Involvement of the immune system in biological therapies specifically targeting tumor microenvironment has been suggested. Substantial advancement in the treatment of malignant tumors utilizing immune cells, most importantly T cells that play a key role in cell-mediated immunity, have led to success in clinical trials.
- tumor microenvironment
- cancer vaccines
- tumor-infiltrating lymphocytes
- combination therapy
- checkpoint-inhibitors
- CAR T cell therapy
1. Tumor Microenvironment in Cancer
2. Immunomodulatory Roles of Lymphangiogenesis in TME
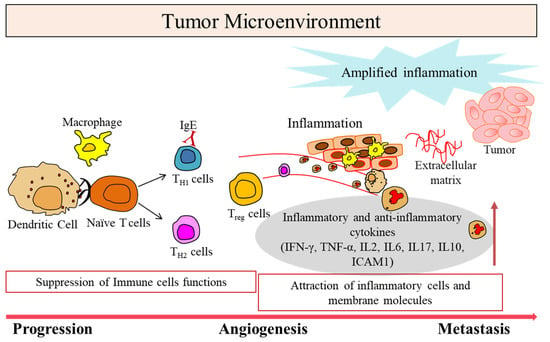
Significant role of lymphatic vessels in the tumor microenvironment is known to promote tumor metastasis in many cancers by undergoing activation, hyperplasia, and lymphangiogenesis in the tumor microenvironment and in the tumor-draining lymph node. Lymphatic vessels were considered passive participants in tumor progression and metastasis by simply providing a physical route for tumor cells dissemination to draining lymph nodes. However, recent studies have highlighted new roles of the lymphatic endothelium in regulating host immunity by identifying several key lymphatic-specific molecular markers, and a complex array of lymphangiogenic factors, chemokines, and immune cell subsets [8][13]. Accumulation of immune cells during the process of angiogenesis in TME is mediated by several growth factors, such as vascular endothelial growth factor A (VEGFA), PDGF, epidermal growth factor (EGF), IL-6 and IL-8 [9][14]. Other prolymphangiogenic factors identified were VEGFC and VEGFD, which bind to the receptors present on the lymphatic endothelium such as tyrosine kinase receptors and VEGF receptors (R)–3 [10][11][12][13][15,16,17,18]. Neuropilin receptor-2 (Nrp-2) is a coreceptor for VEGF receptor signaling by enhancing the binding between VEGF ligands and receptors [14][15][19,20]. Lymphatic vasculature helps in trafficking of immune cells from peripheral tissues to lymph nodes through the signaling of chemokines, where adaptive immune responses are instigated. Chemokines are crucial for providing navigational cues to migrating cancer cells by facilitating tumor growth by promoting EMT as well as angiogenesis. It is generally accepted that the expression of certain chemokine receptors on the surface of the cancer cells promotes metastasis and organ-specific metastasis. For example, the pattern of breast cancer metastasis is largely determined by the interaction between the chemokine receptors on cancer cells and the chemokines expressed. Chemokine receptors CXCR4 and CCR7 ligands (CXCL12 is also referred to as stromal cell-derived factor-1 [SDF-1] and CCL21) are widely expressed on human breast cancer cells and on the organs that tumors normally metastasize [16][25]. Several reports elucidated that tumor-associated lymphatic vessels, but not normal lymphatic vessels, express a high concentration of CXCL12, highlighting an active role for the tumor-associated lymphatic endothelium in metastatic tumor spread [17][18][19][20][26,27,28,29] (Figure 2). The chemokines CCL19 and CCL21 ligands for CCR7 are important for active metastatic dissemination of malignant cells via the lymphatic system. This suggests lymphatic vessels and lymphangiogenesis play important immunomodulatory roles in the tumor microenvironment.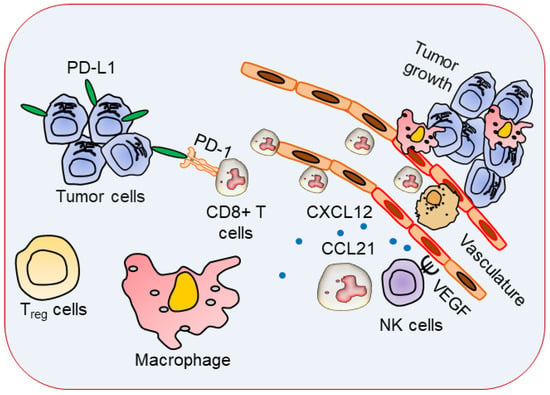
