Microneedles are micron-sized devices that are used for the transdermal administration of a wide range of active pharmaceutics substances with minimally invasive pain. 3D-printing technologies that have the potential to revolutionize the manufacturing of microneedles. 3D-printed microneedles have applications in various fields, such as drug delivery, vaccine delivery, cosmetics, therapy, tissue engineering, and diagnostic devices. Microneedles are classified into five types, which include solid microneedles, hollow microneedles, coated microneedles, hydrogel-forming microneedles, and dissolving microneedles. This review enumerates the challenges that are posed by the 3D-printing technologies, including the manufacturing cost, which limits its viability for large-scale production, the compatibility of the microneedle-based materials with human cells, and concerns around the efficient administration of large dosages of loaded microneedles.
- drug delivery
- FDA regulations
- microneedles
- artificial intelligence
- 3D printing
1. Introduction
-
A computerized 3D solid model is developed;
-
It is converted into a standard AM file format, such as the standard tessellation language format (STL) [13];
- It is converted into a standard AM file format, such as the standard tessellation language format (STL) [13]
- The STL file is sent to a 3D printer where it is modified, e.g., changing the position and orientation of the part or scaling the part;
- ;
- The part is built layer-by-layer on the 3D-printing machine;
-
The cleaning, finishing, and post-processing of the printed parts are conducted.
- A computerized 3D solid model is developed;
- The STL file is sent to a 3D printer where it is modified, e.g., changing the position and orientation of the part or scaling the part;
- The part is built layer-by-layer on the 3D-printing machine;
- The cleaning, finishing, and post-processing of the printed parts are conducted.
| Advantages | Disadvantages |
|---|---|
| Designs can be easily changed, and a range of simple to complex structures can be manufactured. | High-resolution printers are expensive and require huge start-up capital. |
| Printing parts can be easily optimized—lightweight and heavy objects can be fabricated. | Build speeds can be slow and high-volume production is limited. |
| Compared to machining, less wastage is generated. | Additional costs might be incurred for the post-processing of finished products for high-quality surface finish. |
