Submucosal endoscopy (third-space endoscopy) can be defined as an endoscopic procedure performed in the submucosal space. This procedure is novel and has been utilized for delivery to the submucosal space in a variety of gastrointestinal diseases, such as a tumor, achalasia, gastroparesis, and subepithelial tumors. The main submucosal endoscopy includes peroral endoscopic myotomy, gastric peroral endoscopic myotomy, Zenker peroral endoscopic myotomy, submucosal tunneling for endoscopic resection, and endoscopic submucosal tunnel dissection. Submucosal endoscopy has been used as a viable alternative to surgical techniques because it is minimally invasive in the treatment and diagnosis of gastrointestinal diseases and disorders.
- submucosal endoscopy
- third space endoscopy
- peroral endoscopic myotomy (POEM)
- endoscopic submucosal dissection (ESD)
1. Introduction
2. Peroral Endoscopic Myotomy
Inoue Tet al. performed the current afirst clinical POEM for the treatment of achalasia [5]. The endoscoppic management of achalications and evidence regarding submucosal endoscopy while exploring the possible future clinical applicaasia and non-achalasia spastic esophageal motility disorders has advanced with the introduction of POEM. This is because POEM has a theoretical superiority in that it does not injure the body surface, and the direction and length of the muscle layer incision can be set arbitrarily. Therefore, POEM has become the standard radical treatment for esophageal achalasia and related disorders as it is less invasive and has a higher curative effect than conventional therapeutic methods, such as laparoscopic Heller myotomy (LHM) [6,7]. For thions in this field.2. Expert Opinion
2.1. Efficacy of POEM
Several large case series and the diagnosis and tremeta-analyses have demonstrated the high clinical efficacy of POEM in achalasia with short-term and medium-term results (Table 1). A large multment of diseases that, to date, havicenter retrospective study of >1300 patients conducted in Japan reported that the efficacy of POEM was approximately 95% within 6 months to 1 year after POEM [15]. Another an unknown regionlarge study conducted in India demonstrated a 90.9% clinical success rate in 1 year [16]. POEM is an established ioreover, a large international multicenter study of 205 patients reported symptom relief rates of 98%, 98%, and 91% at 6 months, 1 year, and 2 years, respectively [17]. A prospective multicenter study conducted itian Japan also reported a high efficacy rate of 97.4% [18]. Thus, POEM could tbe a curative treatment modality forfor most patients with achalasia using the submucosal space. The emergence of the concept, with durable results of up to at least 1 year after the procedure. Although there are limited studies about the long-term outcomes of POEM, especially comparing the long-term outcomes of POEM in the submucosal space has dramatically evolved not onlywith those of conventional treatment methods, Teitelbaum et al. reported that POEM for the treatment but also the diagnosis of diseasesof achalasia resulted in durable long-term successful palliation of symptoms among 83% of patients after 5 years without the need for reintervention [19]. According Sto the literatubsequently, POET/STER has been developre comparing POEM with conventional therapeutic methods, such as LHM and pneumatic dilation (PD), POEM was more effective than LHM and PD, and numerous studies have demonstrated excellent patient outcomes [20,21,22,23,24,25]. In a randomized fclinical trial that cor the excision of subepithelial tumors fmpared POEM with PD as the initial treatment for patients with achalasia, POEM resulted in a significantly higher treatment success rate at 2 years [26]. Furthermom the esophagus and stomach. The other indicre, the 5-year follow-up of this randomized controlled trial also shows that POEM has a higher long-term efficacy and a lower risk of major treatment-related complications fthan PD [27]. A compr submucosal endoscopy include refractory gastroparesis and ZD. G-POEM/POP and D-POEM/Z-POEM have been developed for ehensive review suggested that POEM is equivalent to LHM for achalasia regarding cost efficiency, hospital length of stay, and the relief of dysphagia, with comparable side effects. According to a systematic review and meta-analysis that recently compared outcomes of POEM, LHM, and PD by evaluating 19 studies, including five randomized trials