Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Conner Chen and Version 3 by Conner Chen.
Tuberculosis (TB) prevalence is increasing in developed nations and continuing to cause significant mortality in low- and middle-income countries. As a result of the uptick in cases, there also exists an increased prevalence of extrapulmonary TB. TB is caused by Mycobacterium tuberculosis (M. tb). When M. tb disseminates to the vertebral column, it is called Pott’s disease or spinal TB. The frequency, symptoms, and severity of the disease range by the location of the spine and the region of the affected vertebrae.
- M. tb
- Pott’s disease
- spinal TB
- extrapulmonary TB
- pathogenesis
1. Introduction
Mycobacterium tuberculosis (M. tb) is the second leading cause of death from an infectious agent worldwide [1]. In 2018, approximately 10 million people became infected with TB, and 1.5 million died due to TB [2]. Primary infection by M. tb often seeds itself in the lungs of its host, causing Tuberculosis (TB), though in rare instances, the infection may spread to the bone and joints. Skeletal TB comprises 10% of extrapulmonary TB cases, of which 50% involve the spinal column [3][4]. Spinal TB is otherwise known as Pott’s disease, named after Pervical Pott, the first patient to present with classic spinal TB in 1779 [3][5].
The variety of the clinical manifestations of Pott’s disease proves to be a significant challenge in providing a timely and correct diagnosis in both developed and developing countries. Despite advances in imaging modalities, the time between the initial onset of symptoms to the time of diagnosis ranges between four and six months [6][7]. A delay in diagnosis is the factor that most contributes to a worse prognosis with an increased likelihood of surgical treatment and neurological deficits [6][7][8][9][10]. Magnetic resonance imaging (MRI) is capable of identifying the soft tissue changes in spinal TB but is often employed at the time of neurological symptom presentation and is mistaken for nontuberculous spinal infection [3][11]. Once symptoms progress to neurological deficits, a significant number of patients may never recover their neurological function. Kumar et al. revealed that their surgical center noted that 28% of total pediatric cases remained the same or worse after surgery, with the majority of patients presenting with neurological symptoms [12]. Treatment at the early stages of Pott’s disease with the standard treatment regimen leads to healing in approximately 95% of patients [13]. Therefore, early diagnosis is crucial to prevent the development of sequelae. However, physicians often exhibit a low index of suspicion of Pott’s disease, especially those from low-incidence countries [6]. Patients may present with non-specific symptoms and misleading data, such as a negative purified protein derivative (PPD) skin test despite active infection [3][14]. To avoid delays in diagnosis, there must be increased awareness of the diverse clinical presentations as well as improvements in the diagnostic criteria of Pott’s disease.
