Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Conner Chen and Version 1 by Waheb A. Jabbar.
The Internet of Wearable Things (IoWT) aims to improve people’s quality of daily life. It involves sensors fitted into wearable devices, monitoring the individual’s activity, health factors, and other things.
- IoT
- IoWT
- healthcare
1. Internet of Wearable Things
The Internet of Wearable Things (IoWT) aims to improve people’s quality of daily life. It involves sensors fitted into wearable devices, monitoring the individual’s activity, health factors, and other things. The data collected from the IoWT can be fed into medical infrastructure, giving clinicians remote access to their patients’ data as they go about their daily lives. Building on the internet of things (IoT) architecture, a novel integrative framework for IoWT is currently being developed. The IoWT is a revolutionary technology that has the potential to change the healthcare industry by creating an ecosystem for automated telehealth treatments [41][1].
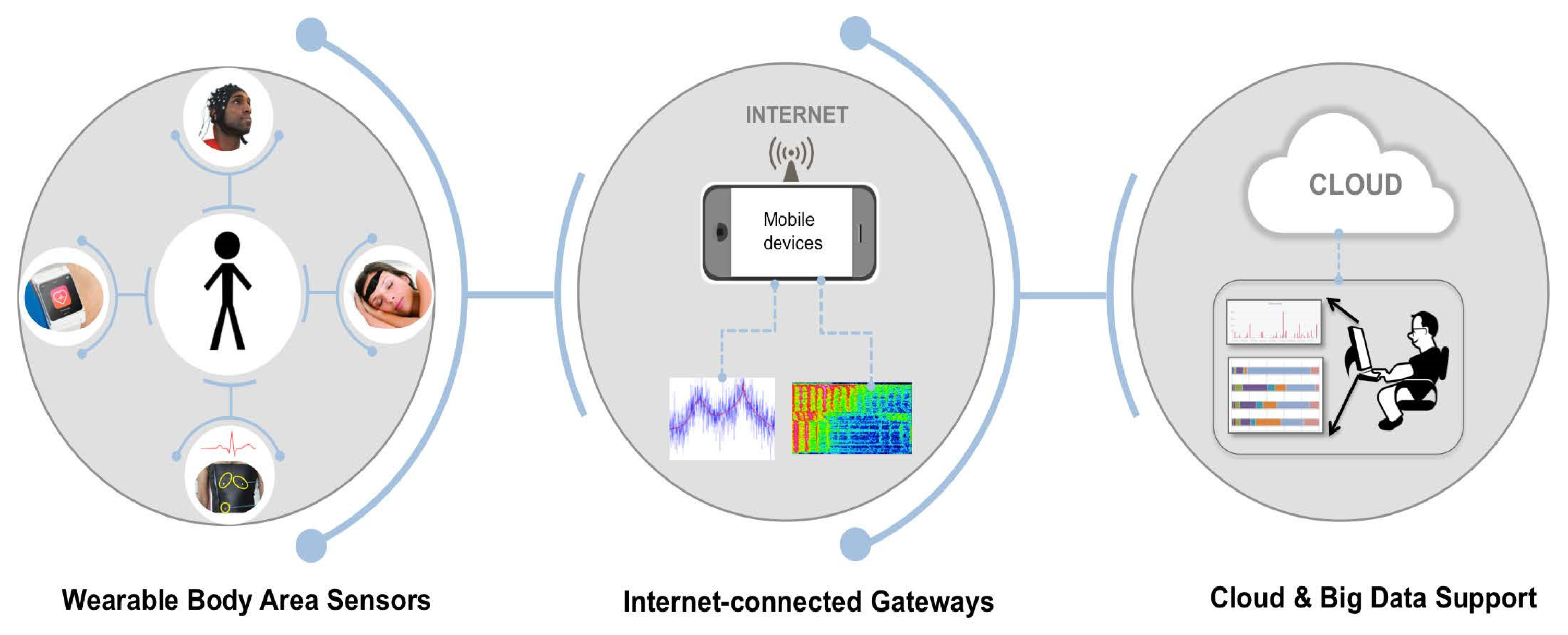
As shown in Figure 21, the architecture of the IoWT and its connections consists of three elements: the WBAN, the gateway connected to the Internet, and the cloud. The WBAN is a front-end component of IoWT that wraps around the body to collect health-related data unnoticed. The WBAN collects data from sensors in direct contact with the body or from sensors in the environment that can collect indirect data about a person’s behavior. The WBAN can either analyze the data or transmit them for remote analysis. In addition, mobile computing devices such as smartphones, tablets, and laptops must be connected to the Internet to send data to powerful computing resources [42][2].