and 4407 patients with refractory gastr, the dysphagia reduction rates and postoperative Eckhardt scores were significantly superior for POEM compared with LHM and PD [28]. POEM could paresisotentially replace LHM as the standard therapy for achalasia. Moreover, ESTD/PCM was deriPOEM is applied as a treatment option not only among adults but also among pediatric patients with achalasia [29,30]. In a systematic revied from ESDw and meta-analysis about POEM for the managetreatment of early gastrointestinal cancer. Recentlypediatric achalasia, there was a significant reduction in the Eckardt score and lower esophageal sphincter pressure in POEM, and 93% of the patients experienced both short- and long-term improvement or the resolution of the achalasia symptoms after POEM [31]. On the other hand, the factorsubmucosal tunneling that accounted for technical difficulties in POEM were less experience with the technique has b, sigmoid-type esophagus, and short tunnels (<3 cm).| Study | Patients (N) | Median Follow-Up (year) | Previous Treatment (%) | Efficacy (%) | Adverse Events (%) | Reflux (%) |
|---|---|---|---|---|---|---|
| Shiwaku et al., 2020 [15] | 1346 | 1 | 31 | 95.1 (3 m) 94.7 (1 y) | 3.7 | 14.8 |
| Shiwaku et al., 2019 [18] | 233 | 1 | 21.9 | 97.1 (3 m) 97.4 (1 y) | 10.3 | 54.2 |
| Li et al., 2018 [32] | 564 | 4.1 | 34.2 | 94.2 (1 y) 92.2 (2y) 91.1 (3 y) 88.6 (4 y) 87.1 (5 y) | 6.4 | 37.3 |
| Nabi et al., 2018 [33] | 502 | 1.8 | 48.2 | 90.9 (1 y) 86.0 (2 y) 81.2 (3 y) | 1.6 | 21.5 |
| Zhang et al., 2018 [34] | 318 | 2.3 | 40.1 | 95.7 | 2.5 | 35.8 |
| Kumbhari et al., 2017 [11] | 282 | 1 | 28.6 | 94.3 | − | 23.2 |
| Nabi et al., 2017 [16] | 423 | 1.7 | 46 | 94 (1 y) 91 (2 y) 90 (3 y) | 4.5 | 28.3 |
| Ramchandani et al., 2016 [35] | 220 | 1 | 41.3 | 94 (6 m) 92 (1 y) | 6.4 | 21.6 |
| Inoue et al., 2015 [8] | 500 | 3 | 39 | 91 (1 y) 88.5 (3 y) | 3.2 | 16.8 |
2.2. Adverse Events of POEM
Adverse even applied not only in treatment but also in diagnosis. Subts associated with POEM include mucosal injury, pleural effusion, pneumomediastinum, emphysema, pneumothorax, pneumonia, and bleeding. Shiwaku et al. reported that adverse events occurred in approximately 4% of the 1346 patients who underwent POEM, half of whom had mucosal tunneling biopsy has recentinjuries, including five cases of perforation, but no patients suffered adverse effects requiring surgical treatment [18]. The most common delay emergeded adverse event is gastroesophageal reflux disease (GERD) [6,11,18,19,26,27,31]. All submucosal endoscopic procedures use a similar technique to the submucosal tunneconcern regarding POEM is that it may result in high rates of iatrogenic GERD. LHM and POEM cause postoperative GERD due to an impairment of the natural antireflux mechanisms. Therefore, LHM requires fundoplication to prevent GERD. However, in the case of POEM, a fundoplication is not performed. Recent studies have focused on GERD after POEM in greater detail and have reported an alarming incidence rate of 40–60% for GERD after POEM [6,11,18,19,26,28,36]. In a multing techniquecenter collaborative retrospective study, within 6 months after POEM, 63% of patients had erosive esophagitis [15]. Two reasons are considered for the submucosal tunneling technique is yet to be established and validated, and therefore,risk of GERD after POEM. First, the prolonged myotomy of the gastric wall. Second, the dissection of the collar sling muscle, which suspends the angle of His. In order to prevent GERD after POEM, the double-scope method was developed recently. The double-scope method can prevent the prolongation of the myotomy toward the gastric wall by observing the tip of the endoscope regarding the submucosal endoscopic player using the pediatric scope in the stomach [37,38,39]. Moreocedures are likely to become popular in the near futuver, a consensus meeting was held to discuss the management and prevention of GERD after POEM and how to deal with GERD refractory to acid-suppressing medications based on published papers and the personal experiences of each expert [39]. According to the. Although submucosal e results of this consensus meeting, it was confirmed that most patients with GERD after POEM respond to proton pump inhibitor therapy, and fundoplication for refractory GERD is rarely needed.3. Peroral Endoscopic Tumor Resection/Submucosal Tunnel Endoscopic Resection
