The p21 Activated Kinases (PAKs) are serine threonine kinases and play important roles in many biological processes, including cell growth, survival, cytoskeletal organization, migration, and morphology. Recently, PAKs have emerged in the process of liver disorders, including liver cancer, hepatic ischemia-reperfusion injury, hepatitis, and liver fibrosis, owing to their effects in multiple signaling pathways in various cell types. Activation of PAKs promotes liver cancer growth and metastasis and contributes to the resistance of liver cancer to radiotherapy and chemotherapy, leading to poor survival of patients. PAKs also play important roles in the development and progression of hepatitis and other pathological processes of the liver such as fibrosis and ischemia-reperfusion injury.
- p21 Activated Kinase
- liver cancer
- hepatitis
- liver fibrosis
1. Introduction
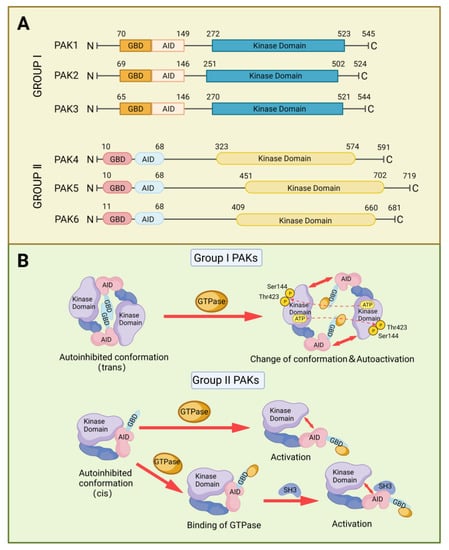
2. Structure and Activation of PAKs Family
3. PAKs in Liver Cancers
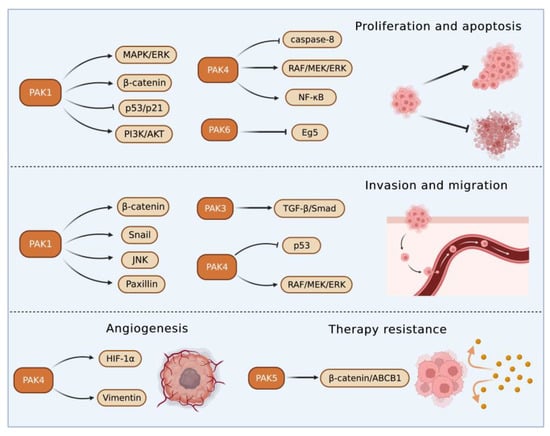
3.1. Roles of Group I PAKs in Liver Cancer
3.2. Roles of Group II PAKs in Liver Cancer
PAK4 enhanced HCC cell survival by modulating caspase-8 and NF-κB pathways [55][61]. In an HCC transgenic mouse model, miR-199-3p inhibited HCC growth by targeting the PAK4/RAF/MEK/ERK pathway [56][57][62,63]. On the contrary, an increased cyclin-dependent kinase 5 (CDK5) regulatory subunit-associated protein 3 in HCC accelerated tumor metastasis bound to and activated PAK4 [58][64]. PAK4 promoted migration and invasion of HCC cells through direct phosphorylation of p53 at S215 [59][65]. MiR-1271 suppressed HCC growth and metastasis through downregulation of RAF/MEK/ERK signaling, achieved by inhibiting Zic2/PAK4. PAK4 was overexpressed in metastatic tumor tissues compared with primary tumor and normal tissues, and PAK4 expression was correlated with worse survival of HCC patients. The results from multivariate analyses of 615 HCC patients showed that PAK4 was an independent indicator of poor prognosis [60][66]. MiR-433 was reduced in HCC tissues. MiR-433 repressed the viability of HCC cells through directly binding to the sequence at 3’-UTR of PAK4 mRNA, which in turn inhibited PAK4 expression [61][67]. MiRNAs are key upstream regulators that directly modulate the translation of multiple oncogenic proteins including PAK4. A miRNA cocktail therapy targeting PAK4, mechanistic target of rapamycin (mTOR), and RAS homolog gene family member C (RHOC), showed remarkable anti-HCC effects in patient-derived xenografts [62][68].
4. PAKs in Hepatic Ischemia/Reperfusion Injury
Hepatic IRI commonly occurs in the process of hemorrhagic shock, liver surgery, and liver transplantation [63][64][78,79]. The underlying mechanisms of hepatic IRI relate to the elevated oxidative stress and activation of immune-metabolic responses, which are harmful to normal cellular structures and functions, and result in liver damage [65][80]. PAKs participate in the modulation of immune responses and inflammation [66][67][81,82], and PAKs have been reported to play a critical role in hepatic IRI [6][68][6,83]. Neuregulin-1/PAK1 axis was found to decrease IRI of liver grafts with or without steatosis through increasing vascular endothelial growth factor-α and insulin growth factor-1 levels, respectively [68][83]. PAK4 was upregulated in hepatic IRI in mice and humans to promote hepatic hypoxia-reoxygenation-induced damage through phosphorylating nuclear factor erythroid 2-related factor 2 and suppressing its transcriptional activity [6]. Genetic knockout or pharmacological inhibition of PAK4 reduced the inflammation and necrosis of hepatocytes [6]. These results suggest that PAK4 inhibition may protect the liver from IRI-induced damage.5. PAKs in Hepatitis
Hepatitis is defined as inflammation of the liver, and its etiologies include virus infection, parasitic invasion, alcohol abuse, autoimmunity imbalance, and metabolic disorder. The main characteristic of hepatitis is represented by the infiltration of inflammatory cells, which induces apoptosis and necrosis of hepatocytes leading to liver damage and dysfunctions [69][70][71][72][84,85,86,87].
