You're using an outdated browser. Please upgrade to a modern browser for the best experience.
Please note this is a comparison between Version 2 by Dean Liu and Version 3 by Dean Liu.
Vascular graft or endograft infection (VGEI) is a complex disease that complicates vascular-surgery and endovascular-surgery procedures and determines high morbidity and mortality.
- VGEI
- infection
- vascular prosthesis
- vascular graft
1. Introduction
A vascular prosthesis is defined as a biological or artificial device meant to replace a segment of an arterial tree whose function is compromised by injury, occlusive disease, or aneurysmal degeneration. A prosthetic graft provides a substitute conduit for blood flow, allowing the diseased vessel segment to be repaired, excised, or bypassed [1][2][3][4][5][6][7][8][9][10].
Vascular prostheses include vascular grafts (VGs), generally implanted surgically, and vascular endografts (VEs) (or stent-grafts) implanted by endovascular procedure. VGs may be classified into biological grafts, which are composed of actual tissues, most often blood vessels (e.g., autologous grafts derived from the patient’s own vessel); allografts (from human vessels); xenografts (generally of bovine origins); and synthetic grafts made from either poly-ethylene-terephthalate (PET, or Dacron), a textile material, or expandedpolytetrafluoroethylene (ePTFE), a non-textile material. In textile VGs, the basic polymer is first made into a yarn, which is then used to construct a graft using various methods of knitting or weaving. Non-textile VGs are manufactured using the techniques of the precipitation or the extrusion of the polymer from solutions or sheets of the material. When the available length of an autogenous tissue graft is inadequate for the required reconstruction, composite VGs can be used. Such VGs are constructed by combining segments of an artificial prosthetic material with autogenous material to form a substitute-vessel conduit. VGs are generally positioned during open surgery and sutured both proximally and distally to the healthy artery by end-to-end or end-to-side anastomosis (Figure 1). An ideal VG should be impermeable, thromboresistant, compliant, biocompatible, durable, resistant to infection, easy to sterilize, easy to implant, readily available, and cost-effective. In particular, biocompatibility is necessary because significant tissue reaction may promote thrombosis, loss of graft integrity, and graft failure. Sterility and resistance to infection are necessary to decrease the incidence of infection. VEs are transluminally implanted vascular devices introduced into the vascular system via a remote artery using minimally invasive techniques that combine a prosthetic fabric with a vascular stent (Figure 1). Vascular stents are made by different alloys, with nitinol being the most used. The graft is anchored in place by a balloon-expandable or self-expanding metal frame that supports all or part of the graft and provides a tight seal proximal and distal to the diseased segment of the artery. Since it circumvents the need for laparotomy, the cross-clamping of the artery, and the obligatory blood loss associated with the opening of the aneurysm sac, the technique has been shown to reduce the morbidity and mortality associated with conventional surgery, and it expands the patient pool to include patients with severe medical- and co-morbidities who were previously denied treatment [11][12][13][14][15][16][17][18][19][20][21][22].
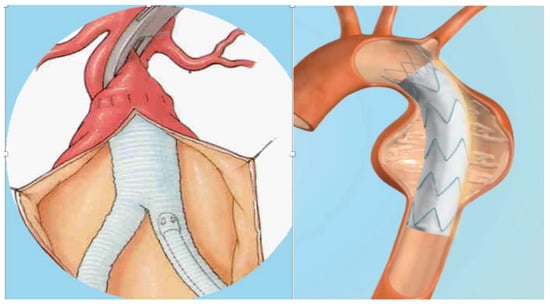
Figure 1. Vascular graft and vascular endograft. On the (left): vascular graft; on the (right): vascular endograft.
According to the location of implantation, grafts may be extra-cavitary (groins and lower limbs) and intra-cavitary (abdominal or thoracic aorta) [21][22].