3. Immune Cells with Specific Phenotypes in TME
Cancer biomarkers help in characterizing alterations in the tumor. A number of genes associated with lymphocyte regulation, cytokine signaling, lymphocyte markers, checkpoint pathways, and tumor characterization have been identified as a predictive biomarker for cancer. The majority of tumors show evidence of a T-cell-infiltrated phenotype. TME and the immune system play critical roles in cancer progression and clinical outcome where regulatory (Treg) and effector T cells’ infiltration contributes to the maintenance of self-tolerance and an immune-homeostasis-creating immunosuppressive environment by suppressing antitumor immunity in the TME. T-cell-inflamed TME is characterized by the elevated expression of type 1 interferon, as well as promigratory chemokines that result in the recruitment of activated CD8+ effector T cells into the tumor parenchyma [21][30]. Anticancer can be segregated into three main phenotypes: the immune-excluded phenotype, the immune-desert phenotype, and the inflamed phenotype. An immune-excluded tumor represents a specific chemokine state that is characterized by the presence of different immune cell types in the aggressive margin or stroma of the tumor but cannot infiltrate into the tumor parenchyma [22][23][31,32]. On the contrary, the immune-desert phenotype is caused by immunological ignorance, which is characterized by the absence of appropriate T cell priming or activation in the parenchyma or stroma of the tumors and poor response to immune checkpoint inhibitors treatment [24][25][33,34]. Inflamed tumors are highly infiltrated with number of immune cells subtypes, including immune-inhibitory regulatory T cells, myeloid-derived suppressor cells, suppressor B cells, and cancer-associated fibroblasts. It contains proinflammatory cytokines that should provide a more favorable environment for T cell activation and expansion [26][35]. Therefore, utilizing the role of cytotoxic T cells to kill cancer cells can be an effective immunotherapy. The presence of activated CD8+ T cells, both within the tumor and in the peritumoral stroma, has been shown to have significant positive prognostic import [27][28][36,37]. A high ratio of CD8+ T cells to Foxp3+ regulatory T cells (Treg) in the ovarian cancer tumor microenvironment has been associated with a particularly favorable clinical outcome [29][38]. A substantial body of evidence suggests that NK cells contribute to host control of hematologic malignancies and contribute to tumor control in solid tumors [30][31][32][44,46,47]. Association between TAMs and anti-PD-1 response has been reported in melanoma cases. It has been established that the association between Fcγ receptor (FcγR), expressed by the host bone marrow cells and Fc domain glycan of the drug, could determine the ability of PD-1-TAMs to capture anti-PD-1 drugs from the surface of T cells, leading to PD-1 inhibitor resistance [33][34][48,49]. In addition, anti-PD-1 response also affect cytotoxic T cells, indicating an increase in CD8+ T cells and NK cells and a decrease in macrophages [25][35][36][34,50,51]. Recently, a study