Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Tommaso Greco and Version 2 by Conner Chen.
Adult acquired flatfoot deformity (AAFD) is a disorder caused by repetitive overloading, which leads to progressive posterior tibialis tendon (PTT) insufficiency. It mainly affects middle-aged women and occurs with foot pain, malalignment, and loss of function. After clinical examination, imaging plays a key role in the diagnosis and management of this pathology. Imaging allows confirmation of the diagnosis, monitoring of the disorder, outcome assessment and complication identification.
- foot and ankle
- adult acquired flatfoot deformity
- progressive collapsing foot deformity
1. Radiography
Radiography is the first-level imaging exam which should be performed in antero-posterior (AP) and lateral weight-bearing (WB) views of both feet (also in case of a unilateral deformity, to compare measurements with normal side), as well as standing AP views of both ankles and the view of Saltzman [1][2]. The X-ray detector and tube should be 35–40 inches apart in both the AP and lateral views of the foot and ankle; furthermore, the beam must be angled at 10° when the AP view of the foot is performed [3]. In Saltzman view, also called hindfoot alignment view, subjects stood on a radiolucent platform with equal weight on both feet. The X-ray tube is oriented 20° from the horizontal, so that it is perpendicular to the plane of the film. The beam is centered at the level of the ankle, and the field of exposure included from midshaft of the tibia to below the calcaneus. Exposure is 62 KV, 6 Mas with a 400 speed, non-grid system using an 11 × 14 in film [2][4].
Numerous radiographic measurements have been proposed for assessing the structural changes associated with adult acquired flatfoot deformity (AAFD)AAFD.
- Talar–first metatarsal angle
- , between the lines drawn along the long axis of the talus and the first metatarsal (normal 0°, flatfoot: mild >4°, moderate >15°, severe >30°) (
- Figure 1
- );
- Talonavicular coverage angle
- , between the line that joins the medial and lateral articular margins of the talus, and the line that joins the medial and lateral articular margins of the navicular, it represents forefoot abduction (normal, <7°; flatfoot, >7°) (
- Figure 2
- );
- Talonavicular uncoverage percentage
- , the percentage of the talus that is not in contact with the navicular medially, useful to evaluate forefoot abduction (normal, 10% to 30%; flatfoot >30%) (
- Figure 3
- );
- Talar incongruency angle
- (normal, 5° = –26°; flatfoot >26°), is formed by the intersection between a line from the most lateral point of the articular surfaces of the talus and the navicular, and a line from the lateral aspect of the talar neck (in its most narrow segment) to the lateral point of the talar articular surface (
- Figure 4
- ).
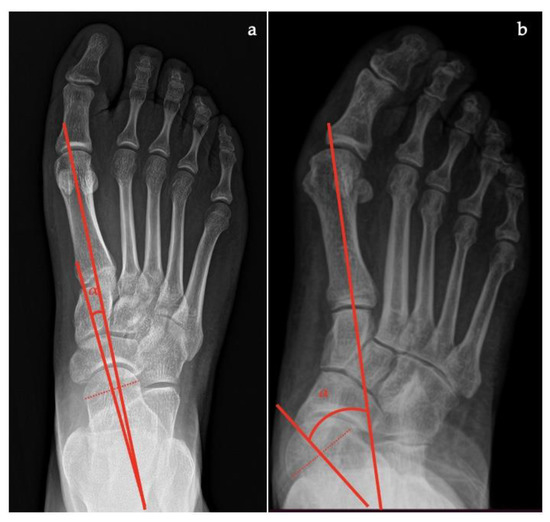
Figure 1. Taler-first metatarsal angle in the anteroposterior view (between the long axis of the talus and the long axis of the first metatarsal). (a) Normal foot, 3°; (b) pathological flatfoot, 30°.

Figure 2. Talonavicular coverage angle (between the line that joins the medial and lateral articular margins of the talus, and the line between that joins the medial and lateral articular margins of the navicular). (a) Normal foot, 2°; (b) pathological flatfoot, 35°.

