2. Association of Oxidative Stress and Inflammation on Asthma
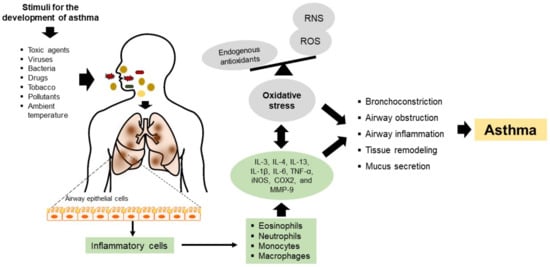
The pathogenesis of asthma involves chronic airway inflammation triggered by allergen agents, ambient temperature, tobacco, bacteria, viruses, respiratory infections, or mechanical stimuli such as exercise. Cells mediating the inflammatory response, such as eosinophils, neutrophils, monocytes, and macrophages, generate ROS and reactive nitrogen species (RNS), contributing to oxidative stress and aggravating the detrimental effects of airway inflammation (
Figure 1). On the other hand, oxidative stress in asthma may also be attributed to viral or bacterial infections and is even considered a factor that can exacerbate this pathology
[7][9]. Such a situation was demonstrated in patients with asthma, where a considerable percentage of viral and bacterial co-infections were observed, and the predominant viruses were rhinoviruses, respiratory syncytial virus, influenza virus, and metapneumovirus. At the same time, the major species of bacteria present were
Streptococcus pneumoniae and
Haemophilus influenzae. In both cases, the patients had lower exhaled nitric oxide (NO) levels, lower immunoglobulin E (IgE) titers, and a higher incidence of comorbid sinusitis, COPD, or pneumonia
[8][10]. These findings have also been related to an increased risk of hospital readmission. This phenomenon is possible because these allergens regulate the toll-like receptor (TLR) and intracellular adhesion molecule-1 (ICAM-1) pathways, causing an increase in neutrophil degranulation and cell lysis, thus exacerbating the clinical severity of the pathology
[9][11].
Airway inflammation is an essential feature of this pathology where the nuclear factor kappa-light-chain-enhancer of activated B (NF-κB) regulates several genes involved in the immune and inflammatory responses. Here, NF-κB is translocated to the nucleus due to the degradation of inhibitory kappa B (IκB), where NF-κB binds to the promoter region of proinflammatory mediators, including inducible nitric oxide synthase (iNOS), cyclooxygenase 2 (COX2) and matrix metallopeptidase-9 (MMP-9)
[10][12]. Thus, the over-expression of iNOS and COX2 increases NO synthesis, which aggravates the inflammatory response. Chronic inflammation and oxidative stress results in cell proliferation, apoptosis of respiratory epithelium, bronchoconstriction, an increase in mucus secretion and airway remodeling, and, finally, irreversible airflow limitations (
Figure 1)
[11][13].
In allergic asthma, exposure to allergens causes an imbalance between the T helper type 1 (Th1) and Th2 cells. The activation of Th2 cells is related to the inflammatory response, leading to tracheal hypersensitivity owing to cytokine release, including interleukin 13 (IL-13), IL-5, and IL-4
[12][14].
3. Garlic
Nowadays, it is indisputable that dietary interventions play a key role in the survival and maintenance of health, as well as in managing diseases, including cardiovascular disease, diabetes mellitus, metabolic syndrome, and cancer
[13][15]. Several studies have reported that nutraceuticals (foods or parts of them) have antioxidant and anti-inflammatory properties that can protect, prevent, or improve chronic diseases such as the lung, including asthma
[14][16]. Garlic is a nutraceutical with health benefits due mainly to the organic sulfur compounds derived from cysteine contained in it
[15][17]. Intact garlic contains non-volatile (non-odiferous and stable) γ-glutamyl-S-alk(en)yl-l-cysteines, namely, γ-glutamyl-S-allyl-l-cysteine, γ-glutamyl-S-trans-1-propenyl-l-cysteine, and S-alk(en)yl-l-cysteine sulfoxides such as S-allyl-l-cysteine sulfoxide (alliin), S-(trans-1-propenyl)-l-cysteine sulfoxide (isoalliin), and S-methyl-l-cysteine sulfoxide (methiin) with a small amount of S-allyl cysteine (SAC). When garlic cloves are crushed or chopped, the enzyme alliinase stored in the vacuoles is released, which encounters cytosolic alliin to convert it into a series of thiosulfinates, most notably allicin (diallyl thiosulfinate). The highly reactive, unstable, and volatile allicin breaks down to produce a large number of sulfides, which are oil-soluble compounds responsible for garlic’s characteristic odor and taste. These sulfides correspond to diallyl sulfide (DAS), diallyl disulfide (DADS), diallyl trisulfide (DATS), methyl allyl disulfide (MADS), methyl allyl sulfide (MAS), ajoene, and vinyl dithiins (2-vinyl-1,3-dithiin, 3-vinyl-1,2-dithiin). The water-soluble garlic compounds are SAC, S-allylmercapto-l-cysteine (SAMC), and S-methyl cysteine
[16][8].
