This review focused on current challenges and future directions on the treatment and prevention of ovarian failure or infertility by chemotherapy in young reproductive women with cancer. We also address current knowledge on chemotherapy-induced ovarian toxicity and its mechanisms. We hope this review will help clinicians to prevent and treat girls and young women with cancer who desire to preserve their ovarian endocrine function and fertility.
- gonadotoxicity
- fertility preservation
- embryo cryopreservation
- oocyte cryopreservation
- ovarian tissue cryopreservation
- oocyte in vitro maturation
- artificial ovaries
- stem cell technologies
- ovarian suppression
- oncofertility
1. Introduction
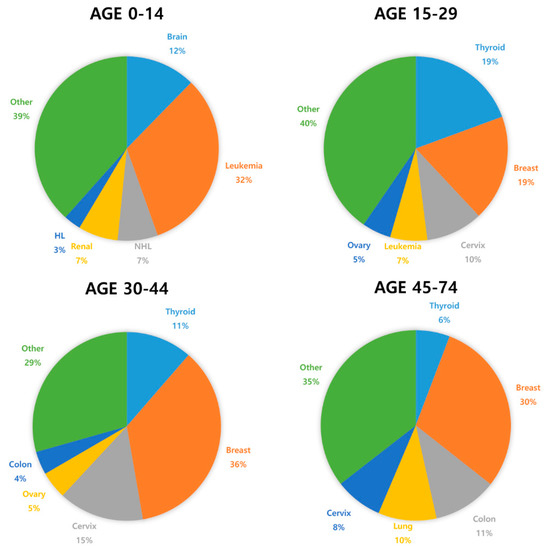
Cancer incidence is rapidly growing worldwide. In 2018, 8.6 million women were diagnosed with cancer globally [1]. Most women diagnosed with cancer are older, but 10% are <45 years of age [2]. Due to advances in cancer diagnosis and treatment, the survival rate for prepubertal and young women with cancer has significantly improved. In Europe, the five-year-survival rate is 79.1% in children diagnosed with cancer [3]. However, aggressive chemotherapy can cause impairment of reproductive functions and even fertility loss [4][5][6][7][4,5,6,7]. Although depletion of ovarian function is associated with improved survival outcomes in breast cancer patients of reproductive age, it has several side effects, such as hot flashes, osteoporosis, and sexual dysfunction [8]. Cardiovascular disease is the main cause of shortened life expectancy in women with premature ovarian insufficiency (POI) [9]. Moreover, chemotherapy-related POI and infertility may be associated with increased risk of neuro-degenerating disease and psychosocial distress [9].
In recent years, interest in fertility preservation has increased significantly among female cancer patients [10]. Despite the huge interest cancer patients have with respect to preserving fertility, there is an unmet need in children and young cancer survivors [11]. Oncofertility is a relatively innovative concept that describes a multidisciplinary network of experts focused on developing and providing the option of fertility preservation to young cancer patients. Currently, embryo and oocyte cryopreservation are the only established methods for fertility preservation [12]. However, there is accumulating evidence for other experimental techniques including ovarian tissue cryopreservation, artificial ovaries, and in vitro maturation [13].
2. The Effect of Chemotherapy on Ovarian Function
2.1. Risk of Ovarian Toxicity Due to Chemotherapy Agents
Although the survival rate of cancer patients has dramatically improved due to development of chemotherapy, ovarian toxicity induced by chemotherapy is a major complication. Gonadotoxic chemotherapy during reproductive age can lead to iatrogenic primary ovarian insufficiency (POI), and loss of follicular reserve that depends on the type, dose, duration, and combination of chemotherapeutic agents, and disease stage, as well as patient age [14][15]. It has been reported that 53–89% of chemotherapy-induced POI occurs in patients with breast cancer [16]. The combination of abdominal radiation and alkylating agents which are likely to cause gonadotoxicity induces POI in almost 100% of cancer patients [17][18]. In a large study of cancer survivors, the risk of POI was increased 9.2-fold for patients who received chemotherapy including alkylating agents and 27-fold in women who received combination alkylating agent-based chemotherapy and radiotherapy [19].
Table 1 show the most common cancers and the risk of chemotherapy-induced ovarian toxicity in women according to chemotherapy protocol and age [3][20][21]. Notice that the course of chemotherapy and its related risks of gonadotoxicity can be unpredictable and variable due to treatment response and disease prognosis, i.e., refractory or recurrent cases [13][22]. In order to prevent POI due to chemotherapy and subsequent complications, effective and comprehensive oncofertility strategies should be undertaken to preserve fertility in young reproductive age women before initiation of cancer treatment [17][23][24][25][26].
Table 1.