Figure 3. Talonavicular uncoverage percentage (percentage of the talus that is not in contact with the navicular medially). (a) Normal foot, <30%; (b) pathological flatfoot, >30%.

Figure 4. Talar incongruency angle (formed by the intersection between a line from the most lateral point of the articular surfaces of the talus and the navicular, and a line from the lateral aspect of the talar neck (in its most narrow segment) to the lateral point of the talar articular surface). (a) Normal foot, 6°; (b) pathological flatfoot, >30°.
- Talar–first metatarsal angle (Meary’s angle), the normal value is 0 ± 10 degrees and is increased in flatfoot deformity (often >20°, apex directed plantarly) (Figure 5);
- Calcaneal pitch, the angle between the line parallel to the ground and the line along the inferior inclination axis of the calcaneus (normal, 20–30°; flatfoot, <20°) (Figure 6);
- Talocalcaneal angle is formed by the long axis of the rearfoot and the midtalar line. This angle is increased in pronated feet on both the AP and lateral views (normal <45°, flatfoot >45°) (Figure 7);
- Calcaneal-fifth metatarsal angle, defined as the angle formed between the tangent to the inferior aspect of the calcaneus and a line drawn along the inferior aspect of the base and head of the fifth metatarsal (normal <170°, flatfoot >170°) (Figure 8).
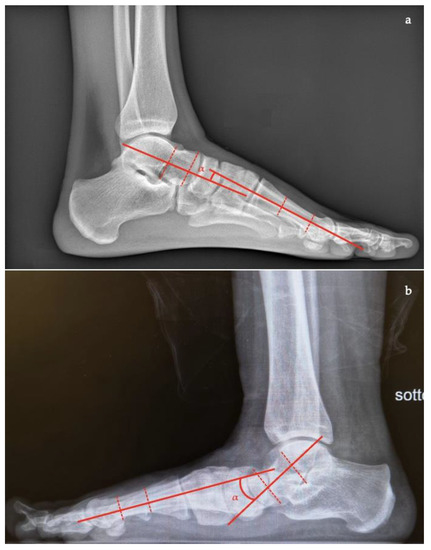
Figure 5. Talar-first metatarsal angle in the lateral view (Meary’s angle, the angle between the long axis of the talus and the long axis of the first metatarsal). (a) Normal foot, 4°; (b) pathological flatfoot, 30°.

Figure 6. Calcaneal pitch (formed by the line parallel to the ground and the line along the inferior inclination axis of the calcaneus) in the lateral X-ray view. (a) Normal foot, 30°; (b) pathological flatfoot, 10°.

Figure 7. Talocalcaneal angle (formed by the long axis of the rearfoot and the midtalar line) in lateral X-ray view. (a) Normal foot, 45°; (b) pathological flatfoot, 52°.
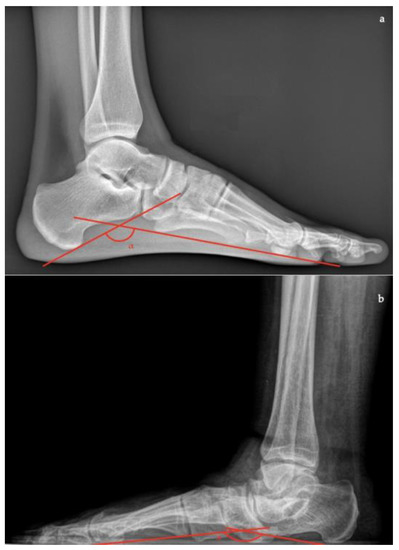
Figure 8. Calcaneal-fifth metatarsal angle (defined as the angle formed between the tangent to the inferior aspect of the calcaneus and a line drawn along the inferior aspect of the base and head of the fifth metatarsal) in the lateral X-ray view. (a) Normal foot, 145°; (b) pathological flatfoot, 175°.