2. Wireless Network Technologies for IoT Healthcare
Healthcare systems can be monitored remotely using various wireless network technologies. The existence and operation of IoT emerging technologies, such as RFID, wireless network technologies (BLE, Wi-Fi, Zigbee), and low-power wireless area network (LPWAN) technologies (such as LoRa and SigFox) are engaging in terms of the IoT’s long-term development and deployment. They enhance device connectivity to the Internet, and the efficiency of IoT application operation [43][3].
BLE, LoRa, and Zigbee are wireless sensor network technologies; meanwhile, to identify and trace products, RFID is used. BLE can transfer data between different mobile devices [44][4]. Communication methods can be long in their range (LoRa, SigFox, and Wi-Fi) or short-range (Bluetooth, RFID, and Zigbee) [24][5]. Due to new communication protocols being created exclusively for IoT devices, such as LoraWAN, NB-IoT, and Sigfox, it is anticipated that the popularity of these applications will increase, enabling a far-reaching remote monitoring system [11,45][6][7].
An essential component of the IoT is the WSN. The IoT, which has already been established, can connect things to the Internet, allowing humans to interact with computers and for computers to interact with other computers. Thus, the combination of the IoT and WSN facilitates machine-to-machine communication. Figure 32 illustrates the architecture of IoT with the WSN. It shows sensor nodes communicating with a gateway in a separate network. Many devices are linked to the gateway via Wi-Fi or the Internet, ensuring interoperability [46][8].
The researchers in [24][5] counted the existing wireless applications in connected healthcare facilities to study operational wireless methods for transmitting data across short distances. The system design and implementation of family mobile medical care are presented in this study. The Android mobile client, data transmission, and a system server are part of the system. Wireless data transfer is potentially possible, at least in theory. An example of the mobile healthcare system’s success is shown here. In the first place, family members’ sign characteristics might be collected via sensors on medical equipment. electrocardiograph (ECG, BP, SpO2), blood pressure (BP), blood-oxygen saturation (SpO2), respiration, and sleep are parameters of interest. The mobile terminal uploads data to a back-end Web server with a wireless network, Bluetooth, and Wi-Fi. Data storage, computation, and analysis are all handled by the MySQL database server [24][5]. A family member’s smartphone or tablet may be used to show data icons or text, making it easy for them to monitor their loved one’s health at any time and location. Family members may prevent significant health issues through early intervention, encouragement, and healthcare maintenance.
3. Wearable Sensors in Healthcare-Monitoring Systems
In real-time, the healthcare sector may use wearable devices to monitor and save patients’ activity and physiological functions. Such devices have one or more sensor nodes, but each sensor node typically has a radio transceiver, a low-speed processing unit, and small memory. The sensors can measure various physiological parameters and activity, including SpO2, BP and temperature, electrodermal activity (EDA), electrocardiograph (ECG), electromyography, HR heart rate (HR), and RR [2,47][9][10].
Bluetooth, infrared, near-field communication (NFC), RFID, Wi-Fi, and Zigbee wireless transceiver technologies can support wearable devices communicating with smartphones and other devices. The technology promotes care by facilitating remote diagnosis and monitoring [11][6]. An important issue of discussion in this period revolves around the IoT in healthcare. One of the essential parts of healthcare is identifying and treating illness. In order to achieve this, the body sensor network will be valuable. Additionally, the data may be accessible from any location in the world [8][11].