| Parts can be manufactured end-to-end without the need for specialized tools. | 3D printers are materials-specific, and this can limit versatility. |
| Complex geometrical structures can be fabricated without any restrictions. |
2. Microneedles
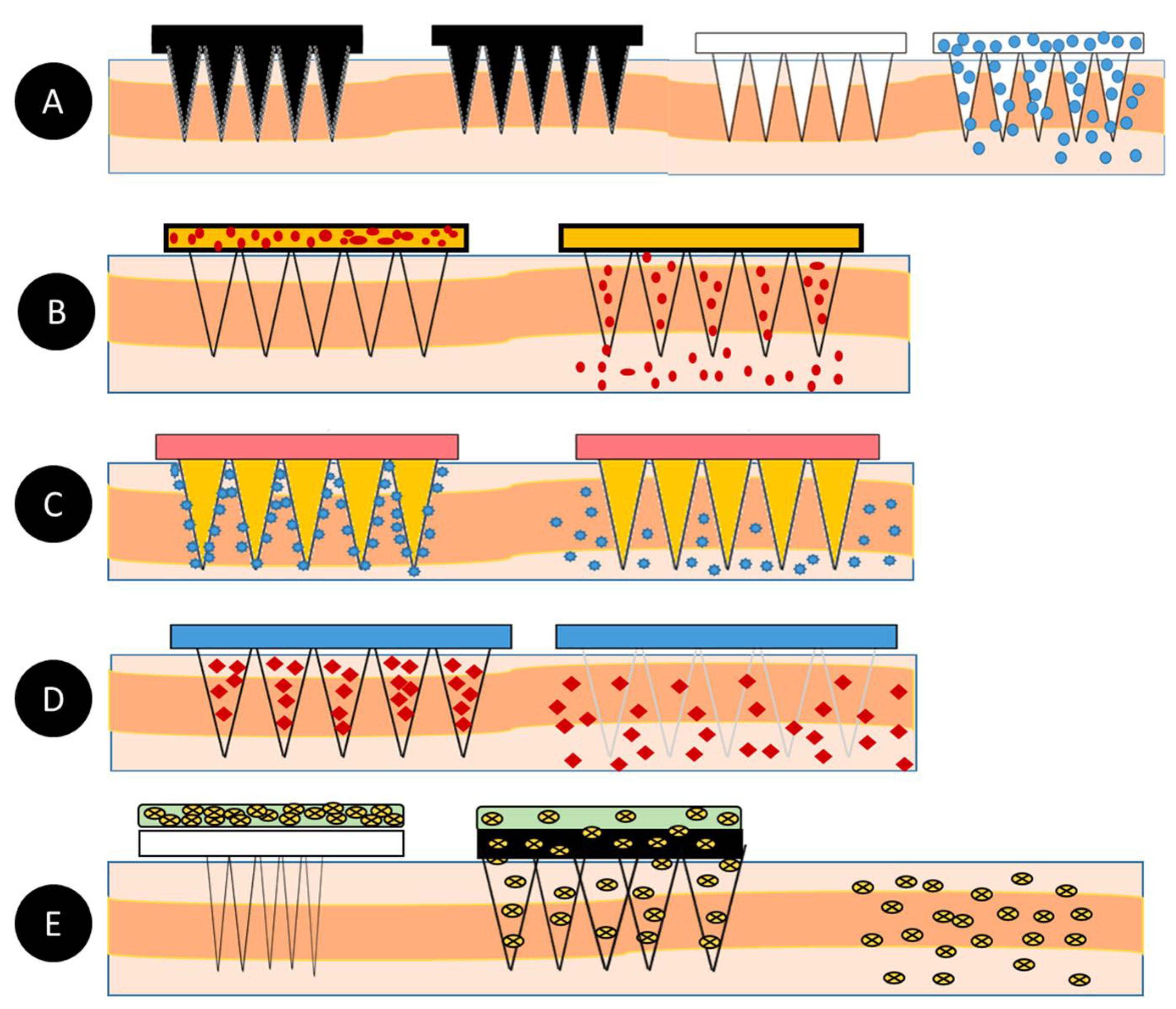
Microneedles (MNs) are minimally invasive, tiny needle devices that can be fabricated from a variety of materials, such as biomaterials, metals, polymers, ceramics, and composites [39,40,41][39][40][41], which are designed to penetrate the skin’s stratum corneum layer for various applications. The aim of microneedles is the delivery of bioactive materials, vaccines, and pharmaceutical agents, and the collection of bio-signals and substances from the body with minimal invasiveness. The administration of drugs through the gastrointestinal passage has not been the most efficient due to the poor absorption of orally ingested drugs and the pharmacokinetic activities of the body, which leaves only a fraction of the drug to achieve its intended therapeutic effect. Patients’ compliance with the conventional use of hypodermic needles has dropped significantly over the years due to the pain, anxiety, and discomfort that accompany their usage. A more appealing approach that offers the possibility of controlled release at the expense of the time of administration is transdermal drug delivery (TDD) using a microneedle patch. However, TDD is severely limited by the inability of most single drug particles to cross the skin at therapeutic rates due to the great barrier that is imposed by the skin’s stratum corneum layer [42]. In order to increase the skin’s permeability, different approaches have been investigated, including, but not limited to, chemical lipid enhancers, electric field employing iontophoresis, and electroporation to pressure waves that are generated by ultrasound or photoacoustic effects [43]. An alternative approach involves creating a pathway of micron-scale needles that serves to create microscopic holes on the outermost layer, called the stratum corneum, by inserting microneedles that are made of silicon, metal, or polymeric material. Microneedle arrays are promising devices in transdermal drug delivery applications. Microneedles are designed to be able to create an easier passage to the rich blood supply in the lower dermal