In Saltzman view (Figure 9):
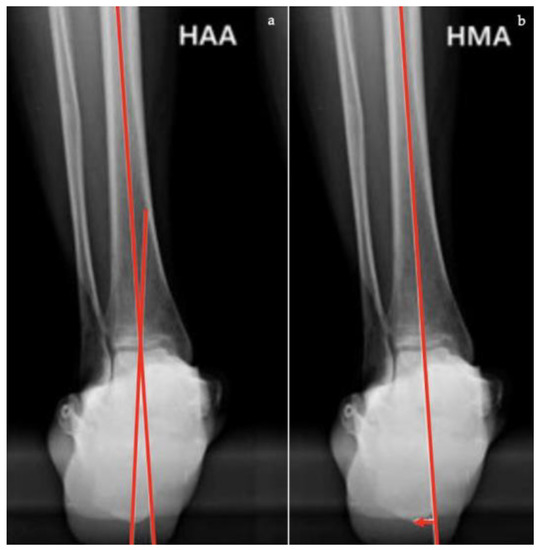
Figure 9. Saltzman view. (a) Hindfoot Alignment Angle (HAA) (formed by the intersection of the longitudinal axis of the tibial shaft and the axis of the calcaneal tuberosity). (b) Hindfoot Moment Arm (measured by the shortest distance between the midtibial axis and the most inferior portion of the calcaneus gus, represented by the red arrow).
- Hindfoot moment arm, measured by the shortest distance between the midtibial axis and the most inferior portion of the calcaneus gus (normal, −3 mm to +10 [varus]; flatfoot, >+10 mm [valgus]);
- Hindfoot alignment angle, formed by the intersection of the longitudinal axis of the tibial shaft and the axis of the calcaneal tuberosity (normal, 5.6 ± 5.4°; flatfoot, 22.5 ± 4.9°) [9].
Considering their widespread use in clinical practice, many studies have tried to quantify the reliability of the angular measurements using this conventional imaging. Sensiba et al. [10] investigated the intra- and inter-observer reliability using three digital radiographs consisting of AP, lateral, and hindfoot alignment, varying levels of observer experience. Intra-observer reliability increased with observer experience. Nevertheless, traditional images are not able to show soft tissue involvement or bone oedema. Other radiographic techniques are often necessary to establish the etiology of the disease and the preoperative planning [11].
The radiographic study was also useful for assessing post-operative outcomes, although the different measurements showed different reliability depending on the corrective surgical technique used [12].
2. Magnetic Resonance Imaging (MRI)
MRI is useful to analyze tendon involvement, soft tissue, and bone structures, allowing the study of the physiopathology of AAFD [5][13][14]. A common incidental finding of MRI is the lateral ankle ligament injury which is secondary to the biomechanical changes within the foot and increases stress placed on the soft tissues surrounding both ankle and subtalar joints, causing pain [15].
MRI protocols should include standard sequences for studying the ankle such as sagittal T1-weighted spin-echo, sagittal fast spin-echo short tau inversion recovery (STIR), axial proton-density weighted, axial T2-weighted fast spin echo fat-saturated, and coronal proton-density weighted fat-saturated. High field strength 1.5T or 3T scanners and dedicated extremity coils provide adequate signal-to-noise ratio and the spatial resolution required for proper imaging of the complex anatomy of the ankle [3].
2.1. Posterior Tibial Tendon
2.2.1. Posterior Tibial Tendon
MRI is the preferred modality for assessment of the posterior tibialis tendon (PTT)PTT (Figure 10a) and it has a good accuracy in showing tendon abnormalities, with a sensitivity of up to 95% and a specificity of 100% in the detection of the rupture of the PTT [16]. The PTT can be affected by degenerative tendinosis, tenosynovitis, and a partial or complete tear. PTT tendinosis can be diagnosed with increased signal intensity in the tendon with preservation of the normal shape; tenosynovitis (isolated) is documented if there is a high fluid signal intensity surrounding 50% or more of the PTT circumference with normal size, shape, and intrinsic low signal. A PTT tear is identified with increased T2 and T1 signal intensity and enlargement of the tendon, defects in the tendon, a linear fluid signal in the tendon (longitudinal split tear) or a lack of continuous tendon fibres (complete rupture) [3].