A wearable sensor gadget created by Vedaei can monitor and analyze the actions of patients. An IoT technology that measures social distance might help prevent a COVID-19 sufferer from becoming sick. Three layers of IoT sensors, machine learning algorithms, and smartphone apps are used to monitor BP, SpO2, cough rate, and temperature daily. The frameworks outlined by the authors helped the users keep a safe distance between themselves and the transmission of the virus and update their information often. A distance-monitoring system based on Radio Frequency (RF) was also presented in the research, which may be used in both indoor and outdoor contexts. In order to compare the findings under environmental restrictions, the authors looked at two alternative situations. Those who wrote the article claim to have helped expose COVID-19 [48][12].
Another study [49][13] demonstrated an IoT-connected wearable sensor network system for industrial outdoor workplace health and safety applications. Wearable sensors worn by the worker collect physiological and environmental data, which are transferred to the system operator and employees for monitoring and analysis. Data harvested from multiple workers wearing wearable sensors can be transferred through a LoRa network to a gateway. The LoRa network combines a Bluetooth-based medical signal-detecting network with a heterogeneous IoT platform. The authors describe the sensor node hardware and design, the gateway, and the cloud application. A heterogeneous wearable IoT device sensor network system for health and safety usage is shown in Figure 43.

3.1. Use Cases of Health-Monitoring Sensors
Medical science research is currently dominated by medical healthcare, which mostly relies on how it integrates with the IoT. This integration is receiving a lot of attention due to its crucial role in utilizing technological paradigms to save human lives. These integrated systems contain three crucial phases, namely, the modules for data collection, data processing, and data evaluation. Healthcare monitoring plays a significant role in the data collection module due to its active involvement in gathering data from various sources and specimens. Most healthcare-monitoring systems use sensors to obtain the necessary input data. The more concise and timely the data, the more accurate the results.
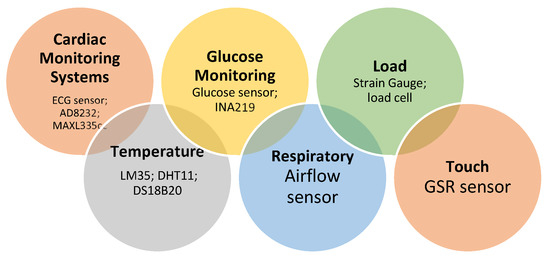
Sensors are employed for more than just data collection; they can also be used for various ongoing and post-monitoring tasks in IoT-based healthcare systems. Blood pressure, body temperature, pulse oximetry, and blood glucose are a few examples of heterogeneous wearable sensing devices developed to collect patients’ biomedical data [50][14] in the era of fast-growing IoT. The proper quality and development of these IoT-based healthcare-monitoring systems are directly related to reliable data from sensors or sensor networks, which necessitates using advanced signal-processing techniques, sensor data fusion, and data analytics. In medical science, sensors that measure heart rate, body temperature, and other things are used to find and diagnose diseases at the earliest stage.
It has been observed that health-monitoring sensors are utilized in various use cases of medical science for healthcare purposes, such as the monitoring of hemoglobin concentration, molecular diagnostics, clinical diagnosis of albumin-related diseases, heart-rate detection, blood-oxygen-saturation detection, respiratory-rate detection, anemia detection, Alzheimer’s disease, and many more.
There are many applications for wearable sensors. IoT-assisted wearables are widely used these days. The friendliness of such devices has created a boom in their application in all fields. With the healthcare field being no exception, the IoT’s exploits in healthcare are enormous. Various technologies are linked to existing technology that helps generate data for monitoring and analysis.
