart-King, C.A.; Erickson, D. Elucidating Mechanical Transition Effects of Invading Cancer Cells with a Subnucleus-Scaled Microfluidic Serial Dimensional Modulation Device. Lab Chip 2013, 13, 340–348.
- Albini, A.; Benelli, R. The Chemoinvasion Assay: A Method to Assess Tumor and Endothelial Cell Invasion and Its Modulation. Nat. Protoc. 2007, 2, 504–511.
- McEwan, R.N.; Kleinman, H.K.; Martin, G.R. A Rapid in Vitro Assay for Quantitating the Invasive Potential of Tumor Cells. Cancer Res. 1987, 47, 3239–3245.
- Justus, C.R.; Leffler, N.; Ruiz-Echevarria, M.; Yang, L.V. In Vitro Cell Migration and Invasion Assays. J. Vis. Exp. 2014, 88, 51046.
- Sieuwerts, A.M.; Klijn, J.G.M.; Foekens, J.A. Assessment of the Invasive Potential of Human Gynecological Tumor Cell Lines with the in Vitro Boyden Chamber Assay: Influences of the Ability of Cells to Migrate through the Filter Membrane. Clin. Exp. Metastasis 1997, 15, 53–62.
- Nyström, M.L.; Thomas, G.J.; Stone, M.; Mackenzie, I.C.; Hart, I.R.; Marshall, J.F. Development of a Quantitative Method to Analyse Tumour Cell Invasion in Organotypic Culture. J. Pathol. 2005, 205, 468–475.
- Ayala, I.; Baldassarre, M.; Caldieri, G.; Buccione, R. Invadopodia: A Guided Tour. Eur. J. Cell Biol. 2006, 85, 159–164.
- Artym, V.V.; Yamada, K.M.; Mueller, S.C. ECM Degradation Assays for Analyzing Local Cell Invasion. Methods Mol. Biol. 2009, 522, 211–219.
- Merkher, Y.; Horesh, Y.; Abramov, Z.; Shleifer, G.; Ben-Ishay, O.; Kluger, Y.; Weihs, D. Rapid Cancer Diagnosis and Early Prognosis of Metastatic Risk Based on Mechanical Invasiveness of Sampled Cells. Ann. Biomed. Eng. 2020, 48, 2846–2858.
- Merkher, Y.; Weihs, D. Proximity of Metastatic Cells Enhances Their Mechanobiological Invasiveness. Ann. Biomed. Eng. 2017, 45, 1399–1406.
- Merkher, Y.; Alvarez-Elizondo, M.B.; Weihs, D. Taxol Reduces Synergistic, Mechanobiological Invasiveness of Metastatic Cells. Converg. Sci. Phys. Oncol. 2017, 3, 044002.
- Merkher, Y.; Kontareva, E.; Melekhova, A.; Leonov, S. Abstract PO-042: Nanoparticles Imaging for Cancer Metastasis Diagnosis. Clin. Cancer Res. 2021, 27, PO-042.
- Merkher Yulia; Kontareva Elizaveta; Bogdan Elizaveta; Achkasov Konstantin; Grolman Joshua; Leonov Sergey Nanoparticle Cellular Endocytosis as Potential Prognostic Biomarker for Cancer Progression. FEBS Open Bio 2021, 11, 429–430.
- Li, Y.; Zhang, H.; Merkher, Y.; Chen, L.; Liu, N.; Leonov, S.; Chen, Y. Recent Advances in Therapeutic Strategies for Triple-Negative Breast Cancer. J. Hematol. Oncol. 2022, 15, 121.