Vascular prostheses may be burdened by a series of complications mainly due to fabrication or biomaterial failure such as dilation, rupture, thrombosis, allergic foreign-body reaction, and infection. In particular, a vascular graft or endograft infection (VGEI) is a clinically important complication that may occur following VG surgery or VE procedures accompanied by high morbidity and mortality rates [22][23][24][25][26][27][28][29][30][31][32][33]. The incidence of thoracic aortic VGEI is around 6% and, with mortality rates that relate to the clinical presentation, around 75%. The incidence of VGEI in the abdominal aorta is a rare complication, occurring in <1%, but one with a high mortality rate. VGEIs in peripheral-artery surgery are mainly represented by vascular graft infection (VGI) for open surgery with an incidence of up to 2.8% [22]. The percentage of infection in prosthetic arteriovenous hemodialysis grafts (AVHGs) is approximately 3.5% [34]. VGEIs are managed mainly through surgical removal, revascularization, and long-term antibiotic treatment. The explantation of an infected graft may determine important mortality rates (18–30%), while conservative management with long-term antibiotic therapy may result in a very high mortality rate, reaching about 100%, if the VGEI is not completely resolved [21].
VGEI, although not particularly frequent, is a multifaceted disease, and diagnosis may be challenging and even complicated for physicians, as they sometimes may be not as timely as an optimal treatment requires. Considering the rarity of this disease, current literature is not specialized as it lacks randomized controlled trials and studies with high patient population. Furthermore, current clinical evidence is based on small case studies, which are very often retrospective in nature [35].
2. Prevention of VGEI
The prevention of VGEI generally consist of adequate pre-operative patient preparation, heedful surgical and procedural management, antisepsis measures, prompting the administration of pre-operative antibiotic prophylaxis, and adequate wound care [34]. Before surgical procedures, it is important to treat any potential source of infection (i.e., dental problems, etc.) [22][36]. In the context of preoperative patient preparation, it seems reasonable to screen patients undergoing graft implantation for S. aureus nasal carriage and, if positive, provide peri-operative nasal eradication therapy because of the risk of potentially related severe VGEIs [22][37]. Adequate antimicrobial prophylaxis with broad-spectrum systemic antibiotics seems to significantly reduce the risk of early graft infection. Generally, the first or second generation of cephalosporin is used. It is also important that antimicrobial prophylaxis covers the most frequent bacteria, including MRSA, and for institutions with high rates of MRSA, daptomycin or vancomycin can be administered additionally [22][34]. Hair removal and appropriate aseptic care in the operating theater remain pivotal in peri-operative care [22]. Postoperative measures consist of speeding up the healing of surgical wounds, for example, the use of negative-pressure wound therapy (NPWT), whereby applying sub-atmospheric pressure decreases inflammatory exudates promoting granulation tissue, may be used to achieve fast wound closure, [38][39][40][41][42] and to consider antimicrobial prophylaxis before any dental procedure [22][43][44][45][46][47].3. Treatment of VGEI
The best treatment for VGEI mainly depends on the location of the graft, the extent of the infection, and the type of microorganism. Generally, the management plan includes the removal of the graft, a careful debridement of the infected surrounding tissues, the restoration of circulation distal to the GI, and adequate antibiotic therapy [36]. Figure 2 and Figure 3 show an infected VG and VE, respectively, during explantation procedures.
Figure 2. Explantation of an infected vascular graft at the groin.
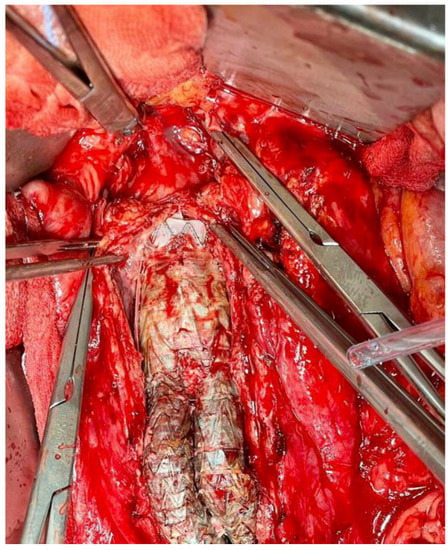
Figure 3. Explantation of an infected aortic and iliac endograft.
Figure 4
shows a general evidence-based algorithm in a case of VGEI.