There is a lot of use cases for IoT-based sensors in real-time environments, which are mentioned below:
Use Cases/Applications
-
Heart-rate detection/Cardiac monitoring systems/Stroke
- 2.
-
Body-temperature measuring
- 3.
-
Activity recognition
- 4.
-
Blood-glucose monitoring and hemoglobin concentration
5. Respiration-rate detection and monitoring
Some writers employed sophisticated sensors that keep track of breathing patterns. A bio-impedance sensor can be useful [51,60,61][15][24][25].- 6.
-
Sleep monitoring
- 7.
-
Alzheimer’s disease monitoring and Anemia detection
- 8.
-
Molecular diagnostics and Clinical diagnosis
- 9.
-
Blood-oxygen-saturation detection
3.2. Classification of Health-Monitoring Sensors
With advancements in wireless communications, medical sensor technology, and data-collection methods, it is now possible to remotely monitor a person’s health by putting wearable technology on them and analyzing the data collected. These sensors and wearable devices can be integrated into various accessories such as clothing, wristbands, glasses, socks, hats, and shoes, as well as other devices such as smartphones, headphones, and wristwatches. Pawan Singh [75][39] classified medical sensors into two categories: contact sensors (i.e., on-body or wearables) and non-contact sensors (i.e., peripherals). Contact sensors are further classified into two sub-categories: monitoring and therapeutic. Again, non-contact sensors are further classified into three sub-categories. All the sub-categories are further classified based on their use. Figure 54 illustrates the classification of health-monitoring sensors with examples of their use.Primarily, health-monitoring sensors can be divided into contact (i.e., on-body) and non-contact (i.e., peripheral) sensors. Contact sensors are attached to the body to monitor physiological behaviors, chemical-level identification, and optical measurement-related monitoring. Contact sensors are also used in therapy-related monitoring such as medication, stimulation, and emergencies. Non-contact sensors are used for monitoring fitness- and wellness-related factors, behavior, and rehabilitation. An example of each type of monitoring is shown in Figure 54. The following are some of the medical applications that could benefit from the use of medical sensors and wearable devices [76][40]:
-
Monitoring vital signs in hospitals.
-
Aging in place and in motion.
-
Assistance with motor and sensory impairments.
-
Large-scale medical and behavioral research in the field.
- Monitoring vital signs in hospitals.
- Aging in place and in motion.
- Assistance with motor and sensory impairments.
- Large-scale medical and behavioral research in the field.
3.3. Performance Evaluation of IoT Sensors
Any healthcare-monitoring system’s sensors serve as its brain and heart. Thus, they must be reliable. Almost all types of sensors used should be small, quiet, accurate, have short data-transmission delays, use little power, and perform well overall. Wearable sensors must be both precise and compact, which presents a challenge. However, in case of wearable sensors, the more value is given to outputs, and they need to be reasonably accurate, too, so that the doctor can use these values to make decisions. Medical-grade sensors are large and difficult to transport and require specialized equipment and trained personnel [51][15]. Additionally, various IoT sensor-based applications constantly require authentication, security, and privacy. Numerous protocols are readily available on the market to assist with security and help offer some solutions over an extended period. Nevertheless, these integrated and crucial data-based apps’ security measures are constantly vulnerable to intrusion.
References
- Seneviratne, S.; Hu, Y.; Nguyen, T.; Lan, G.; Khalifa, S.; Thilakarathna, K.; Hassan, M.; Seneviratne, A. A survey of wearable devices and challenges. IEEE Commun. Surv. Tutor. 2017, 19, 2573–2620.
- Hiremath, S.; Yang, G.; Mankodiya, K. Wearable Internet of Things: Concept, architectural components and promises for person-centered healthcare. In Proceedings of the 2014 4th International Conference on Wireless Mobile Communication and Healthcare—Transforming Healthcare Through Innovations in Mobile and Wireless Technologies (MOBIHEALTH), Athens, Greece, 3–5 November 2014; pp. 304–307.