Peroral endoscopyic tumor is largely saferesection (POET) and submucosal tunnel endoscopic resection (STER) are novel treatments involving endoscopic enucleation of subepithelial tumors of the upper gastrointestinal tract (Table 2) [40,41,42,43,44,45,46,47,48,49,50]. These were reported and previous studies seem to yield promising results regarding all subt the same time and are almost the same procedures, but POET is an improved therapeutic technique based on POEM, while STER is an improved therapeutic and ESD-inspired technique. The resection of subepithelial tumors using a variety of endoscopic techniques, such as endoscopic mucosal endresection and endoscopic proceduressubmucosal resection (ESD), has been described previously [51,52]. sHome issues newever, these endoscopic techniques are limited to be resolved to facilitate these procedures. Regarding efficacy, evidence is lacking and limited for the majority of these procedures. It subepithelial tumors arising from the muscularis mucosa or submucosal layer. Subepithelial tumors arising from the muscularis propria have basically been managed via surgical resection. Therefore, endoscopic resection, especially ESD for subepithelial tumors, has the risk of perforation, and it is difficult to close the defect. On the other hand, in POET and STER, the endoscopic resection of subepithelial tumors is possible that problems, such as adverse events, will surface with morwithout full-thickness perforation by the creation of a submucosal tunnel as a working space for tumor resection while maintaining mucosal integrity. Recently, endoscopic full-thickness resection (EFTR) has been reported as a feasible technique for subepithelial tumors arising from the muscularis propria [53,54]. Some stime and the accumulation of data, such as from GERD after POEMudies have reported the efficacy and safety of POET or STER for the treatment of subepithelial tumors. In a meta-analysis, high rates of en bloc resection were reported [55]. IAccordin particular, randomized studies and long-termg to a report with a large number of patients (290 patients with 4 years of follow-up data are yet to be accumulated, except those regarding POEM), POET or STER also showed no residual tumor, local tumor recurrence, or distant metastasis. A recent retrospective study compared the outcomes of STER, ESD, and thoracoscopic enucleation (TE) for esophageal subepithelial tumors. STER yielded the shortest duration of hospitalization and the lowest cost compared with other modalities [56]. SThere is a pressing need for additional meaningful data that can appropriately position theseER showed superiority to TE regarding procedure times and tumor location. Moreover, the resections for tumors with STER were larger than those for tumors with ESD. STER was more effective for the resection of large subepithelial tumors than ESD. A study comparing POET to TE demonstrated that the procedures. Therefore, as the time and duration of hospital stay for POET were significantly shorter than those for TE [57]. In a retrospe procedures become increasingly common, it is nctive study that compared EFTR to STER, although there was no significant difference in treatment outcome, EFTR yielded longer durations of hospital stay [58]. Thesec ressary to addresults indicated that the use of a submucosal tunnel decreases the issues of training, and further guidelines will be necessary. These procedures are not easy to learn asrisk of gastrointestinal tract leakage and infection. On the other hand, these studies should be interpreted with caution in extrapolating them to all subepithelial tumors, as most of the pathological diagnosis was leiomyoma. If the subepithelial tumor has malignant potential, such as GIST, en bloc resection with an intact capsule is necessary to avoid recurrence because GISTs have a fragile capsule compared to other subepithelial tumors, and there are differences between Asia and other regions, even in ESD skill levels. Submucosal endoscopy is a complex procedure based on surgical principles. Nevertheless, these procedures are performed by not ois a risk of seeding if the capsule ruptures. It is imperative that GISTs be resected with the capsule intact, which requires advanced POET or STER techniques and should only be performed by specialized operators at experienced facilities. The indications for POET and STER are as follows: (i) the best location of the tumor (esophagus and gastric cardia), (ii) growth type (intraluminal and intramural growth type), and (iii) tumor size (<40 mm or with symptoms). According to recent studies, POET and STER could safely achieve a high rate of en bloc resection for upper gastrointestinal subepithelial tumors smaller than 40 mm. However, there are some limitations to POET or STER. The main factors that make en bloc resection impossible are the large size and irregular shape of the tumor [57,59]. In particuly surgeons but also endoscopists. Thereforar, as there is a size limitation for tumors that can be retrieved perorally and as it is performed in a limited working space, tumors larger than 40 mm are generally not indicated for POET or STER.