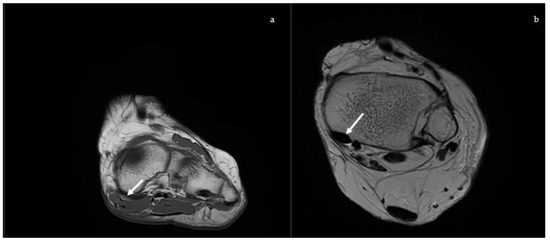
Figure 10. Magnetic Resonance Imaging. (a) Coronal T1: soft tissue involvement of the posterior tibial tendon, (b) Axial T2: superomedial fibers of the spring ligament (white arrow).
2.2. Spring Ligament
The spring ligament (Figure 10b), also known as the plantar calcaneo-navicular ligament, is considered the primary static stabilizer of the medial arch and is second in importance only to the PTT [5]. The superomedial component of the spring ligament complex is the largest and most important part and constitutes a structure that supports the talar head and talonavicular joint and separates the PTT from the talus bone. When it is injured or released and cyclically loaded, it leads to a weakening of other structures, resulting in a plano-valgus deformity [17]. MRI is useful to study the injuries of this ligament and their severity. Diagnostic MRI findings include abnormally high signal intensity on T2-weighted or proton density images, thickening (>5–6 mm), thinning (<2 mm), waviness, and discontinuity [18]. Ormsby et al. showed that in the progression of injury related to AAFD, the dorsal talonavicular component of the tibio-navicular ligament can be involved and it can be well shown by new MRI sequences, which consists of an axial oblique proton dense fat suppressed sequence with 3-mm (0.3 mm gap) slices at 30° to the axial plane along the tibionavicular portion of the deltoid complex [19].
3. Ultrasound (US)
US is an inexpensive but operator-dependent investigation, assessing PTT, spring ligament status (Figure 11) and foot anatomy-functional changes [20], with similar accuracy to MRI [7]. Dynamic Mode can be useful in patients with suspected friction syndrome [5], at a thickened retinaculum and tendon instability related to flexor retinaculum disruption, which fosters anterior tendon subluxation.
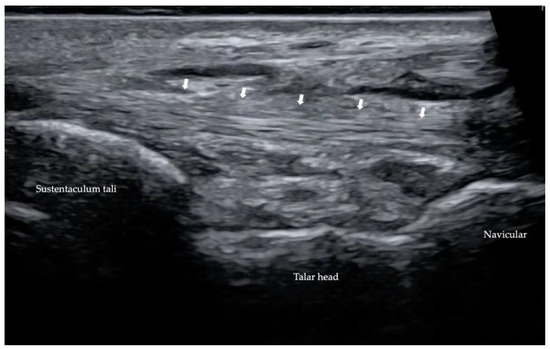
Figure 11.
Ultrasonography of spring ligament (marked by white arrows).
4. Computed Tomography (CT)
CT provides advanced and detailed visualization of the hindfoot and it is useful in the evaluation of bone abnormalities, such as arthritis, tarsal coalitions, and fracture malunions [21]. However, with the traditional CT, images can be obtained only offload. In patients with AAFD, hindfoot instability and alignment have been better observed during WB [22]. Recent developments in CT scan design have contributed to the advent of Cone-beam computed tomography (CBCT) which allows imaging of lower extremities in a normal upright WB. CBCT uses a large-area detector and a pyramid-shaped X-ray beam, obtaining fully volumetric data from multiple projections acquired in a single rotation about the patient without moving the patient through the scanner [23].
Through CT scans, numerous measurements, which can also be calculated with X-ray, can be obtained with a higher level of accuracy [11].
In the axial plane (Figure 12):
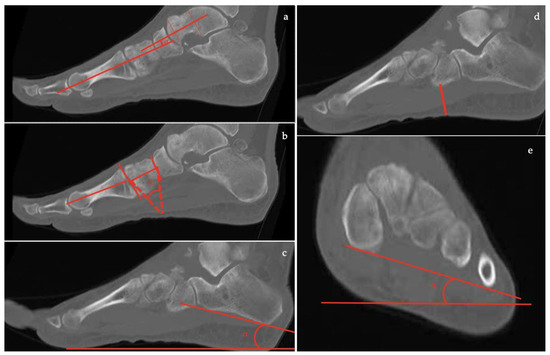
Figure 12. Computed Tomography (CT) imaging: (a) Talar–first metatarsal angle (Meary’s angle), (b) Medial Cuneiform-First metatarsal angle, (c) Calcaneal inclination angle, (d) Cuboid to floor distance, (e) Forefoot arch angle.