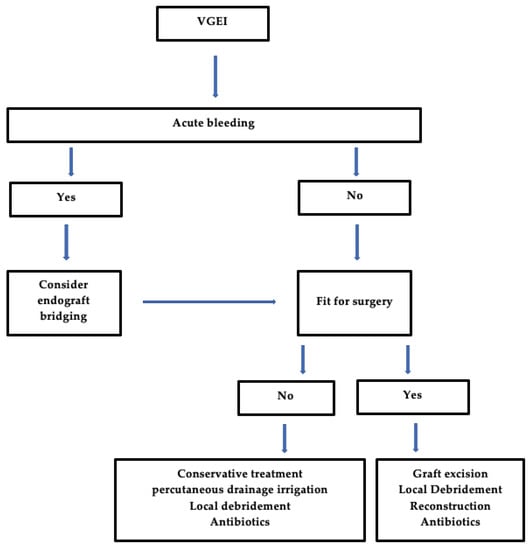
Figure 4. General Algorithm for the management of VGEI. VGEI = vascular graft or endograft infection.
References
- Pennel, T.; Zilla, P. Clinical Applications and Limitations of Vascular Grafts. In Tissue-Engineered Vascular Grafts; Reference Series in Biomedical Engineering; Walpoth, B., Bergmeister, H., Bowlin, G., Kong, D., Rotmans, J., Zilla, P., Eds.; Springer: Cham, Switzerland, 2020; pp. 1–32.
- Abbott, W.M.; Callow, A.; Moore, W.; Rutherford, R.; Veith, F.; Weinberg, S. Evaluation and performance standards for arterial prostheses. J. Vasc. Surg. 1993, 17, 746–756.
- Fazal, F.; Raghav, S.; Callanan, A.; Koutsos, V.; Radacsi, N. Recent advancements in the bioprinting of vascular grafts. Biofabrication 2021, 13, 032003.
- Dahl, S.L.; Blum, J.L.; Niklason, L.E. Bioengineered vascular grafts: Can we make them off-the-shelf? Trends Cardiovasc. Med. 2011, 21, 83–89.
- Antonyshyn, J.A.; D’Costa, K.A.; Santerre, J.P. Advancing tissue-engineered vascular grafts via their endothelialization and mechanical conditioning. J. Cardiovasc. Surg. 2020, 61, 555–576.
- Jafarihaghighi, F.; Ardjmand, M.; Mirzadeh, A.; Hassani, M.S.; Parizi, S.S. Current challenges and future trends in manufacturing small diameter artificial vascular grafts in bioreactors. Cell Tissue Bank. 2020, 21, 377–403.
- Desai, M.; Eaton-Evans, J.; Hillery, C.; Bakhshi, R.; You, Z.; Lu, J.; Hamilton, G.; Seifalian, A.M. AAA stent-grafts: Past problems and future prospects. Ann. Biomed. Eng. 2010, 38, 1259–1275.
- Leal, B.B.J.; Wakabayashi, N.; Oyama, K.; Kamiya, H.; Braghirolli, D.I.; Pranke, P. Vascular Tissue Engineering: Polymers and Methodologies for Small Caliber Vascular Grafts. Front. Cardiovasc. Med. 2021, 7, 592361.
- Obiweluozor, F.O.; Emechebe, G.A.; Kim, D.W.; Cho, H.J.; Park, C.H.; Kim, C.S.; Jeong, I.S. Considerations in the Development of Small-Diameter Vascular Graft as an Alternative for Bypass and Reconstructive Surgeries: A Review. Cardiovasc. Eng. Technol. 2020, 11, 495–521.
- Eliason, J.L.; Upchurch, G.R., Jr. Endovascular treatment of aortic aneurysms: State of the art. Curr. Treat. Options Cardiovasc. Med. 2009, 11, 136–145.
- Iqbal, R.; Bhandare, D.; St Louis, M.; Ruchi, R. Think before you leap: Cutaneous hypersensitivity to polytetrafluoroethylene arteriovenous graft masquerading as infection. BMJ Case Rep. 2019, 12, e230401.
- Zhang, B.; Xu, Y.; Ma, S.; Wang, L.; Liu, C.; Xu, W.; Shi, J.; Qiao, W.; Yang, H. Small-diameter polyurethane vascular graft with high strength and excellent compliance. J. Mech. Behav. Biomed. Mater. 2021, 121, 104614.