4. Effect of Garlic Compounds on Asthma
A study investigated the effects of intraperitoneal injection of aged garlic extract (AGE) on established allergic airway inflammation in a murine model (BALB/c mice)
[17][18]. The injection of AGE caused a decrease in the allergic airway inflammation, including eosinophil percentage in bronchoalveolar lavage fluid (BALF), immunoglobulin G
1 (IgG
1) levels in BALF and serum, the proportion of mucous-producing goblet cells, and peribronchial and perivascular inflammation. It also increased BALF’s interferon-gamma (IFN-γ) levels. The results suggested that AGE could attenuate inflammatory features of allergic airway inflammation.
Shin et al. investigated the effects of DADS on airway inflammation using a mouse model of ovalbumin-induced asthma
[18][19]. In this study, DADS suppressed the expression of iNOS, COX2, and MMP-9, which decreased NF-κB activation, thus inhibiting the production of inflammatory markers (IL-1β and IL-6) in experiments in vitro and in vivo. The suppressed expression of MMP-9 by DADS treatment caused a reduction in IL-4, IL-5, IL-13, and IgE in the lung tissue of rats with asthma. In addition, ovalbumin-induced asthma decreased the expression of IFN-γ levels, while DADS treatment significantly increased the expression of IFN-γ and the expression of antioxidant proteins, such as nuclear factor (erythroid-derived 2)-like 2 (Nrf2) and hemeoxygenase-1 (HO-1) in experiments in vivo and in vitro, leading to reduced ROS production
[18][19]. Thus, the results showed that DADS decreases the inflammatory response by enhancing the antioxidant status induced by Nrf2 activation.
Other studies investigated the effects of DAS orally administered on ovalbumin-induced pulmonary inflammation of asthma mice
[19][20]. In this study, DAS decreased airway inflammation, mucus secretion, and oxidative damage in the lung of asthma mice. In asthmatic responses, Nrf2 disruption causes an increase in the levels of Th2 cytokines IL-4 and IL-13. DAS administration elevated the Nrf2 translocation from the cytosol to the nucleus in the lung cells and consequently decreased the inflammatory state. Specifically, DAS reduced the number of eosinophils in BALF, preventing inflammatory cell infiltration and the generation of Th2 cytokines (IL-4 and IL-10) via Nrf2. Furthermore, DAS decreased the expression of 8-Hydroxy-2’-deoxyguanosine (8-OHdG) and 8-isoprostane, two biomarkers of oxidative damage, suggesting that DAS reduced ROS generation and prevented oxidant-induced damage in the lung
[19][20]. In addition, DAS treatment downregulated the expression of microRNAs (miRNAs) such as miR-144, miR-34a, and miR-34b/c, which play a role in oxidant and inflammatory activities
[20][21][21,22].
Inhalant allergens such as dust or house mites are considered the most important source of allergens worldwide. Dust mites, particularly
Dermatophagoides pteronyssinus (Der p), constitute one of the most critical risk factors for allergic respiratory diseases in patients with a genetic predisposition. In this context, the oral administration of the water-soluble fraction of garlic (collected in Taichung City, Taiwan) on Der p-induced allergic airway inflammation in mice was evaluated
[22][23]. The total inflammatory cells determined in the lung of asthmatic mice were increased by Der p; however, garlic treatment inhibited the total cell counts and inflammatory cell infiltration (eosinophils and lymphocytes) around perivascular space. These results are supported by the reduction of Th2 cytokines by garlic treatment, an important cytokine that regulates the secretion of IgE. In contrast, the garlic extract fraction was found to increase IFN-γ levels. These results indicate that garlic reduces airway inflammation by decreasing Th2 cytokines and increasing Th1 cytokines. In addition, IgE is related to the NF-κB activation
[23][24]. The reduction of IgE by the garlic fraction treatment also inhibited the phosphorylation of NF-κB and the decrement in the expression of IL-13 and IL-4. Garlic extract administration modulated the anti-inflammatory response by inhibiting the IL-6/PI3K/Akt/NF-κB pathway.