In hepatitis B, phosphorylation of PAK1 induced the translocation of RAF-1 to mitochondrial, which in turn facilitated the anti-apoptotic effect of HBV X protein in hepatocyte [73][88]. In fact, HBV X protein can activate PAK1, which protected HCC from anoikis and promoted the metastasis of HCC [74][56]. Results from the PCR showed that the PAK3 gene was the preferential integration site of HBV DNA and the integration potentially changed the expression of PAK3 [5].
Different from the promoting role of PAK1 in HBV, PAK1 had potentially inhibited HCV replication, and its antiviral effects were independent of interferon regulatory factor 3 but dependent on the mTOR-activated PI3K/AKT and ERK [75][91]. HCV protected the infected hepatocytes from cell death by suppressing apoptosis and inflammatory reaction partially through the upregulation of PAK2 [76][92].
In a mouse model infected with Schistosoma japonicum, PAK1 in Kupffer cells was elevated and facilitated the differentiation of CD4+ T cells to T helper 17 cells via the NF-κB/interferon regulatory factor 1/interleukin-6 pathway, leading to aggravated hepatic inflammation [77][95]. Increased PAK1 expression in Kupffer cells was also noticed in patients with autoimmune hepatitis, and the PAK1 expression was found to be associated with disease progression [78][96]. The increased expression of PAK6 found in alcoholic hepatitis may contribute to tumorigenesis [79][97].6. PAKs in Liver Fibrosis
Liver fibrosis is implicated in the interaction between injured hepatocytes, inflammatory cells, and hepatic myofibroblasts. In response to injury, hepatocytes will express more profibrogenic miRNAs and proteins such as TGFβ and Notch, thus initiating fibrosis [80][98]. The transformation from hepatic stellate cells to myofibroblasts that produce extracellular matrix (ECM) provides a protection to liver tissue from injury, and there is a balance between ECM production and degradation. However, the excessive accumulation of ECM produced by consistently activated myofibroblasts will impair the normal physiological structure and function of the liver, resulting in the occurrence of liver fibrosis [81][99]. PAK1 and PAK3 were upregulated in activated hepatic myofibroblasts and promoted fibrotic effects by enhancing the expression of integrin β-1, which is essential for myofibroblasts activation and ECM production [82][100].7. Therapeutic Effects of PAK Inhibitors in Liver Disorders
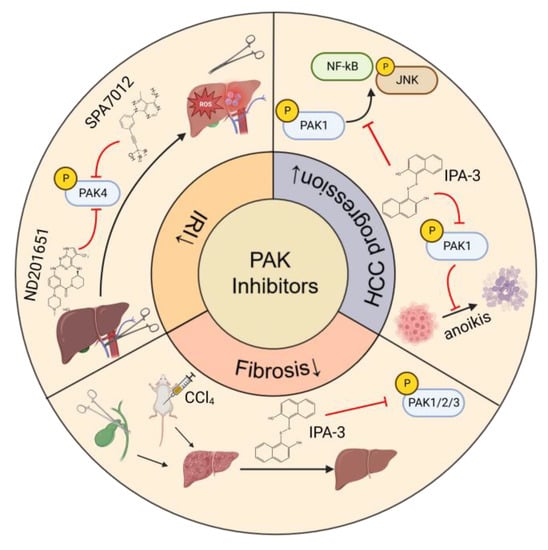
The main strategy for treating HBV or HCV-related liver diseases is long-term administration of antiviral drugs such as entecavir, disoproxil, and IFN-α. Different from HCV, HBV has the characteristic of escaping innate immunity, thus immune therapy is also a vital treatment for HBV [83][84][102,103]. For metabolism-related liver diseases, limiting alcohol consumption, changing eating patterns and diet composition, and reducing insulin resistance and improving lipid metabolism are effective regimens [85][86][104,105]. Liver resection and transplantation are considered as curative treatments for HCC. However, only a small proportion of patients can have these surgical operations at the diagnosis stage and the recurrence after surgery is high. Most HCC patients are diagnosed at advanced stages of the disease and can only have non-surgical treatments, including chemo-, radio-, and immune-therapies. The first-line therapy for advanced HCC includes broad-spectrum tyrosine kinase inhibitors, such as sorafenib and lenvatinib, and combinational therapies of immunotherapy and anti-angiogenesis therapy [87][106]. PAKs play key roles in liver disorders and thus are considered useful targets for the treatment of liver diseases. PAK inhibitors have been developed and can be divided into two categories depending on the binding sites within PAK molecules, ATP-competitive inhibitors, and allosteric PAK inhibitors [88][109]. ATP-competitive PAK inhibitors block PAK phosphorylation by targeting the ATP-binding pocket within the kinase domain. This type of PAK inhibitors is further classified into aminopyrazole-based inhibitors, aminopyrimidine-based inhibitors, indolocarbazole-based inhibitors, 2-amino pyrido[2,3-d] pyrimidine-7(8H)-one-based inhibitors, and other ATP-competitive inhibitors. Compared with ATP-competitive PAK inhibitors, allosteric PAK inhibitors have the potential to be more selective and display discriminative inhibitory activity among PAK family proteins [89][90][110,111]. The studies of the effects of PAK inhibitors in liver disorders are limited (Figure 34). PAK4 was upregulated and played a critical role in the process of hepatic IRI. Application of an ATP-competitive PAK4 inhibitor ND201651 reduced hepatic IRI [6]. Another novel specific PAK4 inhibitor, SPA7012, a pyrazolo [3,4-d] pyrimidine derivative, also showed an anti-inflammatory effect on the liver during hepatic IRI [91][112]. More experimental evidence is necessary for its clinical application.