- Xu, W.; Zhou, F.; Ouyang, C.; Ye, W.; Yao, M.; Xu, B. Mechanical properties of small-diameter polyurethane vascular grafts reinforced by weft-knitted tubular fabric. J. Biomed. Mater. Res. 2010, 92, 1–8.
- Kim, K.B.; Hwang, S.W.; Kim, M.S. Techniques and Outcomes of the No-Touch Vein Conduit as a Y-Composite Graft. Braz. J. Cardiovasc. Surg. 2022, 37, 38–41.
- Betz, T.; Neuwerth, D.; Steinbauer, M.; Uhl, C.; Pfister, K.; Töpel, I. Biosynthetic vascular graft: A valuable alternative to traditional replacement materials for treatment of prosthetic aortic graft infection? Scand. J. Surg. SJS Off. Organ Finn. Surg. Soc. Scand. Surg. Soc. 2019, 108, 291–296.
- Keschenau, P.R.; Gombert, A.; Barbati, M.E.; Jalaie, H.; Kalder, J.; Jacobs, M.J.; Kotelis, D. Xenogeneic materials for the surgical treatment of aortic infections. J. Thorac. Dis. 2021, 13, 3021–3032.
- Chakfé, N.; Dieval, F.; Thaveau, F.; Rinckenbach, S.; Hassani, O.; Camelot, G.; Durand, B.; Kretz, J.G.; Groupe européen de recherche sur les prothèses appliquées à la chirurgie vasculaire. Substituts vasculaires. Vascular graft prosthesis. Ann. Chir. 2004, 129, 301–309.
- Lejay, A.; Vento, V.; Kuntz, S.; Steinmetz, L.; Georg, Y.; Thaveau, F.; Heim, F.; Chakfé, N. Current status on vascular substitutes. J. Cardiovasc. Surg. 2020, 61, 538–543.
- Droc, I.; Calinescu, F.B.; Droc, G.; Blaj, C.; Dammrau, R. Aortic stenting. Minim. Invasive Ther. Allied Technol. MITAT Off. J. Soc. Minim. Invasive Ther. 2015, 24, 296–304.
- Vento, V.; Lejay, A.; Kuntz, S.; Ancetti, S.; Heim, F.; Chakfé, N.; Gargiulo, M. Current status on aortic endografts. J. Cardiovasc. Surg. 2020, 61, 544–554.
- Arnon-Sheleg, E.; Keidar, Z. Vascular Graft Infection Imaging. Semin. Nucl. Med. 2023, 53, 70–77.
- Chakfé, N.; Diener, H.; Lejay, A.; Assadian, O.; Berard, X.; Caillon, J.; Fourneau, I.; Glaudemans, A.W.J.M.; Koncar, I.; Lindholt, J.; et al. Editor’s Choice—European Society for Vascular Surgery (ESVS) 2020 Clinical Practice Guidelines on the Management of Vascular Graft and Endograft Infections. Eur. J. Vasc. Endovasc. Surg. 2020, 59, 339–384, Erratum in: Eur. J. Vasc. Endovasc. Surg. 2020, 60, 958.
- Puges, M.; Bérard, X.; Caradu, C.; Accoceberry, I.; Gabriel, F.; Cazanave, C. Fungal Vascular Graft and Endograft Infections are Frequently Associated with Aorto-Enteric Fistulas. Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 2021, 62, 819–820.
- Čertík, B.; Třeška, V.; Moláček, J.; Šulc, R.; Houdek, K.; Opatrný, V. Infections associated with vascular reconstruction procedures at the Department of Surgery in Pilsen in retrospect. Ohlédnutí za infekcemi cévních rekonstrukcí na chirurgické klinice v Plzni. Rozhl. Chir. Mesic. Ceskoslovenske Chir. Spol. 2022, 101, 318–325.
- Yolgosteren, A.; Kumtepe, G.; Payaslioglu, M.; Ozakin, C. In-vivo evaluation of the effect of cyanoacrylate on prosthetic vascular graft infection—Does cyanoacrylate increase the severity of infection? VASA. Z. Gefasskrankh. 2020, 49, 281–284.