layers, allowing an easy, pain-free delivery of a wide range of medicines across the skin [44]. The advantages of microneedles include painless administration, faster healing, ease of administration, and more control over the rate of drug delivery. Microneedle patches are categorized into five types, as shown in Figure 1, which include the following: solid microneedles, coated microneedles, dissolvable microneedles, hollow microneedles, and hydrogel-based microneedles. Each microneedle type has particular fabrication procedures and application areas. The first report of the term “microneedle” dates back to 1921 (Chambers, 1921), as a means of the micro-dissection of echinoderm eggs [45].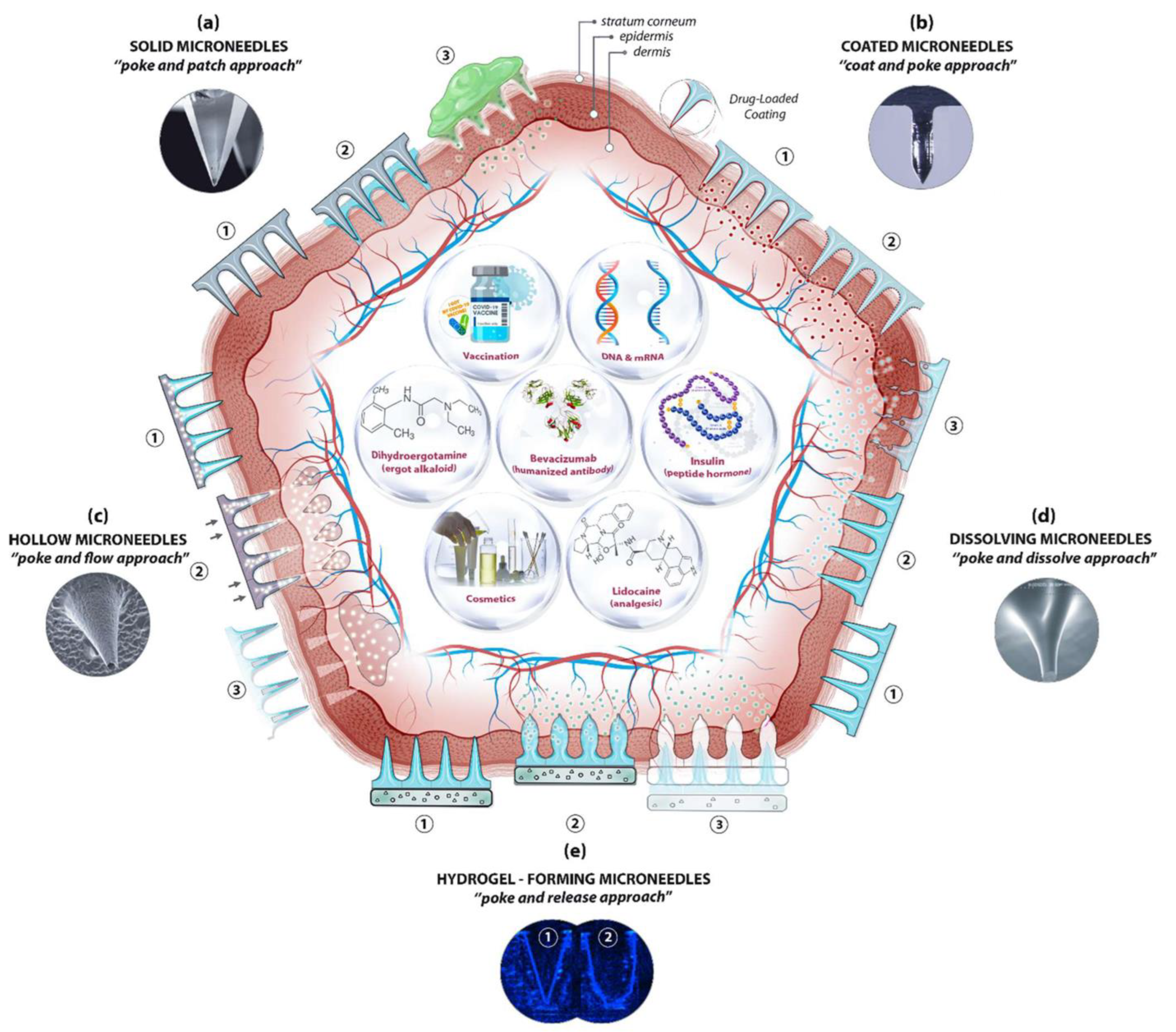

| S/N | MICRONEEDLE TYPE | Fabrication Techniques |
|---|---|---|
| 1. | Solid Microneedles | |
| Metal microneedles |
|
|
|
3. Classification of Microneedles
| S/N | Microneedle Type | Characteristics | Advantages | Disadvantages | Applications | Material | |||
|---|---|---|---|---|---|---|---|---|---|
| 1 | Solid | Creates holes in the skin for easy delivery of drugs to the lower layers of the skin | Can be easily fabricated | Prone to infection | Drug delivery and Cosmetics | Silicon Polymer Metal |
|||
| 2 | Hollow | The drug is filled into the empty space for controlled delivery | Able to handle a large volume of drug solution | Leakage and clogging could occur, and the needle design and insertion methods could pose a challenge | Diagnosis of disease | Silicon | |||
| Silicon microneedles |
| ||||||||
| 3 |
| ||||||||
| Coated | Based on its design, it carries a lower amount of drugs | Quick delivery of drugs to the skin | Susceptible to infections | Drug and Vaccine Delivery | Silicon | Polymer microneedles | |||
| 4 | Dissolving |
|
|||||||
| Rapid release of macromolecules | Can be easily administered to patients with a one-set application | Takes some time to dissolve, and requires expertise to manufacture | Drug delivery | Vaccine delivery Cosmetics |
Silicon | Ceramic microneedles |
| ||
| 5 | Hydrogel-forming | ||||||||
| Absorbs fluids (due to its hydrophilic nature) and swells, creating channels for the delivery of drug molecules | Can be applied to the skin leaving no residues, and has no clogging, unlike hollow microneedles | Potential for localized tissue damage, and has a slow swelling rate | ISF extraction | Transdermal drug delivery Disease treatment |