- the talar-first metatarsal angle;
- the talonavicular coverage angle.
In the coronal plane, nine parameters can be evaluated:
- the forefoot arch angle;
- the navicular-to-skin distance;
- the navicular-to-floor distance;
- the medial cuneiform-to-skin distance;
- the medial cuneiform-to-floor distance;
- the calcaneofibular distance;
- the subtalar horizontal angle, which is the angle between the posterior facet of the talus and the floor measured at 25% (posterior aspect), at 50% (midpoint), and at 75% (anterior aspect) of the posterior subtalar joint length.
In the sagittal plane, eight parameters can be assessed:
- the talus-first metatarsal angle;
- the navicular-to-skin distance;
- the navicular-to-floor distance;
- the cuboid-to-skin distance;
- the cuboid-to-floor distance;
- the medial cuneiform-to-skin distance;
- the medial cuneiform-to-floor distance;
- the calcaneal inclination angle.
References
- Lee, M.S.; Vanore, J.V.; Thomas, J.L.; Catanzariti, A.R.; Kogler, G.; Kravitz, S.R.; Miller, S.J.; Gassen, S.C. Diagnosis and Treatment of Adult Flatfoot. J. Foot Ankle Surg. 2005, 44, 78–113.
- Saltzman, C.L.; El-Khoury, G.Y. The Hindfoot Alignment View. Foot Ankle Int. 1995, 16, 572–576.
- Lin, Y.-C.; Mhuircheartaigh, J.N.; Lamb, J.; Kung, J.W.; Yablon, C.M.; Wu, J.S. Imaging of Adult Flatfoot: Correlation of Radiographic Measurements With MRI. Am. J. Roentgenol. 2015, 204, 354–359.
- Neri, T.; Barthelemy, R.; Tourné, Y. Radiologic Analysis of Hindfoot Alignment: Comparison of Méary, Long Axial, and Hindfoot Alignment Views. Orthop. Traumatol. Surg. Res. 2017, 103, 1211–1216.
- Flores, D.V.; Mejía Gómez, C.; Fernández Hernando, M.; Davis, M.A.; Pathria, M.N. Adult Acquired Flatfoot Deformity: Anatomy, Biomechanics, Staging, and Imaging Findings. RadioGraphics 2019, 39, 1437–1460.
- Henry, J.K.; Shakked, R.; Ellis, S.J. Adult-Acquired Flatfoot Deformity. Foot Ankle Orthop. 2019, 4, 247301141882084.
- Abousayed, M.M.; Alley, M.C.; Shakked, R.; Rosenbaum, A.J. Adult-Acquired Flatfoot Deformity: Etiology, Diagnosis, and Management. JBJS Rev. 2017, 5, e7.
- Perez Boal, E.; Becerro de Bengoa Vallejo, R.; Fuentes Rodriguez, M.; Lopez Lopez, D.; Losa Iglesias, M.E. Geometry of the Proximal Phalanx of Hallux and First Metatarsal Bone to Predict Hallux Abducto Valgus: A Radiological Study. PLoS ONE 2016, 11, e0166197.
- Cody, E.A.; Williamson, E.R.; Burket, J.C.; Deland, J.T.; Ellis, S.J. Correlation of Talar Anatomy and Subtalar Joint Alignment on Weightbearing Computed Tomography with Radiographic Flatfoot Parameters. Foot Ankle Int. 2016, 37, 874–881.
- Sensiba, P.R.; Coffey, M.J.; Williams, N.E.; Mariscalco, M.; Laughlin, R.T. Inter- and Intraobserver Reliability in the Radiographic Evaluation of Adult Flatfoot Deformity. Foot Ankle Int. 2010, 31, 141–145.