conducted by Crist et. al. has shown that the antidiabetic agent metformin slows tumor growth and progression in vitro and in combination with chemoradiotherapy in patients suffering from head and neck cancer squamous cell carcinoma (HNSCC) in their phase 1 clinical trial (NCT02325401). It increases the activated peripheral NK cell populations, enhanced HNSCC NK cell cytotoxicity, and inhibited the CXCL1 pathway while stimulating the STAT1 pathway [37][52]. It also influences anticancer immunity in esophageal squamous cell carcinoma (ESCC) in both humans and mice, via triggering an AMPK activation and STAT3 inactivation. In clinical trials, low-dose metformin recruits a greater number of CD8+ cytotoxic T lymphocyte and CD20+ B lymphocyte while enhancing tumor-suppressive (CD11c+) and reducing tumor-promoting (CD163+) macrophages in TME [38][53]. In addition to this strategy, mannose-modified, macrophage-derived microparticles (Man-MPs) loading metformin (Met@Man-MPs) were used to effectively target M2-like TAMs to transform them into M1-like phenotypes. This strategy reprogrammed the TME towards an inflamed anti-tumor microenvironment by increasing the recruitment of CD8+ T cells. The Met@Man-MPs approach boosted the anti-PD-1 antibody therapy and developed long-term memory immunity [39][54]. Interestingly, the anti-tumor efficacy of the PD-L1 depression strategy was found to be superior to the conventional anti-PD-L1 therapy in terms of selectivity and efficacy. This group has developed a mitochondria-oxidative phosphorylation (OXPHOS) depression nanosystem using IR-LND (conjugate of mitochondria-targeted heptamethine cyanine dye IR-68 with mitochondrial complexes I and II depression agent lonidamine (LND)) assembled with albumin (Alb) to form IR-LND@Alb nanoparticles [40][55]. Another promising therapy that has the same limitation of causing severe hypoxia and PD-L1 over-expressed immunosuppressed TME is photodynamic therapy (PDT). The drawback of regular chemotherapy is increased in the expression of PD-L1 in almost all kinds of cancers, causing reduced efficacy of T-cell-mediated immune killing in tumors. Recently, chitosan oligosaccharide (COS), a biomaterial derived from the N deacetylation product of chitin, has been found to inhibit the upregulated PD-L1 expression. Due to the property of COS to significantly restrict the growth of CT26 tumors, it has been combined with Gemcitabine (GEM), one of the typical chemotherapeutic drugs, leading to a more remarkable tumor remission [41][58]. In conclusion, targeting immune cells in TME could be a great predictive biomarker for immune checkpoint inhibitors.4. Cancer Immunotherapy
Cancer immunotherapies involving T lymphocyte have become a primary goal for engaging the immune system in fighting cancer (Figure 3). Therefore, recent studies are emphasizing the ability of T cells to promote cancer treatments involving checkpoint blockade, adoptive cellular therapy, and cancer vaccinology [42][43][44][45][59,60,61,62]. Cancer vaccines boost the immune system to mount an attack against cancer cells (see the current status of cancer immunotherapies available in Table 1 and Table 2). By default, the immune system responds chemotactically to the known or self-substance