Polymer | 2. | Hollow microneedles |
|
|
| 3. | Coated microneedles |
|
|||||||
| 4. | Dissolvable microneedles |
|
|||||||
| 5. | Hydrogel-forming microneedles |
|
3.1. Solid Microneedles
3.2. Hollow Microneedles
3.3. Coated Microneedles
3.4. Dissolving Microneedles
3.5. Hydrogel-Forming Microneedles
References
- Aldawood, F.K.; Desai, S.; Chang, S. Additive Manufacturing of Compensator Devices for Radiation Therapy. In Proceedings of the 2020 IISE Annual Conference, New Orleans, LA, USA, 30 May–2 June 2020.
- Parupelli, S.K.; Desai, S. Understanding Hybrid Additive Manufacturing of Functional Devices. Am. J. Eng. Appl. Sci. 2017, 10, 264–271.
- Aljohani, A.; Desai, S. 3D Printing of Porous Scaffolds for Medical Applications. Am. J. Eng. Appl. Sci. 2018, 11, 1076–1085.
- Haeberle, G.; Desai, S. Investigating Rapid Thermoform Tooling Via Additive Manufacturing (3d Printing). Am. J. Appl. Sci. 2019, 16, 238–243.
- Desai, S.; Parupelli, S. Additive Manufacturing (3D Printing). In Maynard’s Industrial and Systems Engineering Handbook, 6th ed.; Springer International Publishing: Berlin/Heidelberg, Germany, 2022; ISBN 1260461564.
- Adarkwa, E.; Kotoka, R.; Desai, S. 3D printing of polymeric Coatings on AZ31 Mg alloy Substrate for Corrosion Protection of biomedical implants. Med. Devices Sens. 2021, 4, e10167.
- Slotwinski, J.A.; Campbell, T.A. Metrology for Additive Manufacturing—Opportunities in a Rapidly Emerging Technology; NOVA Science Publishers: Hauppauge, NY, USA, 2013; Volume 7, pp. 153–174.
- Ivanova, O.; Williams, C.; Campbell, T. Additive manufacturing (AM) and nanotechnology: Promises and challenges. Rapid Prototyp. J. 2013, 19, 353–364.
- McKenzie, J.; Desai, S. Investigating Sintering Mechanisms for Additive Manufacturing of Conductive Traces. Am. J. Eng. Appl. Sci. 2018, 11, 652–662.
- Parupelli, S.K.; Desai, S. Hybrid additive manufacturing (3D printing) and characterization of functionally gradient materials via in situ laser curing. Int. J. Adv. Manuf. Technol. 2020, 110, 543–556.
- Adarkwa, E.; Roy, A.; Ohodnicki, J.; Lee, B.; Roy, A.; Kumta, P.; Desai, S. 3D printing of drug-eluting bioactive multifunctional coatings for orthopedic applications. Int. J. Bioprinting 2023, 9, 0119.
- Aldawood, F.K.; Chang, S.X.; Desai, S. Design and Manufacture of a High Precision Personalized Electron Bolus Device for Radiation Therapy. Med. Devices Sens. 2020, 3, e10077.