| Diagnosis | Chemotherapy Protocol | Risk of Iatrogenic POI | |||||
|---|---|---|---|---|---|---|---|
| Non-Hodgkin lymphoma |
Cyclophosphamide, hydroxydaunorubicin, oncovin, and prednisone (CHOP) (four to six cycles) Rituximab, cyclophosphamide, hydroxydaunorubicin, oncovin, and prednisone (R-CHOP) (four to six cycles) |
<20% [3][28] | <20% [3,28] | ||||
| Hodgkin lymphoma |
Adriamycin, bleomycin, vinblastine, and dacarbazine (ABVD) |
<20% [3] | <20% [3] | ||||
| Mustargen, oncovin, prednisone, and procarbazine (MOPP) |
10–50% [29][30][31][32] | 10–50% [29,30,31,32] | |||||
| Bleomycin, etoposide, adriamycin, cyclophosphamide, oncovin, procarbazine, and prednisone (BEACOPP) (eight cycles) |
50–95% (age dependent) [33] | ||||||
| Acute lympho- cytic leukemia |
Most standard chemotherapy protocols do not include a gonadotoxic multi-agent | <20% [3][13][14] | <20% [3,13,14] | ||||
| Acute myeloid leukemia |
Most standard chemotherapy protocols do not include gonadotoxic anthracycline/cytarabine | <20% [3][13][14] | <20% [3,13,14] | ||||
| Breast cancer | Cyclophosphamide, methotrexate, fluorouracil (CMF) (six cycles) Cyclophosphamide, epirubicin, fluorouracil (CEF) (six cycles) Cyclophosphamide, eoxorubicin (adriamycin), fluorouracil (CAF) (six cycles) |
>80% [3] (≥age 40) |
|||||
| 30–70% [3] (age 30–39) |
|||||||
| Doxorubicin (adriamycin), cyclophosphamide (AC) (four cycles) |
30–70% [3] (≥age 40) |
||||||
| >20 [3] (age 30–39) |
|||||||
| Others | Cyclophosphamide ≥ 7 g/m | 2 | in females < 20 years Cyclophosphamide ≥ 5 g/m | 2 | in females > 40 years Any alkylating agent (e.g., cyclophosphamide, ifosfamide, busulfan, carmustine, lomustine) |
>80% [34][35] | >80% [34,35] |
| Cyclophosphamide ≥ 5 g/m | 2 | in females 30–40 years | 30–70% [34][35] | 30–70% [34,35] | |||
| Taxanes Oxaliplatin Irinotecan Monoclonal antibodies (trastuzumab, bevacizumab, cetuximab) Tyrosine kinase inhibitors (erlotinib, imatinib) |
Unknown |
2.2. Mechanisms of Ovarian Toxicity
Gonadotoxic chemotherapy leads to primordial follicle loss, resulting in POI and infertility. Both direct acute and indirect delayed mechanisms have been reported for the effects of anticancer agents that cause a decrease in ovarian reserve. The main mechanism is that anticancer drugs directly induce DNA double-strand breaks (DSBs), which activate apoptosis and/or autophagy-related pathways [36][37][38][39][40][41][42][36,37,38,39,40,41,42]. The second mechanism is that anticancer drugs can indirectly cause primordial follicle depletion by microvascular and stromal injury through ischemia, necrosis, or inflammation [38][42][43][44][45][38,42,43,44,45]. There is third hypothesis called the “burnout” effect. A few studies have shown that anticancer drugs induce activation of the phosphoinositide 3-kinase/protein kinase B/forkhead box protein O3a (PI3K/AKT/FOXO3a) pathway, which leads to follicle reduction by massive activation of primordial follicles in mice and cultured human ovarian tissue [36][46][47][48][49][36,46,47,48,49]. However, there is some question of methodology and biological mechanism of follicle loss based on studies supporting “burnout theory”. It has not been proven that primordial follicle growth is the main cause of chemotherapy-induced primordial follicle loss. Thus, the “burnout” theory of chemotherapy-induced follicle depletion is still lacking evidence and is under debate [36][46][36,46]. The main cause of the follicle depletion induced by chemotherapy seems to be DNA double-strand breaks and apoptosis.
3. Improving Oncofertility Care
Preserving fertility is important to most young cancer survivors. One study reported that more than half (51.7%) of young women undergoing cancer treatment felt that having children was the “most important” issue in their life [50]. The fear of treatment-related infertility may affect patients’ decision making in choosing cancer treatment among those who want to conceive their own genetic offspring [51][52]. Therefore, according to the ASCO, clinicians should refer cancer patients who are undecided or uncertain about their fertility intentions to a reproductive specialist for a fertility preservation consultation before initiating cancer treatment [53][54]. Established in 2007, the Oncofertility Consortium (OC) is a nationwide network of oncologists, reproductive specialists, and research scientists for fertility preservation in young cancer patients [55]. The National Physicians Cooperative, formed by the OC to share knowledge and resources, comprises 60 centers across the United States that provide oncofertility services to women [56]. In Japan, after establishment of the Japan Society for Fertility Preservation (JSFP) in 2012, there are 46 current medical institutions for preserving fertility. In Europe, the FertiPROTEKT network was founded in May 2006, and has included approximately 100 centers from Germany, Austria, and Switzerland since January 2014 [55].
Despite the increasing interest in and the advance of technologies available in the oncofertility field, accessibility to fertility preservation remains relatively low for young cancer patients, particularly those in low- and middle-income countries [57][58]. In a retrospective cohort study of women aged 18–42 years diagnosed with cancer, 20.6% received fertility preservation care [57]. In another study, only 9% of patients received any information on fertility preservation options [59].
Major barriers are lack of awareness among oncologists, lack of referrals from oncologists, lack of interinstitutional networks, and lack of oncofertility specialists [20]. In addition, many oncologists fail to have fertility discussions with their cancer patients and, thus, fail to make timely referrals due to patients’ lack of awareness of treatment-related infertility, together with time pressures, financial costs, and conflicting priorities of physicians [60][61].
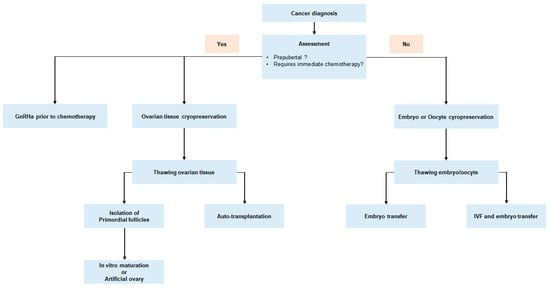
Figure 2.