to work normally in our system, whereas it signals a danger when it encounters a non-self or foreign substance. Cancer cells express certain molecules called cancer-specific antigens, neoantigens, or tumor associated antigens (TAAs) on their surface that healthy cells do not express. These TAAs are recognized by cytolytic T lymphocytes (CTL). A melanoma-associated antigen, MZ2-E, which is a rejection antigen that is recognized by the patients’ autologous, tumor-directed and specific cytolytic, CD8+ CTL [46][63]. The association of the antigen MZ2-E with the HLA-A1 molecule was confirmed by a nonapeptide which was recognized by CTL when it was presented by mouse cells transfected with an HLA-A1 gene [47][64]. The advantage of a higher expression of TAAs on tumor cells and minimally on normal tissues can be utilized in creating therapeutic vaccine-based approaches [46][63]. Boosting immune effector mechanisms to specifically target cancer cells may be utilized to inhibit the further growth of advanced cancers. Historically, vaccination approaches in the 1970s were based on autologous tumor vaccines prepared using patient-derived tumor cells. These tumor cells were irradiated and administered together with an adjuvant or virus to the individual from whom the tumor cells were isolated to stimulate immune responses [48][65]. Unfortunately, this approach faces multiple limitations due to nonavailability of tumor specimens, most notably in non-small cell lung cancer (NSCLC) [49][66]. Vaccines should fulfill the criteria of eliciting more robust immune responses without causing autoimmune-related toxicities. Therefore, it is urgent to find newer approaches to progress cancer treatment better, with high efficacies and enhanced overall survival.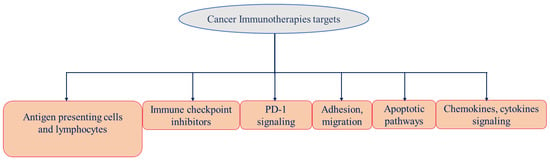
|
Target |
|
|---|---|
|
Small Drugs Based | Drug INN (Brand Name) |
Cancer Type |
Current Status |
Ref. |
|||||
|---|---|---|---|---|---|---|---|---|---|
|
Antibodies Based |
|||||||||
|
Target |
Drug INN (Brand Name) |
Cancer Type |
Current Status |
Ref. |
|||||
|
CTLA-4 |
Ipilimumab (Yervoy) |
Melanoma (2011) and Renal cell carcinoma (2018) |
|||||||
|
EGFR |
Gefitinib | FDA approved |
NSCLC (2015) |
FDA approved |
|||||
[ | ] |
Multiple cancers |
Phase I-III |
||||||
|
Erlotinib HCl (Tarceva) |
NSCLC (2004) |
FDA approved |
Tremelimumab (Imjudo) |
Antineoplastic; liver cancer |
FDA approved | ||||
|
Osimertinib mesylate |
NSCLC (2020) |
FDA approved [52][ |
|||||||
, | ] |
PD-1 |
|||||||
|
Dacomitinib (Vizimpro) |
Nivolumab (Opdivo) |
EGFR-mutated NSCLC (2018) Melanoma (2014), NSCLC (2015), and Renal (2018) cancers, Hodgkin lymphoma |
FDA approved FDA approved |
||||||
|
Multiple cancers |
Phase I-III |
||||||||
|
Pembrolizumab (Keytruda) |
Melanoma (2014), Various (2015) |
FDA approved |
|||||||
|
Multiple cancers |
Phase I-III |
||||||||
|
MED10680 |
Multiple cancers |
Phase I |
|||||||
|
AMP-224 |
Multiple cancers |
Phase I |
|||||||
|
Pidilizumab |
Multiple cancers |
Phase I-II |
|||||||
|
Cemiplimab (Libtayo) |
Cutaneous squamous-cell carcinoma (2018) |
FDA approved |
|||||||
|
PD-L1 |
Atezolizumab (Tecentriq) |
Bladder, NSCLC (2016), and TNBC (2019), hepatocellular carcinoma, HCC (2020) |
FDA approved |
||||||
|
Avelumab (Bavencio) |