- Kumar, V.; Dutta, D. An assessment of data formats for layered manufacturing. Adv. Eng. Softw. 1997, 28, 151–164.
- Desai, S.; Bidanda, B.; Bártolo, P. Metallic and ceramic biomaterials: Current and future developments. In Bio-Materials and Prototyping Applications in Medicine; Springer: Boston, MA, USA, 2008; pp. 1–14.
- Desai, S.; Shankar, M.R. Chapter 2 Polymers, Composites and Nano Biomaterials: Current and Future Developments. In Bio-Materials and Prototyping Applications in Medicine; Springer: Boston, MA, USA, 2008; pp. 15–26.
- Desai, S.; Harrison, B. Direct-Writing of Biomedia for Drug Delivery and Tissue Regeneration. Printed Biomaterials; Springer: New York, NY, USA, 2010; pp. 71–89.
- Perkins, J.; Xu, Z.; Smith, C.; Roy, A.; Kumta, P.N.; Waterman, J.; Conklin, D.; Desai, S. Direct Writing of Polymeric Coatings on Magnesium Alloy for Tracheal Stent Applications. Ann. Biomed. Eng. 2015, 43, 1158–1165.
- Desai, S.; Bidanda, B.; Bártolo, P.J. Emerging Trends in the Applications of Metallic and Ceramic Biomaterials. Bio-Materials and Prototyping Applications in Medicine; Springer: Berlin/Heidelberg, Germany, 2021; pp. 1–17.
- Desai, S.; Shankar, M.R. Emerging Trends in Polymers, Composites and Nano Biomaterial Applications. Bio-Materials & Prototyping Applications in Medicine; Springer International Publishing: Berlin/Heidelberg, Germany, 2020; ISBN 978-3-030-35875-4.
- Marquetti, I.D.S. Analyzing Bone Morphogenetic Protein-2 Adsorption Behavior on Hydrophobic Graphite Substrate. In Proceedings of the Brazilian Graduate Students and Scholars Conference (BRASCON), Columbus, OH, USA, 23–24 June 2018.
- Haeberle, G.; Desai, S. Additive Manufacturing (3D Printing) of Thermoform Tooling. Int. J. Mech. Prod. Eng. 2019, 7, 1–4.
- Perkins, J.; Yi, H.; Ye, S.H.; Wagner, W.; Desai, S. Direct Write Manufacturing of Controlled Release Coatings for Drug Eluting Cardiovascular Stents. J. Biomed. Res. Part A 2014, 102, 4290–4300.
- Marquetti, I. Molecular Modeling of Bone Morphogenetic Protein for Tissue Engineering Applications. In Proceedings of the Industrial Engineers Research Conference, Orlando, FL, USA, 19–22 May 2018; Volume 2, pp. 1108–1113.
- Marquetti, I.; Desai, S. Adsorption Behavior of Bone Morphogenetic Protein-2 on a Graphite Substrate for Biomedical Applications. Am. J. Eng. Appl. Sci. 2018, 11, 1037–1044.
- Adarkwa, E.; Desai, S.; Ohodnicki, J.M.; Roy, A.; Lee, B.; Kumta, P.N. Amorphous Calcium Phosphate Blended Polymer Coatings for Biomedical Implants. In Proceedings of the 2014 Industrial and Systems Engineering Research Conference, Montréal, QC, Canada, 31 May–3 June 2014.
- Luzuriaga, M.A.; Berry, D.R.; Reagan, J.C.; Smaldone, R.A.; Gassensmith, J.J. Biodegradable 3D printed polymer microneedles for transdermal drug delivery. Lab Chip 2018, 18, 1223–1230.
- Krieger, K.J.; Bertollo, N.; Dangol, M.; Sheridan, J.T.; Lowery, M.M.; O’Cearbhaill, E.D. Simple and customizable method for fabrication of high-aspect ratio microneedle molds using low-cost 3D printing. Microsyst. Nanoeng. 2019, 5, 42.
- Prasad, L.K.; Smyth, H. 3D Printing technologies for drug delivery: A review. Drug Dev. Ind. Pharm. 2015, 42, 1019–1031.
- Yang, J.; Liu, X.; Fu, Y.; Song, Y. Recent advances of microneedles for biomedical applications: Drug delivery and beyond. Acta Pharm. Sin. B 2019, 9, 469–483.