- Mufty, H.; Van Den Eynde, J.; Meuris, B.; Metsemakers, W.J.; Van Wijngaerden, E.; Vandendriessche, T.; Steenackers, H.P.; Fourneau, I. Pre-clinical in vivo Models of Vascular Graft Coating in the Prevention of Vascular Graft Infection: A Systematic Review. Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 2021, 62, 99–118.
- Wilson, W.R.; Bower, T.C.; Creager, M.A.; Amin-Hanjani, S.; O’Gara, P.T.; Lockhart, P.B.; Darouiche, R.O.; Ramlawi, B.; Derdeyn, C.P.; Bolger, A.F.; et al. Vascular Graft Infections, Mycotic Aneurysms, and Endovascular Infections: A Scientific Statement From the American Heart Association. Circulation 2016, 134, e412–e460.
- Smeds, M.R.; Duncan, A.A.; Harlander-Locke, M.P.; Lawrence, P.F.; Lyden, S.; Fatima, J.; Eskandari, M.K.; Vascular Low-Frequency Disease Consortium. Treatment and outcomes of aortic endograft infection. J. Vasc. Surg. 2016, 63, 332–340.
- Argyriou, C.; Georgiadis, G.S.; Lazarides, M.K.; Georgakarakos, E.; Antoniou, G.A. Endograft Infection After Endovascular Abdominal Aortic Aneurysm Repair: A Systematic Review and Meta-analysis. J. Endovasc. Ther. Off. J. Int. Soc. Endovasc. Spec. 2017, 24, 688–697.
- Szczot, M.; Meybeck, A.; Legout, L.; Pasquet, A.; Van Grunderbeeck, N.; Langlois, J.; Sarraz-Bournet, B.; Devos, P.; Leroy, O. Vascular graft infections in the intensive care unit: Clinical spectrum and prognostic factors. J. Infect. 2011, 62, 204–211.
- Kingsmore, D.; Stevenson, K.; Jackson, A.; Richarz, S.; Isaak, A.; White, B.; Thomson, P. Application and implications of a standardised reporting system for arteriovenous access graft infection. J. Vasc. Access 2022, 23, 353–359.
- Husmann, L.; Eberhard, N.; Huellner, M.W.; Ledergerber, B.; Mueller, A.; Gruenig, H.; Messerli, M.; Mestres, C.A.; Rancic, Z.; Zimmermann, A.; et al. Impact of unknown incidental findings in PET/CT examinations of patients with proven or suspected vascular graft or endograft infections. Sci. Rep. 2021, 11, 13747.
- Wouthuyzen-Bakker, M.; van Oosten, M.; Bierman, W.; Winter, R.; Glaudemans, A.; Slart, R.; Toren-Wielema, M.; Tielliu, I.; Zeebregts, C.J.; Prakken, N.H.J.; et al. Diagnosis and treatment of vascular graft and endograft infections: A structured clinical approach. Int. J. Infect. Dis. IJID Off. Publ. Int. Soc. Infect. Dis. 2022, 126, 22–27.
- Young, M.H.; Upchurch, G.R., Jr.; Malani, P.N. Vascular graft infections. Infect. Dis. Clin. N. Am. 2012, 26, 41–56.
- Van Hemelrijck, M.; Sromicki, J.; Husmann, L.; Rancic, Z.; Hasse, B.; Carrel, T.P. Vascular graft infections. Vessel Plus 2022, 6, 47.
- Gharamti, A.; Kanafani, Z.A. Vascular Graft Infections: An update. Infect. Dis. Clin. N. Am. 2018, 32, 789–809.
- Langenberg, J.C.M.; Kluytmans, J.A.J.W.; Mulder, P.G.H.; Romme, J.; Ho, G.H.; Van Der Laan, L. Peri-Operative Nasal Eradication Therapy Prevents Staphylococcus aureus Surgical Site Infections in Aortoiliac Surgery. Surg. Infect. 2018, 19, 510–515.
- Norman, G.; Goh, E.L.; Dumville, J.C.; Shi, C.; Liu, Z.; Chiverton, L.; Stankiewicz, M.; Reid, A. Negative pressure wound therapy for surgical wounds healing by primary closure. Cochrane Database Syst. Rev. 2020, 6, CD009261.