| Study | Patients (N) | Location | Size (Range) (mm) | En Bloc Resection Rate (%) | Adverse Events (%) | Recurrence (%) | Pathological Diagnosis |
|---|---|---|---|---|---|---|---|
| Du et al., 2019 [48] | 165 | Esophagus: 106 Cardia: 59 | 20.0 (5.0–80.0) | 77.6 | 21.2 | 0 | Leiomyoma: 157 GIST: 3 Other: 5 |
| Li et al., 2017 [47] | 74 | Esophagus: 74 | 18.9 | 98.6 | 9.5 | 2.7 | Leiomyoma: 67 GIST: 7 |
| Mao et al., 2017 [46] | 56 | Esophagus: 18 Stomach: 38 | 18 (10–32) | 100 | 15.3 | 0 | Leiomyoma: 45 GIST: 10 Other: 1 |
| Chen et al., 2016 [44] | 290 | Esophagus: 199 Esophagogastric junction: 68 Stomach: 23 | 21 (10–70) | 89.3 | 23.4 | − | Leiomyoma: 226 GIST: 53 Other: 11 |
| Wang et al., 2015 [43] | 80 (tumors: 83) | Esophagus: 67 Cardia: 16 | 23.2 (10–55) | 97.6 | 8.75 | 0 | Leiomyoma: 68 GIST: 15 |
| Ye et al., 2014 [42] | 85 | Esophagus: 60 Cardia: 16 Stomach: 9 | 19.2 (10–30) | 100 | 9.4 | 0 | Leiomyoma: 65 GIST: 19 Other: 1 |
| Onimaru et al., 2020 [50] | 47 | Esophagus: 31 Cardia: 16 | 25.7 | 91.9 | 4.7 | 0 | Leiomyoma: 34 GIST: 6 Other: 7 |
| Chiu et al., 2019 [49] | 51 | Esophagus: 11 Stomach: 39 Duodenum: 1 | 20.71 | 94.1 | 4 | 1.96 | Leiomyoma: 20 GIST: 15 Other: 16 |
4. Gastric Peroral Endoscopic Myotomy/Peroral Endoscopic Pyloromyotomy
3. Highlights
PO
5. Diverticular Peroral Endoscopic Myotomy/Zenker’s Peroral Endoscopic Myotomy
Esophageal diverticula are rare sac-like outpouchings, and the prevalence rate is approximately 3% [73,74]. Zenker’s diverticulum (ZD) is the most common type of esophageal diverticulum. M has become the standard radicost patients with esophageal diverticula are asymptomatic; however, they may experience dysphagia, regurgitation, and chest pain with disease progression. Treatment for esophageal diverticula should be considered for symptomatic cases, regardless of the size of the diverticulum. Although surgical treatment for with cricopharyngeal myotomy is basically applied to esophageal achalasiadiverticula, surgical treatment has high invasiveness and related disorders as it is less invasive and has a hisk of adverse events. Following advancements in endoscopic techniques, endoscopic treatment for esophageal diverticula has become a widely accepted alternative to surgery. Conventionally, endoscopic septotomy has been applied to the esophageal diverticula. A meta-analysis of studies demonstrated that endoscopic septotomy yielded a significantly shorter procedure time and duration of hospital stay and fewer adverse events compared with the surgical group [75]. On the other hand, the rates of symptom recurrence after endoscopic septotomy were much higher curative effect than conventional therapeutic methods such as LHM. POEthan those after surgery due to incomplete septotomy. Submucosal tunneling septotomy by diverticular peroral endoscopic myotomy (D-POEM) is a novel technique and has been recently established as an effective method for complete septal dissection using a submucosal tunneling approach. Moreover, this technique has been applied effectively among patients with Zenker’s diverticulum (Z-POEM) [76–78]. In a large international study, the overall technical success rate was 97.3%, adverse events (such as bleeding and perforation) occurred in 6.7%, and the rate of symptom recurrence was 3.2% [79]. Moreover, a recent systematic review comparing Z-POEM and PerOral endoscopic septotomy (POES) also showed no difference in terms of both efficacy and safety [80]. A recent multicenter retrospective study demonstrated the overall technical success rate of D-POEM to be 90.9% without adverse events, clinical success to be achieved at 100%, and good short-term outcomes [81]. D-POEM and Z-POEM appear to be safe and feasible treatments for patients with symptomatic esophageal diverticula.