- de Cesar Netto, C. Flexible Adult-Acquired Flatfoot Deformity: Comparison Between Weight Bearing and Non-Weight Bearing Measurements Using Cone Beam Computed Tomography. In Weight Bearing Cone Beam Computed Tomography (WBCT) in the Foot and Ankle; Springer International Publishing: Cham, Switzerland, 2020; pp. 181–198. ISBN 978-3-030-31948-9.
- Conti, M.S.; Garfinkel, J.H.; Ellis, S.J. Outcomes of Reconstruction of the Flexible Adult-Acquired Flatfoot Deformity. Orthop. Clin. N. Am. 2020, 51, 109–120.
- Polichetti, C.; Greco, T.; Inverso, M.; Maccauro, G.; Forconi, F.; Perisano, C. Retro-Malleolar Z-Plasty of Flexor Hallucis Longus Tendon in Post-Traumatic Checkrein Deformity: A Case Series and Literature Review. Medicina 2022, 58, 1072.
- Perisano, C.; Greco, T.; Vitiello, R.; Maccauro, G.; Liuzza, F.; Tamburelli, F.C.; Forconi, F. Mueller-Weiss Disease: Review of the Literature. J. Biol. Regul. Homeost. Agents 2018, 32 (Suppl. S1), 157–162.
- Persaud, S.; Hentges, M.J.; Catanzariti, A.R. Occurrence of Lateral Ankle Ligament Disease with Stage 2 to 3 Adult-Acquired Flatfoot Deformity Confirmed via Magnetic Resonance Imaging: A Retrospective Study. J. Foot Ankle Surg. 2019, 58, 243–247.
- Rosenberg, Z.S.; Cheung, Y.; Jahss, M.H.; Noto, A.M.; Norman, A.; Leeds, N.E. Rupture of Posterior Tibial Tendon: CT and MR Imaging with Surgical Correlation. Radiology 1988, 169, 229–235.
- McCormack, A.P.; Niki, H.; Kiser, P.; Tencer, A.F.; Sangeorzan, B.J. Two Reconstructive Techniques for Flatfoot Deformity Comparing Contact Characteristics of the Hindfoot Joints. Foot Ankle Int. 1998, 19, 452–461.
- Kimura, Y.; Yamashiro, T.; Saito, Y.; Kitsukawa, K.; Niki, H.; Mimura, H. MRI Findings of Spring Ligament Injury: Association with Surgical Findings and Flatfoot Deformity. Acta Radiol. Open 2020, 9, 205846012098014.
- Ormsby, N.; Jackson, G.; Evans, P.; Platt, S. Imaging of the Tibionavicular Ligament, and Its Potential Role in Adult Acquired Flatfoot Deformity. Foot Ankle Int. 2018, 39, 629–635.
- Lobo, C.C.; Marín, A.G.; Sanz, D.R.; López, D.L.; López, P.P.; Morales, C.R.; Corbalán, I.S. Ultrasound Evaluation of Intrinsic Plantar Muscles and Fascia in Hallux Valgus: A Case-Control Study. Medicine 2016, 95, e5243.
- Meehan, R.E.; Brage, M. Adult Acquired Flat Foot Deformity: Clinical and Radiographic Examination. Foot Ankle Clin. 2003, 8, 431–452.
- de Cesar Netto, C.; Shakoor, D.; Dein, E.J.; Zhang, H.; Thawait, G.K.; Richter, M.; Ficke, J.R.; Schon, L.C.; Demehri, S.; Richter, M.; et al. Influence of Investigator Experience on Reliability of Adult Acquired Flatfoot Deformity Measurements Using Weightbearing Computed Tomography. Foot Ankle Surg. 2019, 25, 495–502.
- Carrino, J.A.; Al Muhit, A.; Zbijewski, W.; Thawait, G.K.; Stayman, J.W.; Packard, N.; Senn, R.; Yang, D.; Foos, D.H.; Yorkston, J.; et al. Dedicated Cone-Beam CT System for Extremity Imaging. Radiology 2014, 270, 816–824.
More
