Several key factors might improve adherence to insulin pump therapy: efficient communication between care provider and patients (including home-based video-visits), continuous diabetes education, family support and parental involvement, as well as informational, practical assistance, and emotional support from the society.
1. Introduction
The past few decades came with a rise in the prevalence of chronic diseases in children, and one of the most prevalent chronic diseases in this age group is type 1 diabetes mellitus (T1D). T1D, which is also the most prevalent endocrine condition in children and teenagers, is brought on by an autoimmune response that targets pancreatic beta cells over the course of several months or years. As a result, insulin output declines, which can result in a partial or, more frequently, an absolute deficit. The patients must receive exogenous insulin for the remainder of their lives
[1][2][3][1,2,3].
For patients and their caregivers, keeping the blood glucose level within the normal range can prove to be a challenge. This has served as motivation to find effective strategies to control T1D and prevent its consequences ever since insulin was discovered in 1921
[4]. The rapid development of diabetes technology over the past few decades includes continuous subcutaneous insulin infusion (CSII) as one of the most notable developments. The Diabetes Control and Complications Trial highlighted the value of rigorous therapy during childhood as it avoids and delays microvascular complications, despite the fact that the first insulin pump was created in the early 1970s
[5]. This led to an increase in the popularity of the device.
Notably, following extensive research in the last decades on insulin delivery systems, the International Society for Pediatric and Adolescents Diabetes (ISPAD) advocated for insulin pump therapy for diabetes management in children of all ages
[6]. Also, ISPAD recommended insulin pumps to improve glycemic controls, reduce the risk of chronic complications, and reduce episodes of hypoglycemia. In addition, real-time glucose sensors could be used to achieve better glycemic control
[6].
Nevertheless, ISPAD guidelines highlighted some barriers that should be addressed in adopting device-based therapy for children with diabetes
[6]. Adherence to insulin pump therapy was reported in 4% of cases, mainly due to pump wearability and anxiety. This issue could be overcome by adequate training by care providers, including progressive teaching from basic to advanced skills, and family support. Other barriers were linked to device-linked complications, such as malfunction, infusion failure, alarms, system occlusion, risk of ketoacidosis, and lipohypertrophy. Efficient communication and education offered by care providers and parents could be the solution to all these limitations, as insulin pump therapy benefits outweigh potential adverse events
[6].
2. Adherence Obstacles
The American Diabetes Association classifies adherence barriers into three categories: patient, medication, and system barriers
[7][11]. Good adherence to diabetes management is related to a better glycemic control. A meta-analysis that included 21 studies and 2429 adolescents concluded that better adherence is associated with better glycemic control, regardless of socioeconomic factors
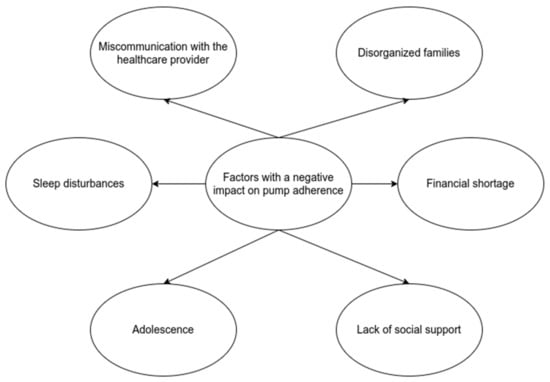
[8][9][12,13]. All the factors and barriers involved in achieving optimal adherence to insulin pumps are opportunities for intervention to increase glycemic control and, consequently, to increase the quality of life of young patients (
Figure 12).
Figure 12.
Factors with a negative impact on pump adherence.
3. Care Provider-Patient Relationship
When discussing with young patients and their parents, the term adherence is preferred over the term compliance. Efficient communication with doctors is part of successful therapy. Furthermore, a patient actively involved in making decisions regarding health issues has an increased adherence
[7][10][11,14]. Studying the SEARCH cohort of young patients with type 1 diabetes, researchers found that 48% of families felt that the providers did not discuss questions and concerns, 43% reported that communication with the diabetologist was insufficient, and 48% complained about the costs
[11][15].