- Donnelly, R.F.; Singh TR, R.; Morrow, D.I.; Woolfson, A.D. Microneedle-Mediated Transdermal and Intradermal Drug Delivery; John Wiley and Sons: Hoboken, NJ, USA, 2012.
- Desai, S.; Lovell, M. Multiphysics Modeling of a Piezoelectric Bimorph Disc in a Direct Write Fabrication Process. In Proceedings of the ASME 2005 International Mechanical Engineering Congress and Exposition, Orlando, FL, USA, 5–11 November 2005; Volume 100, pp. 437–442.
- Adarkwa, E.; Desai, S. Scalable Droplet Based Manufacturing Using In-Flight Laser Evaporation. J. Nanoeng. Nanomanufacturing 2016, 6, 87–92.
- Desai, S.; Lovell, M. Modeling fluid–structure interaction in a direct write manufacturing process. J. Mater. Process. Technol. 2012, 212, 2031–2040.
- Cordeiro, J.; Desai, S. Process Parameter Studies of Molecular Dynamics Models to Control Substrate Wettability. In Proceedings of the International Manufacturing Science and Engineering Conference, Guangzhou, China, 28–29 November 2015.
- Desai, S.; Lovell, M. CFD Analysis of a Continuous Inkjet Print Head for Direct Write Fabrication. In Proceedings of the ASME 2007 International Mechanical Engineering Congress and Exposition, Seattle, WC, USA, 11–15 November 2007; Volume 13, pp. 209–213.
- Cordeiro, J.; Desai, S. Exploring Nano Scale Design Space with Molecular Dynamics Simulations. In Proceedings of the 2015 Industrial and Systems Engineering Research Conference, Nashville, TN, USA, 30 May–2 June 2015; p. 856. Available online: https://www.proquest.com/openview/15b4103286e4d16481a08298800d3854/1?pq-origsite=gscholar&cbl=51908 (accessed on 12 October 2022).
- Desai, S. Methods and Apparatus for Manufacturing Micro-and/or Nano-Scale Features. U.S. Patent Application 13/959,849, 28 November 2013.
- Desai, S.; Lovell, M. Coupled field analysis of a piezoelectric bimorph disc within a CIJ microfabrication process. In Proceedings of the 2006 IIE Annual Conference and Exhibition, Orlando, FL, USA, 20–24 May 2006.
- Erdem, Ö.; Eş, I.; Akceoglu, G.A.; Saylan, Y.; Inci, F. Recent Advances in Microneedle-Based Sensors for Sampling, Diagnosis and Monitoring of Chronic Diseases. Biosensors 2021, 11, 296.
- Sharma, S.; Hatware, K.; Bhadane, P.; Sindhikar, S.; Mishra, D.K. Recent advances in microneedle composites for biomedical applications: Advanced drug delivery technologies. Mater. Sci. Eng. C 2019, 103, 109717.
- Ali, R.; Mehta, P.; Arshad, M.; Kucuk, I.; Chang, M.W.; Ahmad, Z. Transdermal Microneedles—A Materials Perspective. AAPS PharmSciTech 2020, 21, 1–14.
- Bronaugh, R.L.; Maibach, H.I. (Eds.) Percutaneous Absorption: Drugs, Cosmetics, Mechanisms, Methods; CRC Press: Boca Raton, FL, USA, 2021.
- Prausnitz, M.R. Microneedles for transdermal drug delivery. Adv. Drug Deliv. Rev. 2004, 56, 581–587.
- Escobar-Chávez, J.J.; Bonilla-Martínez, D.; Villegas-González, M.A.; Molina-Trinidad, E.; Casas-Alancaster, N.; Revilla-Vázquez, A.L. Microneedles: A Valuable Physical Enhancer to Increase Transdermal Drug Delivery. J. Clin. Pharmacol. 2011, 51, 964–977.
- Dabbagh, S.R.; Sarabi, M.R.; Rahbarghazi, R.; Sokullu, E.; Yetisen, A.K.; Tasoglu, S. 3D-printed microneedles in biomedical applications. iScience 2021, 24, 102012.
- Avcil, M.; Çelik, A. Microneedles in Drug Delivery: Progress and Challenges. Micromachines 2021, 12, 1321.