- Svensson-Björk, R.; Hasselmann, J.; Asciutto, G.; Zarrouk, M.; Björk, J.; Bilos, L.; Pirouzram, A.; Acosta, S. Negative Pressure Wound Therapy for the Prevention of Surgical Site Infections Using Fascia Closure After EVAR-A Randomized Trial. World J. Surg. 2022, 46, 3111–3120.
- Cheng, H.T.; Hsu, Y.C.; Wu, C.I. Efficacy and safety of negative pressure wound therapy for Szilagyi grade III peripheral vascular graft infection. Interact. Cardiovasc. Thorac. Surg. 2014, 19, 1048–1052.
- Andersson, S.; Monsen, C.; Acosta, S. Outcome and Complications Using Negative Pressure Wound Therapy in the Groin for Perivascular Surgical Site Infections after Vascular Surgery. Ann. Vasc. Surg. 2018, 48, 104–110.
- O’Malley, P.; McDonnell, C. Negative pressure wound therapy-two novel approaches to healing dehisced vascular bypass wounds. J. Wound Care 2021, 30, 449–453.
- Acosta, S.; Björck, M.; Wanhainen, A. Negative-pressure wound therapy for prevention and treatment of surgical-site infections after vascular surgery. Br. J. Surg. 2017, 104, e75–e84.
- Kwon, J.; Staley, C.; McCullough, M.; Goss, S.; Arosemena, M.; Abai, B.; Salvatore, D.; Reiter, D.; DiMuzio, P. A randomized clinical trial evaluating negative pressure therapy to decrease vascular groin incision complications. J. Vasc. Surg. 2018, 68, 1744–1752.
- Lee, K.; Murphy, P.B.; Ingves, M.V.; Duncan, A.; DeRose, G.; Dubois, L.; Forbes, T.L.; Power, A. Randomized clinical trial of negative pressure wound therapy for high-risk groin wounds in lower extremity revascularization. J. Vasc. Surg. 2017, 66, 1814–1819.
- Ikeno, Y.; Sakakibara, S.; Yokawa, K.; Kitani, K.; Nakai, H.; Yamanaka, K.; Inoue, T.; Tanaka, H.; Terashi, H.; Okita, Y. Post-sternotomy deep wound infection following aortic surgery: Wound care strategies to prevent prosthetic graft replacement†. Eur. J. Cardio-Thorac. Surg. Off. J. Eur. Assoc. Cardio-Thorac. Surg. 2019, 55, 975–983.
- Lafaurie, G.I.; Noriega, L.A.; Torres, C.C.; Castillo, Y.; Moscoso, S.B.; Mosquera, S.; Díaz-Báez, D.; Chambrone, L. Impact of antibiotic prophylaxis on the incidence, nature, magnitude, and duration of bacteremia associated with dental procedures: A systematic review. J. Am. Dent. Assoc. 2019, 150, 948–959.
- Khalid, W.; Puges, M.; Stenson, K.; Cazanave, C.; Ducasse, E.; Caradu, C.; Berard, X. Referral Centre Experience with Infected Abdominal Aortic Endograft Explantation. Eur. J. Vasc. Endovasc. Surg. 2023, 65, 149–158.
- Gavali, H.; Mani, K.; Furebring, M.; Olsson, K.W.; Lindström, D.; Sörelius, K.; Sigvant, B.; Gidlund, K.D.; Torstensson, G.; Andersson, M.; et al. Editor’s Choice—Outcome of Radical Surgical Treatment of Abdominal Aortic Graft and Endograft Infections Comparing Extra-anatomic Bypass with In Situ Reconstruction: A Nationwide Multicentre Study. Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 2021, 62, 918–926.
- Saleem, B.R.; Meerwaldt, R.; Tielliu, I.F.; Verhoeven, E.L.; van den Dungen, J.J.; Zeebregts, C.J. Conservative treatment of vascular prosthetic graft infection is associated with high mortality. Am. J. Surg. 2010, 200, 47–52.
- Caradu, C.; Puges, M.; Cazanave, C.; Martin, G.; Ducasse, E.; Bérard, X.; Bicknell, C.; Imperial Vascular Unit and the University Hospital of Bordeaux Vascular Unit. Outcomes of patients with aortic vascular graft and endograft infections initially contra-indicated for complete graft explantation. J. Vasc. Surg. 2022, 76, 1364–1373.e3.