In addition to identifying key diagnostic modalities for the detection of Pott’s disease, it is crucial to understand the risk factors in patient populations to identify at-risk individuals and to expand upon the prophylactic measures to reduce the incidence of the disease. Immunodeficiency, most notably human immunodeficiency virus (HIV), as well as vitamin D deficiency, are strongly implicated as risk factors associated with Pott’s disease due to their profound influence on the body’s ability to handle the infective processes of M. tb [15][16].
Pott’s disease has surged in developed nations, especially targeting immunocompromised individuals, due to global migration [17].
2. Pathogenesis and Clinical Presentation of Pott’s Disease
With the recent uptick in the incidence of TB in both developed and developing countries, having an understanding of the rare presentations of TB is increasing in importance [3]. M. tb spreads through aerosol droplets to cause a primary infection in the lungs of the host due to its dependence on oxygen [18]. As seen in Figure 1, M. tb infection has multiple avenues in which it spreads throughout the host [19]. Without proper treatment or detection, the infection may become latent in the lungs or spread via hematogenous dissemination to the extrapulmonary sites of the body [18][20].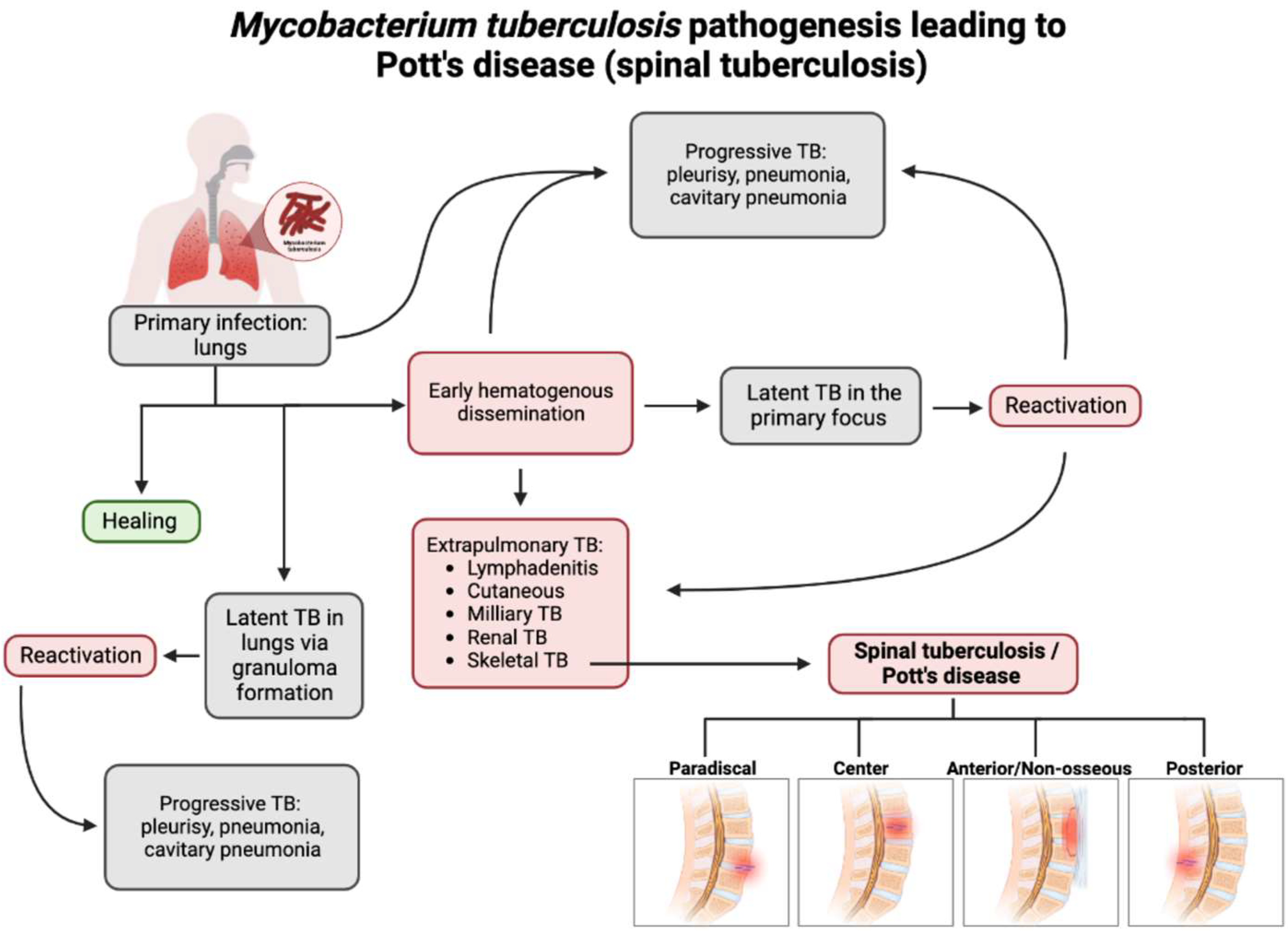
Figure 1. Flow chart depicting the pathogenesis of Pott’s disease. From primary infection, spinal tuberculosis may develop from hematogenous dissemination from the primary infection site and spread to an extrapulmonary site, one of which is the involvement of the skeletal system and, thus, the spine. Following this infection of the spine, spinal TB could present in four major presentations: paradiscal (involves the subchondral space and disc degeneration), central (stems from the center of the vertebral body), anterior/non-osseous (abscess formation between the spinal column and the anterior longitudinal ligament, often spanning multiple segments, sparing bone/disc involvement), and posterior (the infection seeds in the neural arch and posterior aspects of the vertebra). This leads to a compromise and the destruction of the spinal column and causes the classic and atypical presentations of spinal TB/Pott’s disease [3][18][19][20].