Miscommunication and misunderstanding of the recommendations negatively influence the child’s adherence to treatment. This is an excellent intervention opportunity to increase glycemic control, and practitioners should try to eliminate communication barriers. In addition, closely related to communication is diabetes education. Studies emphasize the role of continuous diabetes education delivered by a multidisciplinary team, proving that it reduces hospitalization rates, emergencies, and complications
[12][16].
A small non-randomized study including 57 children with T1D concluded that home-based video visits are an excellent intervention to decrease HbA1c levels and increase adherence to treatment
[13][17]. Another study documented similar results, as telehealth improved glucose control in children and adolescents with type 1 diabetes
[14][18]. Moreover, one study reported excellent social receptivity regarding telephone and virtual visits for routine pediatric diabetes care
[15][19]. In addition, adherence is better when patients and their parents undergo insulin pump training in a pediatric endocrinology center
[16][20]. Therefore, telemedicine visits with both, parents and adolescents are feasible and can improve adherence to insulin pump therapy and glycaemic control. Nevertheless, these data are limited to small observational studies and large randomized controlled trials are required to confirm the results.
4. Family Role
Regarding the pediatric population and its adherence to therapy, it is crucial to consider that children are not the only managers of their treatment. Parents, other family members, teachers, and friends play an essential and decisive role in optimal diabetes management. Cross-sectional and prospective studies reported that patients with parents who are supportive, cohesive, collaborative in solving the problems, and willing to share the tasks, with an authoritative style of parenting, have good results in maintaining optimal metabolic control
[6][10][17][6,14,21].
On the other hand, patients with disorganized families, who must face conflicts with parents who are over or under-involved in a child’s disorder, are linked with poor treatment adherence
[8][18][12,22]. In addition, conflictual family relationships lead to depression among young people, while a collaborative parent-child relationship is associated with better adherence to CSII therapy and emotional stability
[6]. Another aspect consists of the socio-demographic characteristics of each family. For example, lower family income, ethnic and racial issues, and numerous members lead to less parental involvement in diabetes management with negative consequences. A low income is associated with less interaction between patients and doctors
[19][20][23,24].
5. Adolescence Period
Adolescents’ demand to feel autonomous rises as they mature, and, as a result, they start to take on more responsibilities related to their illness. Although the transfer in responsibility is a realistic aim, it is also associated with decreased adherence once parental supervision is reduced, particularly if parental disengagement occurs too soon. Despite the fact that children become more independent from their families once they grow up, thus impacting adherence to therapy, carbohydrate counting has a fundamental role in glycaemic control improvement
[21][22][23][24][25][26][25,26,27,28,29,30].
Psychosocial, emotional, and hormonal changes that occur during adolescence have an impact on therapeutic compliance. An ideal serum glucose level must be maintained despite insulin resistance brought on by hormonal changes. According to data from medical literature, the transition to self-care throughout adolescence is when glycemic control is least likely to be achieved. Only 21% of teenagers had HbA1c levels that were within the desired range
[27][31]. Parental participation appears to improve glycemic control and treatment adherence for diabetes, but it relies on how their children interpret this association: if the involvement is viewed as invasive, adherence declines; if it is viewed as collaborative, adherence improves
[17][27][21,31].
6. Social Support
Each child or adolescent’s social interactions are a crucial component of their lives, and they have an impact on how well they use their insulin pumps. Recently, social support for young individuals with diabetes has received more attention. There are three sorts of social support discussed: informational (advice), practical assistance, and emotional support. Young diabetics’ adherence to pump therapy is likely to worsen when they must deal with their peers’ unfavorable comments about managing their diabetes. Stigma is still a real issue that harms a child’s emotional well-being. However, although quantitative research links stigma with worsening glycemic control, qualitative investigations have produced mixed outcomes
[6][28][29][6,32,33].