- Masabni, K.; Weaver, M.R.; Kandagatla, P.; Shepard, A.D.; Huang, J.; Al Adas, Z.; Liang, L.; Balraj, P.; Nypaver, T.J.; Kabbani, L.S. Cryopreserved Allograft in the Management of Native and Prosthetic Aortic Infections. Ann. Vasc. Surg. 2019, 56, 1–10.
- Mestres, C.A.; Quintana, E.; Kopjar, T.; Ambrosioni, J.; Almela, M.; Fuster, D.; Ninot, S.; Miró, J.M.; Hospital Clinic Infective Endocarditis Investigators. Twenty-year experience with cryopreserved arterial allografts for vascular infections. Eur. J. Cardio-Thorac. Surg. Off. J. Eur. Assoc. Cardio-Thorac. Surg. 2019, 55, 358–365.
- Couture, T.; Gaudric, J.; Davaine, J.M.; Jayet, J.; Chiche, L.; Jarraya, M.; Koskas, F. Results of cryopreserved arterial allograft replacement for thoracic and thoracoabdominal aortic infections. J. Vasc. Surg. 2021, 73, 626–634.
- Lee, J.; Chan, M.C.; James, C.; Lantis, J.C., 2nd. Cryopreserved Allograft Use in Vascular Surgery. Surg. Technol. Int. 2020, 37, 237–243.
- Touma, J.; Cochennec, F.; Parisot, J.; Fialaire Legendre, A.; Becquemin, J.P.; Desgranges, P. In situ reconstruction in native and prosthetic aortic infections using cryopreserved arterial allografts. Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 2014, 48, 292–299.
- Weiss, S.; Bachofen, B.; Widmer, M.K.; Makaloski, V.; Schmidli, J.; Wyss, T.R. Long-term results of cryopreserved allografts in aortoiliac graft infections. J. Vasc. Surg. 2021, 74, 268–275.
- Špaček, M.; Měřička, P.; Janoušek, L.; Štádler, P.; Adamec, M.; Vlachovský, R.; Guňka, I.; Navrátil, P.; Thieme, F.; Špunda, R.; et al. Current vascular allograft procurement, cryopreservation and transplantation techniques in the Czech Republic. Adv. Clin. Exp. Med. Off. Organ Wroc. Med. Univ. 2019, 28, 529–534.
- Lejay, A.; Delay, C.; Girsowicz, E.; Chenesseau, B.; Bonnin, E.; Ghariani, M.Z.; Thaveau, F.; Georg, Y.; Geny, B.; Chakfe, N. Cryopreserved Cadaveric Arterial Allograft for Arterial Reconstruction in Patients with Prosthetic Infection. Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 2017, 54, 636–644.
- Janko, M.R.; Bose, S.; Lawrence, P.F. Current status of treatment for aortic graft infection: When should cryopreserved allografts be used? Semin. Vasc. Surg. 2019, 32, 81–87.
- Antonopoulos, C.N.; Papakonstantinou, N.A.; Hardy, D.; Lyden, S.P. Editor’s Choice—Cryopreserved Allografts for Arterial Reconstruction after Aorto-Iliac Infection: A Systematic Review and Meta-Analysis. Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 2019, 58, 120–128.
- Goëau-Brissonnière, O.; Javerliat, I.; Koskas, F.; Coggia, M.; Pechère, J.C. Rifampin-bonded vascular grafts and postoperative infections. Ann. Vasc. Surg. 2011, 25, 134–142.
- Okita, Y.; Yamanaka, K.; Okada, K. Opinion: Aortic Graft Infection-Any Guidelines or Just Surgeon’s Experience Lines! Semin. Thorac. Cardiovasc. Surg. 2019, 31, 674–678.
- Mufty, H.; Van den Eynde, J.; Steenackers, H.P.; Metsemakers, W.J.; Meuris, B.; Fourneau, I. A systematic review of preclinical data regarding commercial silver-coated vascular grafts. J. Vasc. Surg. 2021, 74, 1386–1393.e1.
- Ricco, J.B.; Assadian, O. Antimicrobial silver grafts for prevention and treatment of vascular graft infection. Semin. Vasc. Surg. 2011, 24, 234–241.