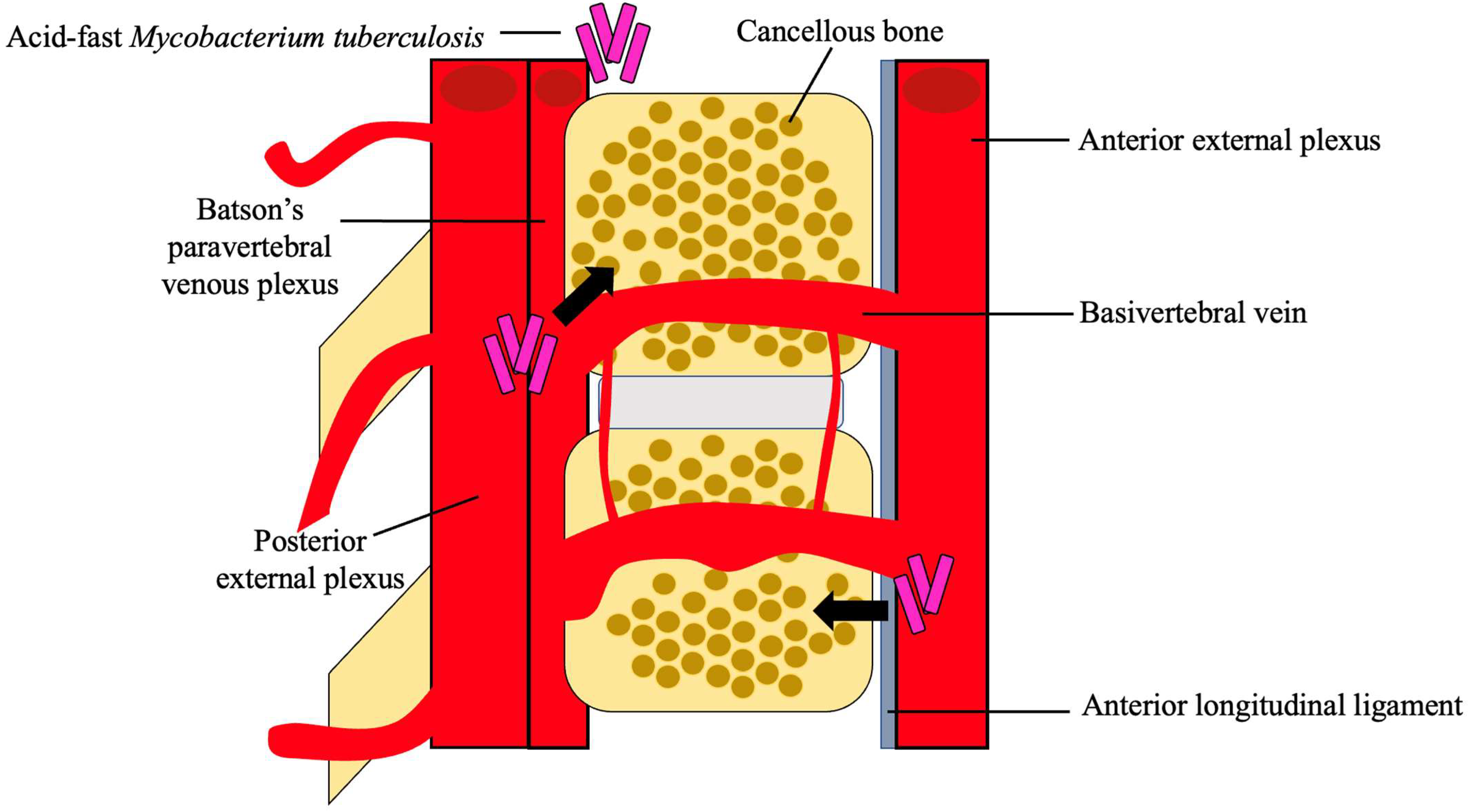
Figure 2. Hematogenous spread of M. tb. M. tb reaches the cancellous bone through the anterior and posterior external venous plexuses. A combination of the valveless Batson’s paravertebral venous plexus and cavity pressures spreads M. tb to the inferior anterior portion of the vertebra and ultimately to the anterior longitudinal ligament where it may disseminate to adjacent vertebra [4][5][18][21].
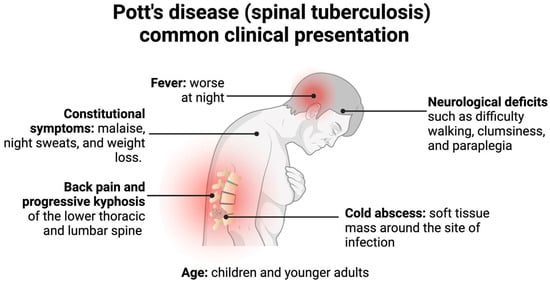
Figure 3. Pott’s disease commonly presents in children or younger adults with back pain, neurological deficits, cold abscesses, and possible kyphotic deformities. Less commonly, patients present with constitutional symptoms and fevers, which generally precede the former symptoms [3][4][5][19][20][25][26].
References
- World Health Organization. Global Tuberculosis Report 2022; World Health Organization: Geneva, Switzerland, 2022.
- MacNeil, A.; Glaziou, P.; Sismanidis, C.; Date, A.; Maloney, S.; Floyd, K. Global Epidemiology of Tuberculosis and Progress Toward Meeting Global Targets—Worldwide, 2018. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 281–285.
- Viswanathan, V.K.; Subramanian, S. Pott Disease. In StatPearls; StatPearls Publishing: Tampa, FL, USA, 2022.
- Garg, R.K.; Somvanshi, D.S. Spinal tuberculosis: A review. J. Spinal Cord Med. 2011, 34, 440–454.
- Ansari, S.; Amanullah, M.F.; Ahmad, K.; Rauniyar, R.K. Pott’s Spine: Diagnostic Imaging Modalities and Technology Advancements. N. Am. J. Med. Sci. 2013, 5, 404–411.