- Walsh, L. Microneedling: A versatile and popular treatment option. J. Aesthetic Nurs. 2019, 8, 280–284.
- Gerstel, M.S.; Place, V.A. Drug Delivery Device. U.S. Patent US3964482A, 22 June 1976.
- Henry, S.; McAllister, D.V.; Allen, M.G.; Prausnitz, M.R. Microfabricated Microneedles: A Novel Approach to Transdermal Drug Delivery. J. Pharm. Sci. 1998, 87, 922–925.
- Kim, Y.C.; Park, J.H.; Prausnitz, M.R. Microneedles for drug and vaccine delivery. Adv. Drug Deliv. Rev. 2012, 64, 1547–1568.
- Aldawood, F.K.; Andar, A.; Desai, S. A Comprehensive Review of Microneedles: Types, Materials, Processes, Characterizations and Applications. Polymers 2021, 13, 2815.
- Verbaan, F.J.; Bal, S.M.; Van den Berg, D.J.; Groenink, W.H.H.; Verpoorten, H.; Lüttge, R.; Bouwstra, J.A. Assembled microneedle arrays enhance the transport of compounds varying over a large range of molecular weight across human dermatomed skin. J. Control. Release 2007, 117, 238–245.
- Ovsianikov, A.; Chichkov, B.; Mente, P.; Monteiro-Riviere, N.A.; Doraiswamy, A.; Narayan, R.J. Two Photon Polymerization of Polymer–Ceramic Hybrid Materials for Transdermal Drug Delivery. Int. J. Appl. Ceram. Technol. 2007, 4, 22–29.
- Wang, J.; Lu, J.; Ly, S.Y.; Vuki, M.; Tian, B.; Adeniyi, W.K.; Armendariz, R.A. Lab-on-a-Cable for electrochemical monitoring of phenolic contaminants. Anal. Chem. 2000, 72, 2659–2663.
- Park, J.H.; Allen, M.G.; Prausnitz, M.R. Biodegradable polymer microneedles: Fabrication, mechanics and transdermal drug delivery. J. Control. Release 2005, 104, 51–66.
- Ren, L.; Jiang, Q.; Chen, Z.; Chen, K.; Xu, S.; Gao, J.; Jiang, L. Flexible microneedle array electrode using magnetorheological drawing lithography for bio-signal monitoring. Sens. Actuators A Phys. 2017, 268, 38–45.
- Lee, K.; Lee, H.C.; Lee, D.S.; Jung, H. Drawing Lithography: Three-Dimensional Fabrication of an Ultrahigh-Aspect-Ratio Microneedle. Adv. Mater. 2010, 22, 483–486.
- Li, J.; Liu, B.; Zhou, Y.; Chen, Z.; Jiang, L.; Yuan, W.; Liang, L. Fabrication of a Ti porous microneedle array by metal injection molding for transdermal drug delivery. PLoS ONE 2017, 12, e0172043.
- Al-Muriesh, M.; Huang, C.Z.; Ye, Z.; Yang, J. Dermoscopy and VISIA imager evaluations of non-insulated microneedle radiofrequency versus fractional CO2 laser treatments of striae distensae. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 1859–1866.
- Tu, K.T.; Chung, C.K. Rapid prototyping of biodegradable microneedle arrays by integrating CO2 laser processing and polymer molding. J. Micromechanics Microengineering 2016, 26, 065015.
- Johnson, A.R.; Procopio, A.T. Low cost additive manufacturing of microneedle masters. 3D Print. Med. 2019, 5, 2.
- Waghule, T.; Singhvi, G.; Dubey, S.K.; Pandey, M.M.; Gupta, G.; Singh, M.; Dua, K. Microneedles: A smart approach and increasing potential for transdermal drug delivery system. Biomed. Pharmacother. 2019, 109, 1249–1258.
- Hashmi, S.; Hashmi, G.; Gaugler, R. Genetic Transformation of an Entomopathogenic Nematode by Microinjection. J. Invertebr. Pathol. 1995, 66, 293–296.
- Prausnitz, M.R.; Mikszta, J.A.; Raeder-Devens, J. Microneedles. In Percutaneous Penetration Enhancers; CRC Press: Boca Raton, FL, USA, 2005; pp. 253–270.