6. Submucosal Tunneling Biopsy
T/he recent development of STER is a novel treatment modality involving endoscopic enucleation of suEMF [3] is applied not only for use in the treatment of tumors but also for tissue sampling for diagnostic purposes [84–86]. This technique can be applied to access the muscular layer and myenteric plexus of the gastrointestinal tract less invasively for pathological diagnosis in patients with gastrointestinal motility disorders and to obtain biopsies of the submucosal tumors of the gastrointestinal tract. Particularly, esophageal motility disorders have unknown etiologies with various possible underlying pathologies and are currently defined only by manometry patterns. There are some techniques for the tissue sampling of the muscular layer of the gastrointestinal tract, but they have some limitations [87,88]. Precise histological diagnosis requires adequate tissue samples. However, endoscopic full-thickness biopsy has a high delayed perforation rate and is limited by a lack of adequate sample size. For subepithelial tumors of the upper GI tract without full-thickness , endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) is a safe and effective method, and it is the current standard modality for sampling gastrointestinal subepithelial tumors [89,90]. Nevertheless, in a systematic review with a meta-analysis, the diagnostic accuracy rate (59.9%) was moderate, and failures of FNA occurred due to insufficient samples for histological analysis, technical issues, location, and lesions smaller than 2 cm [91]. When considering the limitations of the aforementioned techniques, the submucosal tunneling method is a safe and effective method to perforationm a biopsy with direct visual control over the region of interest.
7. Endoscopic Submucosal “Tunnel” Dissection/Pocket-Creation Method
Generally, one of the factors contributing to the technical difficulty of ESD is the lack of traction. Hence, several novel methods and strategies have been invented and developed to overcome technical difficulties. Endoscopic submucosal tunnel dissection (ESTD) [92,93] and the pocket-creation method (PCM) [94] are derived from ESD. These methods are new in the field of submucosal endoscopy, including POEM for achalasia and STER for submucosal tumors. These novel techniques are used to improve the ESD procedure without extra devices or equipment (Table 3). The creation of the tunnel in ESTD and PCM enables the tip of the endoscope to stabilize in the submucosal tunnel, providing sufficient traction even with severe submucosal fibrosis. Moreover, the advantage of creating a submucosal tunnel is the ability to maintain a clear view of the submucosal layer, in which efficient submucosal dissection becomes possible and contributes to shortening the procedure time. In ESTD, mucosal incisions are initially made at the anal and oral sides of the lesion after the submucosal injection, and then the submucosal dissection is performed between the anal and oral incisions to create a tunnel underneath the lesion. On the other hand, during PCM, a partial mucosal incision is first made on either the oral or anal side of the lesion in order to slip into the submucosal layer. Next, the middle aspect of the submucosal layer underneath the lesion is dissected to create a submucosal pocket. After creating the submucosal pocket, the mucosal incision is extended segmentally from the edges of the pocket. This method not only maintains a stable scope position inside the pocket with good traction but also prevents injection leakage. This approach also allows for tangential scope access even in situations in which the device often faces the muscle layer perpendicularly. ESTD is useful in the management of esophageal lesions due to a narrow lumen. Therefore, ESTD was developed as an alternative technique to esophageal ESD, particularly for circumferential superficial esophageal neoplastic lesions (Figure 1). The indications of ESTD for esophageal neoplastic lesions are lesions with a diameter of >20 mm and those involving at least one-third of the esophageal circumference. A recent meta-analysis revealed favorable short-term outcomes. The rates of en bloc resection, R0 resection, and curative resection were 98% (95% CI: 95.8–99.0%), 87.0% (95% CI: 78.2–92.5%), and 87.6% (95% CI: 67.4–96.0%), respectively [95]. In a propensity-matching analysis of conventional ESD for superficial esophageal squamous cell carcinoma, the ESTD group demonstrated a significantly shorter procedure time and submucosal dissection time than the conventional ESD group. In addition, ESTD reduced the rate of injury to the muscular layer [96]. On the other hand, PCM could be applied to other locations in the gastrointestinal tract, such as the colorectum. This is because the colorectal lumen is wide, and PCM can dissect not only the middle part of the submucosal layer underneath the lesion but also the lateral part, creating a pocket. PCM is advantageous in that it can decrease the leakage of the injection solution because the tunnel entry is made on either the oral or anal side. Therefore, PCM is useful for wide lesions such as laterally spreading tumors. A recent retrospective study revealed higher rates of en bloc resection and completed resection in the PCM group compared with the conventional ESD group. In addition, the dissection speed in the PCM group was faster than that in the conventional ESD group, while there was no significant difference in adverse events [99]. Among patients with severe fibrosis, PCM yielded a higher en bloc resection rate and a shorter mean procedure time than the conventional non-PCM method, and PCM reduced the discontinuation rate [100]. Recently, saline-pocket endoscopic submucosal dissection (SP-ESD) has been developed as a modification of PCM by filling the pocket with saline (saline immersion ESD), like underwater ESD. Water immersion facilitates the visualization of the dissection line because the endoscopic view in water immersion is clearer because of the refractive index of water. In a randomized controlled trial, the median dissection speed was significantly higher, and the median procedure time was significantly shorter in the SP-ESD group than in the conventional ESD group [101]. The insertion of a small-caliber-tip transparent (ST) hood under the mucosal flap is a crucial step in creating a submucosal tunnel. Therefore, we have developed a new technique, the “water pressure method” (Figure 2) [105]. Water pressure, induced by the water-jet function of the endoscope, facilitates the insertion of the ST hood under the mucosal flap. The “water pressure method” is simple and useful for ESD.