- Colmenero, J.D.; Ruiz-Mesa, J.D.; Sanjuan-Jimenez, R.; Sobrino, B.; Morata, P. Establishing the diagnosis of tuberculous vertebral osteomyelitis. Eur. Spine J. 2013, 22 (Suppl. 4), 579–586.
- Kamara, E.; Mehta, S.; Brust, J.C.M.; Jain, A.K. Effect of delayed diagnosis on severity of Pott’s disease. Int. Orthop. 2012, 36, 245–254.
- McHenry, M.C.; Easley, K.A.; Locker, G.A. Vertebral osteomyelitis: Long-term outcome for 253 patients from 7 Cleveland-area hospitals. Clin. Infect Dis. 2002, 34, 1342–1350.
- Pigrau-Serrallach, C.; Rodriguez-Pardo, D. Bone and joint tuberculosis. Eur. Spine J. 2013, 22 (Suppl. 4), 556–566.
- Solis Garcia del Pozo, J.; Vives Soto, M.; Solera, J. Vertebral osteomyelitis: Long-term disability assessment and prognostic factors. J. Infect. 2007, 54, 129–134.
- Wang, D. Diagnosis of tuberculous vertebral osteomyelitis (TVO) in a developed country and literature review. Spinal Cord 2005, 43, 531–542.
- Kumar, R.; Srivastava, A.K.; Tiwari, R.K. Surgical management of Pott’s disease of the spine in pediatric patients: A single surgeon’s experience of 8 years in a tertiary care center. J. Pediatr. Neurosci. 2011, 6 (Suppl. 1), S101–S108.
- Tuli, S.M. Historical aspects of Pott’s disease (spinal tuberculosis) management. Eur. Spine J. 2013, 22, 529–538.
- Maron, R.; Levine, D.; Dobbs, T.E.; Geisler, W.M. Two cases of pott disease associated with bilateral psoas abscesses: Case report. Spine 2006, 31, E561–E564.
- Bruchfeld, J.; Correia-Neves, M.; Källenius, G. Tuberculosis and HIV Coinfection. Cold Spring Harb. Perspect. Med. 2015, 5, a017871.
- Tang, L.; Liu, S.; Bao, Y.C.; Gao, R.X.; Han, C.F.; Sun, X.C.; Zhang, W.L.; Feng, S.Q. Study on the relationship between vitamin D deficiency and susceptibility to spinal tuberculosis. Int. J. Surg. 2017, 44, 99–103.
- Rajasekaran, S.; Soundararajan, D.C.R.; Shetty, A.P.; Kanna, R.M. Spinal Tuberculosis: Current Concepts. Glob. Spine J. 2018, 8 (Suppl. 4), 96s–108s.
- Khoo, L.T.; Mikawa, K.; Fessler, R.G. A surgical revisitation of Pott distemper of the spine. Spine J. 2003, 3, 130–145.
- Gardini, G.; Gregori, N.; Matteelli, A.; Castelli, F. Mycobacterial skin infection. Curr. Opin. Infect. Dis. 2022, 35, 79–87.
- Rajasekaran, S.; Kanna, R.M.; Shetty, A.P. Pathophysiology and Treatment of Spinal Tuberculosis. JBJS Rev. 2014, 2, e4.
- Weaver, P.; Lifeso, R.M. The radiological diagnosis of tuberculosis of the adult spine. Skelet. Radiol. 1984, 12, 178–186.
- Jung, J.H.; Choi, S.; Kang, Y.; Cho, D.C.; Lee, S.M.; Park, T.I.; Choe, B.H.; Kim, D.; Kang, B. Development of Spinal Tuberculosis in an Adolescent With Crohn’s Disease After Infliximab Therapy: A Case Report With Literature Review. Front. Pediatr. 2021, 9, 802298.
- Kubihal, V.; Sharma, R.; Krishna Kumar, R.G.; Chandrashekhara, S.H.; Garg, R. Imaging update in spinal tuberculosis. J. Clin. Orthop. Trauma 2022, 25, 101742.
- Garg, B.; Mehta, N.; Mukherjee, R.N.; Swamy, A.M.; Siamwala, B.S.; Malik, G. Epidemiological Insights from 1,652 Patients with Spinal Tuberculosis Managed at a Single Center: A Retrospective Review of 5-Year Data. Asian Spine J. 2022, 16, 162–172.
- Jain, A.K.; Rajasekaran, S.; Jaggi, K.R.; Myneedu, V.P. Tuberculosis of the Spine. J. Bone Jt. Surg. Am. 2020, 102, 617–628.
- Nussbaum, E.S.; Rockswold, G.L.; Bergman, T.A.; Erickson, D.L.; Seljeskog, E.L. Spinal tuberculosis: A diagnostic and management challenge. J. Neurosurg. 1995, 83, 243–247.
More