- Cheung, K.; Das, D.B. Microneedles for drug delivery: Trends and progress. Drug Deliv. 2014, 23, 2338–2354.
- Sabri, A.H.; Ogilvie, J.; Abdulhamid, K.; Shpadaruk, V.; McKenna, J.; Segal, J.; Scurr, D.J.; Marlow, M. Expanding the applications of microneedles in dermatology. Eur. J. Pharm. Biopharm. 2019, 140, 121–140.
- Tariq, N.; Ashraf, M.W.; Tayyaba, S. A Review on Solid Microneedles for Biomedical Applications. J. Pharm. Innov. 2021, 1–20.
- Mishra, P.; Gautam, V.; Sharma, R.K.; Tiwari, A.; Sawarkar, A. Microneedle: A useful tool for drug delivery system. J. Pharm. Phytochem. 2020, 9, 340–345.
- Suh, H.; Shin, J.; Kim, Y.-C. Microneedle patches for vaccine delivery. Clin. Exp. Vaccine Res. 2013, 3, 42–49.
- Mahato, R. Chapter 13—Microneedles in Drug Delivery. In Emerging Nanotechnologies for Diagnostics, Drug Delivery and Medical Devices; Elsevier: Amsterdam, The Netherlands, 2017; pp. 331–353.
- Mishra, R.; Maiti, T.K.; Bhattacharyya, T.K. Design and scalable fabrication of hollow SU-8 microneedles for transdermal drug delivery. IEEE Sens. J. 2018, 18, 5635–5644.
- van der Maaden, K.; Jiskoot, W.; Bouwstra, J. Microneedle technologies for (trans)dermal drug and vaccine delivery. J. Control. Release 2012, 161, 645–655.
- Zhang, P.; Jullien, G.A. Microneedle arrays for drug delivery and fluid extraction. In Proceedings of the 2005 International Conference on MEMS, NANO and Smart Systems, ICMENS 2005, Banff, AB, Canada, 24–27 July 2005; pp. 392–395.
- Zhang, P.; Dalton, C.; Jullien, G.A. Design and fabrication of MEMS-based microneedle arrays for medical applications. Microsyst. Technol. 2009, 15, 1073–1082.
- Ingrole, R.S.J.; Gill, H.S. Microneedle Coating Methods: A Review with a Perspective. J. Pharmacol. Exp. Ther. 2019, 370, 555–569.
- Duong, H.T.T.; Yin, Y.; Thambi, T.; Nguyen, T.L.; Phan, V.H.G.; Lee, M.S.; Lee, J.E.; Kim, J.; Jeong, J.H.; Lee, D.S. Smart vaccine delivery based on microneedle arrays decorated with ultra-pH-responsive copolymers for cancer immunotherapy. Biomaterials 2018, 185, 13–24.
- Nagarkar, R.; Singh, M.; Nguyen, H.X.; Jonnalagadda, S. A review of recent advances in microneedle technology for transdermal drug delivery. J. Drug. Deliv. Sci. Technol. 2020, 59, 101923.
- Tomono, T. A new way to control the internal structure of microneedles: A case of chitosan lactate. Mater. Today Chem. 2019, 13, 79–87.
- Ita, K. Transdermal Delivery of Drugs with Microneedles—Potential and Challenges. Pharmaceutics 2015, 7, 90–105.
- Donnelly, R.F.; Singh, T.R.R.; Garland, M.J.; Migalska, K.; Majithiya, R.; McCrudden, C.M.; Kole, P.L.; Mahmood, T.M.T.; McCarthy, H.O.; Woolfson, A.D. Hydrogel-Forming Microneedle Arrays for Enhanced Transdermal Drug Delivery. Adv. Funct. Mater. 2012, 22, 4879–4890.
- Hong, X.; Wu, Z.; Chen, L.; Wu, F.; Wei, L.; Yuan, W. Hydrogel Microneedle Arrays for Transdermal Drug Delivery. Nano-Micro Lett. 2014, 6, 191–199.
- Migdadi, E.M.; Courtenay, A.J.; Tekko, I.A.; McCrudden, M.T.C.; Kearney, M.-C.; McAlister, E.; McCarthy, H.O.; Donnelly, R.E. Hydrogel-forming microneedles enhance transdermal delivery of metformin hydrochloride. J. Control. Release 2018, 285, 142–151.