Hsieh et al. also reported that garlic extract (collected in Taichung City, Taiwan) corrected the imbalance of Th1 and Th2 cells in BALB/c mice with Der p-induced asthma. Again, Th2 cytokines (IL-4, IL-5, and IL-13) decreased with garlic administration, causing a reduction in the stimulation of mucus secretion from epithelial cells in the airways, decreasing the expression of vascular endothelial cell adhesion molecules (VCAM) and inhibiting IgE production. On the other hand, it increased IFN-γ and IL-12 and restored the expression of IL-10 in BALF
[22][23]. SAC is another compound in garlic that has been reported to have beneficial effects on the ovalbumin-induced asthma model
[15][17]. In this study, SAC attenuated airway hyperresponsiveness and inflammatory cell infiltration by significantly reducing inflammatory cell counts. In asthma, goblet cells show an increase in mucin 5AC (MUC5AC), a major component of airway mucus, caused by an increase in Th2 cytokines. Mucus production from goblet cells is triggered by an increase in Th2 cytokines and increased activity of molecules in the inflammatory signaling pathway, such as NF-κB
[24][25]. In addition, the oral administration of SAC decreased Th2 cytokines and IgE levels in BALF and serum. Finally, SAC administration inhibited NF-κB translocation to the nucleus and, thus, the transcription of inflammatory proteins, resulting in reduced airway hyperresponsiveness and MUC5AC.
Other studies have reported that oral administration of SAC has beneficial effects in neonatal asthmatic rats (in an ovalbumin-induced asthmatic animal model)
[25][26]. SAC administration decreased the inflammation and the infiltration of eosinophils, lymphocytes, mast cells, and monocytes, as well as the number of goblet cells in the airway. In addition, SAC decreased smooth muscle mass, mucous gland hypertrophy, and vascular congestion in the asthmatic model. In this study, the administration of SAC decreased the expression of fibrinogen, prothrombin, and thrombin time; these parameters are related to the degree of inflammation in asthma. Moreover, SAC administration decreased the expression of TNF-α, IL-1β, IL-6, IL-13, and IL-17. In contrast, the expression levels of IL-10 were increased with the treatment
[25][26]. Studies have reported that the production of several proinflammatory cytokines is inhibited in the presence of prostaglandin E2 (PGE2). PGE2 suppresses the production of the Th1 cytokine secretion
[26][27]. However, PGE2 can act on uncommitted B lymphocytes to promote isotype switching to IgE or IgG1
[27][28]. IL-6 is a proinflammatory mediator involved in synthesizing PGE2 and the infiltration of eosinophils in the airway. In asthmatic animals, high expression of COX2 correlates with IL-6, which regulates immune cells to generate PGE2. SAC treatment decreased IL-6, PGE2, and COX2. In addition, other compounds derived from arachidonic acid, such as leukotriene, cysteinyl leukotrienes, and leukotrienes B4 in eosinophils, act as potent bronchoconstrictor and cause airway smooth muscle constriction and increase mucus secretion. These effects were decreased by SAC treatment
[25][26]. IL-13 also plays a role in this pathology by regulating the inflammation and remodeling of the lung tissues by Th2 cytokines. This mechanism is accompanied by a coordinated response of the various chemokines, such as eotaxin, which, upon activation, regulated normal T cell expressed and secreted macrophage inflammatory protein-1 beta (MIP1-β) and monocyte chemoattractant protein-1 (MCP-1), resulting in the Th2 inflammatory response in the lungs. This phenomenon increases the traffic of eosinophils from the bloodstream to the airways, increasing adhesion molecules to join the epithelial cells of the airways. In this study, IL-13 inhibition through SAC administration could ameliorate asthma-related inflammatory events by downregulating Th2 cytokines. Therefore, SAC may be an important nutraceutical for inhibiting airway inflammation by decreasing the expression of inflammatory cytokines in asthma patients. The garlic compounds could also be used as a coadjutant or therapeutic option in treating pathogen-infected asthma exacerbation patients, mainly bacterial and viral infections. Based on this knowledge, the dietary intake of these nutraceuticals as coadjuvant therapy could reduce the adverse effects of antiviral drugs, including preventing bacterial or viral infections that exacerbate asthma.