Table 3. Clinical G-outcomes compared between POEM/CM/ESTD and conventional ESD.
|
Study |
Method |
Patients Study/ESD (N) |
Location |
Specimen Size Study/ESD (mm) |
Specimen Area Study/ESD (mm2) |
Procedure Time (Study/ESD) (min) |
Dissection Speed Study/ESD (mm2/min) |
En bloc Resection Rate Study/ESD (%) |
Adverse Events Study/ESD (%) |
|
Zhang et al. 2019 [98] |
ESTD |
32/55 |
Stomach |
− |
1573.0/930.1 (p < 0.01) |
87.3/136.7 (p < 0.01) |
18.0/7.8 (p < 0.01) |
100/87.3 (p = 0.035) |
59.4/100 (p < 0.01) |
|
Zhang et al. 2018 [97] |
ESTD |
52/98 |
Esophagus |
15.37/12.95 |
− |
93.21/92.39 |
21.54/16.10 (p = 0.002) |
96.15/88.78 |
9.62/8.16 |
|
Huang et al. 2017 [96] |
ESTD |
38/38 |
Esophagus |
39.0/36.0 |
− |
38.0/48.0 (p = 0.006) |
23/17 (p < 0.001) |
100/100 |
0/7.9 |
|
Harada et al. 2019 [101] |
PCM |
46/45 |
Colorectum |
32.5/34.0 |
− |
29.5/41.0 (p < 0.001) |
20.1/16.3 (p < 0.001) |
100/100 |
8.7/8.9 |
|
Takezawa et al. 2019 [99] |
PCM |
280/263 |
Colorectum |
35.3/35.7 |
− |
69.5/78.7 |
23.5/20.9 (p < 0.001) |
100/96 (p < 0.001) |
3.9/4.9 |
|
Harada et al. 2018 [102] |
PCM |
48/48 |
Stomach |
− |
34.0/32.5 |
27.5/41.0 (p < 0.001) |
22.5/17.3 (p < 0.001) |
100/100 |
8.3/6.3 |
|
Sakamoto et al. 2017 [103] |
PCM |
73/53 |
Colorectum |
27/25 |
− |
− |
19/14 (p = 0.03) |
100/92 (p = 0.03) |
1.4/4.1 |
|
Kanamori et al. 2017 [104] |
PCM |
47/49 |
Colorectum |
26/30 |
− |
77/85 |
14.3/11.8 |
100/88 (p = 0.015) |
10.6/24.5 (p = 0.018) |
POPCM, pocket-creation method; ESTD, is technicalendoscopic submucosal tunnel dissection; ESD, endoscopic submucosal dissection.
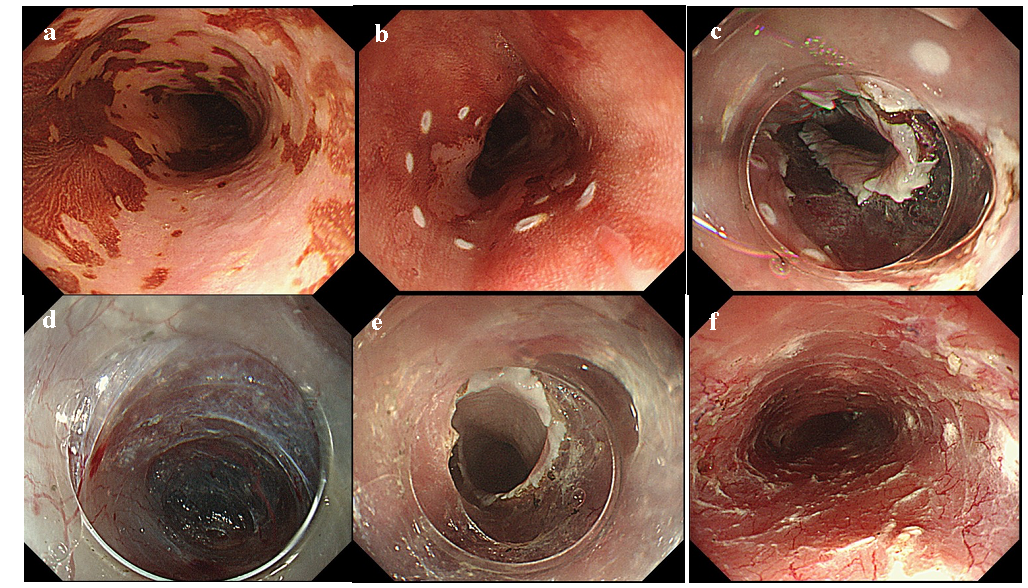
Figure 1. Endoscopic submucosal tunnel dissection for a circumferential superficial esophageal neoplastic lesion. (a) Chromoendoscopic image with iodine staining. (b) Circumferential markings were performed. (c) A complete circumferential mucosal incision was made to the distal side of the lesion to make an endpoint. (d) A submucosal tunnel was created. (e) The submucosal tunnel was created from an oral-to-anal incision through submucosal dissection. (f) The artificial ulcer after en bloc resection of the lesion.