Urothelial Carcinoma (2017), Merkel Cell Carcinoma (2017), Renal carcinoma (2019) |
FDA approved |
|||||||
|
MED14736 |
Multiple cancers |
Phase III |
|||||||
|
Avelumab (Bavencio) |
Merkel cell carcinoma (2017), Rena (2019), Urothelial carcinoma (2020) |
FDA approved |
|||||||
|
BMS-936559 |
Multiple cancers |
Phase I |
|||||||
|
Durvalumab (IMFINZI) |
Bladder Cancer (2017), NSCLC (2018) |
FDA approved |
|||||||
[ | ][80] |
LAG-3 |
|||||||
|
Multitarget TKI (VEGFR2/3, EGFR, and RET) | IMP321 |
Vandetanib (Caprelsa) Multiple cancers |
Phase I |
Unresectable or metastatic medullary thyroid cancer (2011) [ |
FDA approved |
||||
[ | ] |
BMS-986016 |
|||||||
|
Multitarget TKI (VEGFRs, MET, RET, FLT3, KIT, TIE2, and AXL) |
Multiple cancers |
Phase I |
[52] |
Cabozantinib S-malate (Cometriq)[69] |
|||||
Progressive, metastatic medullary thyroid cancer (2012) |
Relatlimab (Opdualag) |
Melanoma (2022) |
FDA approved |
||||||
|
VEGFRs |
Axitinib (Inlyta) |
Advanced RCC (2012) |
FDA approved |
VEGF |
Bevacizumab |
Colorectal (2004), NSCLC (2006, 2018), Renal (2009), Cervical (2014), Glioblastoma (2009), and Ovarian (2018) Cancers |
FDA approved |
||
|
Tivozanib HCl (Fotivda) |
Advanced RCC (2021) |
FDA approved | |||||||
|
VEGF-A, Ang-2 |
Faricimab (Vabysmo) |
wAMD, DME |
FDA approved |
||||||
|
mTOR |
Everolimus (Afinitor) |
Advanced RCC (2009), HER2-negative breast cancer after failure of treatment with letrozole or anastrozole (2012), nonfunctional neuroendocrine tumors of gastrointestinal or lung origin with unresectable, locally advanced, or metastatic disease (2016) |
VEGFR2 |
Ramucirumab (Cyramza) |
Gastric cancer (2014), NSCLC (2020), HCC (2019) |
FDA approved |
|||
|
EGFR |
Cetuximab |
Colorectal cancer (CRC) (2004, 2012) and Head and neck squamous cell carcinoma (2006, 2011) |
FDA approved |
||||||
|
Necitumumab (Portrazza) |
NSCLC (2015) |
FDA approved |
76] |
||||||
|
Mobocertinib succinate (Exkivity) |
EGFR exon 20-mutated NSCLC (2021) |
FDA approved |
63][ | ||||||
|
HER2 |
Tucatinib (Tukysa) |
HER2-positive breast cancer (2020) | ,80] |
||||||
|
EGFR, HER2, and HER4 |
Neratinib maleate (Nerlynx) |
HER2-overexpressed breast cancer (2017) |
FDA approved |
||||||
|
Afatinib dimaleate (Gilotrif) |
Metastatic NSCLC with EGFR exon 19 deletion or exon 21 (L858R) mutation (2013) |
FDA approved |
|||||||
] |
Panitumumab (Vectibix) |
Fam-trastuzumab deruxtecan (Enhertu) |
HER2-positive Breast cancer (2019) |
FDA approved |
|||||
|
Trastuzumab tucatinib |
HER2-positive Breast cancer (2020) |
FDA approved |
|||||||
|
CCR4 |
Mogamulizumab (Poteligeo) |
Cutaneous T cell lymphoma (2018) |
FDA approved |
||||||
|
CD20 |
Obinutuzumab (Gazyva) |
Chronic lymphocytic leukemia (2013), follicular lymphoma (2017) |
FDA approved |
||||||
|
Ofatumumab (Arzerra) |
Chronic lymphocytic leukemia (2014) |
FDA approved |
|||||||
|
Rituximab (MabThera, Rituxan) |
B-Cell Lymphoma (1997) |
FDA approved |
|||||||
|
Ibritumomab tiuxetan (Zevalin) |
NHL (2004) |
FDA approved |
|||||||
|
tositumomab Iodine-131 (Bexxar) |
NHL (2003) |
FDA approved |
|||||||
|
Ublituximab |
Chronic lymphocytic leukemia, CLL, non-Hodgkin’s lymphoma) and non-cancer (multiple sclerosis) |
Phase III |
|||||||
|
CD33 |
Gemtuzumab ozogamicin (Mylotarg) |