- Matic, P.; Tanaskovic, S.; Babic, S.; Gajin, P.; Jocic, D.; Nenezic, D.; Ilijevski, N.; Vucurevic, G.; Radak, D.J. In situ revascularisation for femoropopliteal graft infection: Ten years of experience with silver grafts. Vascular 2014, 22, 323–327.
- Berard, X.; Puges, M.; Pinaquy, J.B.; Cazanave, C.; Stecken, L.; Bordenave, L.; Pereyre, S.; M’Zali, F. In vitro Evidence of Improved Antimicrobial Efficacy of Silver and Triclosan Containing Vascular Grafts Compared with Rifampicin Soaked Grafts. Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 2019, 57, 424–432.
- Batt, M.; Jean-Baptiste, E.; O’Connor, S.; Bouillanne, P.J.; Haudebourg, P.; Hassen-Khodja, R.; Declemy, S.; Farhad, R. In-situ revascularisation for patients with aortic graft infection: A single centre experience with silver coated polyester grafts. Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 2008, 36, 182–188.
- Molacek, J.; Treska, V.; Houdek, K.; Opatrný, V.; Certik, B.; Baxa, J. Use of a Silver-Impregnated Vascular Graft: Single-Center Experience. Antibiotics 2022, 11, 386.
- Savlania, A.; Tripathi, R.K. Aortic reconstruction in infected aortic pathology by femoral vein “neo-aorta”. Semin. Vasc. Surg. 2019, 32, 73–80.
- Nordanstig, J.; Törngren, K.; Smidfelt, K.; Roos, H.; Langenskiöld, M. Deep Femoral Vein Reconstruction of the Abdominal Aorta and Adaptation of the Neo-Aortoiliac System Bypass Technique in an Endovascular Era. Vasc. Endovasc. Surg. 2019, 53, 28–34.
- Laohapensang, K.; Arworn, S.; Orrapin, S.; Reanpang, T.; Orrapin, S. Management of the infected aortic endograft. Semin. Vasc. Surg. 2017, 30, 91–94.
- Smith, S.T.; Clagett, G.P. Femoral vein harvest for vascular reconstructions: Pitfalls and tips for success. Semin. Vasc. Surg. 2008, 21, 35–40.
- Sorber, R.; Osgood, M.J.; Abularrage, C.J.; Black, J.H., 3rd; Lum, Y.W. Treatment of Aortic Graft Infection in the Endovascular Era. Curr. Infect. Dis. Rep. 2017, 19, 40.
- Seeger, J.M. Management of patients with prosthetic vascular graft infection. Am. Surg. 2000, 66, 166–177.
- Uslu, H.Y.; Kurt, H. A case report of a unique aorto-bifemoral graft infection and its treatment. J. Surg. Case Rep. 2020, 11, rjaa382.
- Fujii, T.; Watanabe, Y. Multidisciplinary Treatment Approach for Prosthetic Vascular Graft Infection in the Thoracic Aortic Area. Ann. Thorac. Cardiovasc. Surg. 2015, 21, 418–427.
- Berger, P.; Moll, F.L. Aortic graft infections: Is there still a role for axillobifemoral reconstruction? Semin. Vasc. Surg. 2011, 24, 205–210.
- Harky, A.; Othman, A.; Nistal De Paz, C.; Shaw, M.; Nawaytou, O.; Harrington, D.; Kuduvalli, M.; Field, M. Systematic approach to diagnosis and management of infected prosthetic grafts in the proximal aorta. J. Card. Surg. 2021, 36, 145–152.
- Revest, M.; Camou, F.; Senneville, E.; Caillon, J.; Laurent, F.; Calvet, B.; Feugier, P.; Batt, M.; Chidiac, C.; Groupe de Réflexion sur les Infections de Prothèses vasculaires (GRIP). Medical treatment of prosthetic vascular graft infections: Review of the literature and proposals of a Working Group. Int. J. Antimicrob. Agents 2015, 46, 254–265.
- Graulus, E.; Schepens, M. Perspective: Options in managing aortic graft infections. Indian J. Thorac. Cardiovasc. Surg. 2019, 35, 186–191.
More