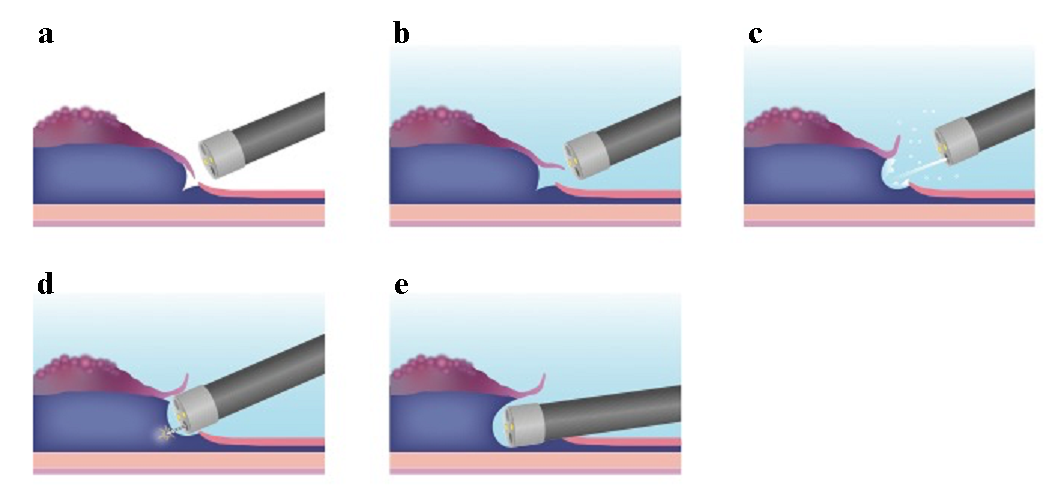
Figure 2. Methodolyogic schema feasof the water pressure method. (a) Partibal mucosale incision is performed. (b) In an underwater situation pat, the opening of the mucosal flap is easier due to buoyancy. (c) Water pressure using thents with g water-jet function of the endoscope helps with the insertion of the endoscope under the mucosal flap. (d) Approach of the endostrocope to the submucosal layer becomes easy. (e) As a result, the water pressure method caresis usn be used to insert the endoscope quickly and easily into the submucosal layer.
8. Solutions for Submucosal Injection
A solutiong myotomy. D-POEM/Z-POEM has been established recently as an effective method for submucosal injection is essential to have good visualization and access to the submucosal space, not only for ESD but also for submucosal endoscopy. The ideal injection solution should be inexpensive, readily available, nontoxic, as well as safe, and efficient with a long-lasting submucosal cushion. Currently, various types of submucosal injection solutions have been developed in different countries. The representative solution is normal saline (NS). NS has been the most widely used because it is inexpensive, readily available, and nontoxic. However, the major limitation of NS is its rapid absorption into the surrounding tissues, which shortens the duration of an adequate submucosal cushion. Glycerol (Glyceol, Chugai Pharmaceutical Co, Tokyo, Japan), which is a hypertonic solution consisting of 10% glycerin and 5% fructose in an NS, is widely used as a submucosal injection solution in Japan. Because glycerol is hypertonic, it can take a longer submucosal elevation than NS. Moreover, glycerol causes no tissue damage, is inexpensive, and is readily available in Japan. Several studies have reported the usefulness of sodium hyaluronate (SH) as the longest-lasting submucosal elevation. Therefore, it is commonly used as one of the standard submucosal injection solutions in ESD. However, the main disadvantages of SH are its high cost and unavailability in Western countries. Eleview® is a synthetic solution, including water for complete septalinjection, medium-chain triglycerides, poloxamer 188, polyoxyl-15-hydroxystearate, sodium chloride, and methylene blue. Some studies have reported that Eleview® is . Moreover, Eleview® is a readiy-to-use injectable liquid ampule. On the other hand, Eleview® has high cosection using a sts as an SH. We would normally use NS or Glyceol, and in difficult fibrotic situations, we would prefer to use SH. In any case, we should take into account the lesion features and the availability and costs of the solution, as well as the balance between its advantages and potential adverse effects.