Acute myeloid leukemia (2000) |
FDA approved |
||||||
|
CD30 |
Brentuximab vedotin (Adcetris) |
Hodgkin’s lymphoma and Anaplastic large-cell lymphoma (2011) |
FDA approved |
||||||
|
CD79B |
Polatuzumab vedotin (Polivy) |
Diffuse large B-cell lymphoma (2019) |
FDA approved |
||||||
|
CD22 |
Inotuzumab ozogamicin (BESPONSA) |
Acute lymphoblastic leukemia (2017) |
FDA approved |
||||||
|
Moxetumomab pasudotox (Lumoxiti) |
FDA approved | ||||||||
|
Isatuximab (Sarclisa) |
Multiple Myeloma (2020) |
FDA approved |
|||||||
FDA approved |
[57][ |
GD2 |
Dinutuximab (Qarziba; Unituxin) | ||||||
|
PARP |
Olaparib (Lynparza) |
Advanced BRCA-mutated ovarian cancer (2020) |
FDA approved |
||||||
|
Rucaparib camsylate (Rubraca) |
BRCA-positive ovarian cancer (2016) |
FDA approved |
|||||||
|
Niraparib tosylate (Zejula) |
Epithelial ovarian, fallopian tube, or primary peritoneal cancer (2017) |
FDA approved |
|||||||
|
PDGFRα |
Avapritinib (Ayvakit) |
metastatic gastrointestinal stromal tumor (GIST) with platelet-derived growth factor receptor alpha (PDGFRA) exon 18 mutations (2020) |
FDA approved |
||||||
|
Multitarget TKI (VEGFRs, PDGFRα/β, CSF1R, KIT, and FLT3) |
Sunitinib malate (Sutent) |
Imatinib-resistant GIST and advanced RCC (2013) |
FDA approved |
||||||
|
Multitarget TKI (RET, VEGFRs, KIT, PDGFRα/β, FGFR1/2, RAF1, BRAF, and BRAFV600E) |
Regorafenib (Stivarga) |
Metastatic colorectal cancer (2012) |
FDA approved |
||||||
|
Multitarget TKI (VEGFR2/3, PDGFRβ, FLT3, KIT, RAF1, and BRAF) |
Sorafenib toylate (Nexavar) |
Advanced RCC (2005) |
FDA approved |
||||||
|
Multitarget TKI (VEGFRs, PDGFRα/β, FGFR1/2, KIT) |
Pazopanib HCl (Votrient) |
Metastatic RCC (2009) |
FDA approved |
FDA approved |
|||||
|
Temsirolimus (Torisel) |
Advanced RCC (2007) |
FDA approved |
Colorectal Cancer (2006) |
FDA approved |
|||||
|
PDGFRα |
Olaratumab (Lartruvo) |
Soft-tissue sarcoma (2016) |
FDA approved |
||||||
|
HER2 |
Pertuzumab (Perjeta) Hairy-cell leukemia (2018) |
FDA approved |
|||||||
|
Multitarget TKI (VEGFRs, FGFRs, PDGFRα, RET, and KIT) |
Lenvatinib mesylate (Lenvima) |
Thyroid cancer (2015) |
HER2-positive Breast cancer (2012) |
FDA approved |
|||||
|
Trastuzumab (Herceptin) |
HER2-positive Breast cancer (1998) |
FDA approved |
|||||||
|
Ado-trastuzumab emtansine (Kadcyla) |
HER2-Breast cancer (2013) |
FDA approved |
|||||||
|
CD19 |
Inebilizumab (Uplizna) |
Neuromyelitis optica and neuromyelitis optica spectrum disorders (2022) |
FDA approved |
||||||
|
CD19, CD3 |
Blinatumomab (Blincyto) |
Acute lymphoblastic leukemia (2014) |
FDA approved |
||||||
|
TROP2 |
Sacituzumab govitecan (Trodelvy) |
TNBC (2020) |
FDA approved |
||||||
|
CD3 |
Muromonab-CD3 (Orthoclone Okt3) |
Reversal of kidney transplant rejection (1986) |
FDA approved |
||||||
FDA approved | [ |
CD3, BCMA |
Teclistamab (TECVAYLI) |
Multiple myeloma (2022) |
FDA approved |
||||
|
gp100, CD3 |
Tebentafusp (KIMMTRAK) |
Metastatic uveal melanoma (2022) |
FDA approved |
||||||
|
CD30, CD3 |
Mosunetuzumab (Lunsumio) |
Follicular lymphoma (2022) |
FDA Review |
||||||
|
CD38 |
Daratumumab (Darzalex) |
Multiple Myeloma (2015) |
Neuroblastoma (2015) |
FDA approved |
|||||
|
Nectin-4 |
Enfortumab Vedotin (Padcev) |
Bladder cancer (2019), Urothelial cancer (2022) |
FDA approved |
||||||