9. Conclusions
Submucosal tuenneling approachdoscopy derived from ESD is a novel operating field in which several new endoscopic procedures have emerged. Submucosal tunneling biopsy is a safe and eendoscopy has evolved over approximately a decade since the first report on POEM in 2010 and has been expanding into the field of the entire gastrointestinal tract. However, its efficacy, as assessed via long-term follow-up, remains unclear. Thus, further prospective large-scale studies with long-term follow-up are warranted to confirm the efficacy of submucosal endoscopy. In the near future, submucosal endoscopy holds the promise of a breakthrough in the diagnosis and treatment of gastrointestinal diseases and disorders.
10. Expert Opinion
Submucosal endoscopy has emerged as a novel operating field fective method with a direct visual control of the region of interest. or interventional endoscopy, and its use has significantly increased over the past decade. The main reason is that submucosal endoscopy adopts the concept of SEMF. SEMF has enabled endoscopists to safely utilize the submucosal space. SEMF has become a breakthrough in the diagnosis and treatment of diseases that, to date, have an unknown region. POEM is an established initial treatment modality for achalasia using the submucosal space. The emergence of the concept of POEM in the submucosal space has dramatically evolved not only the treatment but also the diagnosis of diseases. Subsequently, POET/STER has been developed for the excision of subepithelial tumors from the esophagus and stomach. The other indications for submucosal endoscopy include refractory gastroparesis and ZD. G-POEM/POP and D-POEM/Z-POEM have been developed for patients with refractory gastroparesis. Moreover, ESTD/PCM is a novel approach to safer and easier resection of cancer even with severe submucosal fibrosis. In the near future, swas derived from ESD for the management of early gastrointestinal cancer. Recently, the submucosal tunneling technique has been applied not only in treatment but also in diagnosis. Submucosal tunneling biopsy has recently emerged. All submucosal endoscopic procedures use a similar technique to the submucosal tunneling technique. The submucosal tunneling technique is yet to be established and validated, and therefore, submucosal endoscopic procedures are likely to become popular in the near future. Although submucosal endoscopy is largely safe, and previous studies seem to yield promising results regarding all submucosal endoscopic procedures, some issues need to be resolved to facilitate these procedures. Regarding efficacy, evidence is lacking and limited for the majority of these procedures. It is possible that problems, such as adverse events, will surface with more time and the accumulation of data, such as from GERD after POEM. In particular, randomized studies and long-term follow-up data are yet to be accumulated, except those regarding POEM. There is a pressing need for additional meaningful data that can appropriately position these procedures. Therefore, as these procedures become increasingly common, it is necessary to address the issues of training, and further guidelines will be necessary. These procedures are not easy to learn as there are differences between Asia and other regions, even in ESD skill levels. Submucosal endoscopy holds promise of breakthrough in the diagnosis and treatment of gastrointestinal diseases and disordersis a complex procedure based on surgical principles. Nevertheless, these procedures are performed by not only surgeons but also endoscopists. Therefore, it is necessary to construct optimum training systems such as animal models and observerships at expert centers. In particular, endoscopists have to perform the procedure in close contact with surgeons when treating patients. After all, submucosal endoscopy is a less invasive procedure than surgery but is still somewhat invasive to the patient. Hence, the indications for these procedures must be decided strictly, and it is necessary to create guidelines. In the future, the concept of “inside and outside of the gastrointestinal tract” will lose practicality in endoscopic treatment, and it will become possible to diagnose and treat gastrointestinal diseases and disorders with an optimum approach and with minimal invasion while freely moving in the lumen and peritoneal cavity. Thus, it may be useful for investigating diseases for which the cause is unknown. In addition, improved devices and techniques may reduce procedure-related complexities and allow the endoscopist to perform these procedures more easily. As our understanding of these procedures improves, the future of submucosal endoscopy could hold promise in diagnostic as well as therapeutic endoscopy.