- Misran, N.; Islam, M.S.; Beng, G.K.; Amin, N.; Islam, M.T. IoT Based Health Monitoring System with LoRa Communication Technology. In Proceedings of the 2019 International Conference on Electrical Engineering and Informatics (ICEEI), Bandung, Indonesia, 9–10 July 2019; pp. 514–517.
- Dias, R.M.; Marques, G.; Bhoi, A.K. Internet of Things for Enhanced Food Safety and Quality Assurance: A Literature Review. Adv. Electron. Commun. Comput. 2021, 709, 653–663.
- Sahu, M.L.; Atulkar, M.; Ahirwal, M.K.; Ahamad, A. Vital Sign Monitoring System for Healthcare Through IoT Based Personal Service Application. Wirel. Pers. Commun. 2021, 122, 129–156.
- Philip, N.Y.; Rodrigues, J.J.P.C.; Wang, H.; Fong, S.J.; Chen, J. Internet of Things for In-Home Health Monitoring Systems: Current Advances, Challenges and Future Directions. IEEE J. Sel. Areas Commun. 2021, 39, 300–310.
- Almuhaya, M.A.; Jabbar, W.A.; Sulaiman, N.; Abdulmalek, S. A survey on Lorawan technology: Recent trends, opportunities, simulation tools and future directions. Electronics 2022, 11, 164.
- Desai, M.R.; Toravi, S. A Smart Sensor Interface for Smart Homes and Heart Beat Monitoring using WSN in IoT Environment. In Proceedings of the 2017 International Conference on Current Trends in Computer, Electrical, Electronics and Communication (CTCEEC), Mysore, India, 8–9 September 2017; pp. 74–77.
- Alekya, R.; Boddeti, N.D.; Monica, K.S.; Prabha, R.; Venkatesh, V. IoT based smart healthcare monitoring systems: A literature review. Eur. J. Mol. Clin. Med. 2021, 7, 2020.
- Malapane, T.J. A Cyber-Physical System for Smart Healthcare; University of Johannesburg: Johannesburg, South Africa, 2020.
- Jain, U.; Gumber, A.; Ajitha, D.; Rajini, G.; Subramanian, B. A Review on a Secure IoT-Based Healthcare System. In Proceedings of the Advances in Automation, Signal Processing, Instrumentation, and Control: Select Proceedings of i-CASIC, India, 27–28 February 2020; pp. 3005–3016.
- Vedaei, S.S.; Fotovvat, A.; Mohebbian, M.R.; Rahman, G.M.E.; Wahid, K.A.; Babyn, P.; Marateb, H.R.; Mansourian, M.; Sami, R. COVID-SAFE: An IoT-Based System for Automated Health Monitoring and Surveillance in Post-Pandemic Life. IEEE Access 2020, 8, 188538–188551.
- Wu, F.; Wu, T.; Yuce, M.R. Design and Implementation of a Wearable Sensor Network System for IoT-Connected Safety and Health Applications. In Proceedings of the 2019 IEEE 5th World Forum on Internet of Things (WF-IoT), Limerick, Ireland, 15–18 April 2019; pp. 87–90.
- Wan, J.; AAH Al-awlaqi, M.; Li, M.; O’Grady, M.; Gu, X.; Wang, J.; Cao, N. Wearable IoT enabled real-time health monitoring system. EURASIP J. Wirel. Commun. Netw. 2018, 2018, 298.
- Mamdiwar, S.D.; Shakruwala, Z.; Chadha, U.; Srinivasan, K.; Chang, C.-Y. Recent advances on IoT-assisted wearable sensor systems for healthcare monitoring. Biosensors 2021, 11, 372.
- Pal, A.; Visvanathan, A.; Choudhury, A.D.; Sinha, A. Improved heart rate detection using smart phone. In Proceedings of the 29th Annual ACM Symposium on Applied Computing, Gyeongju, Korea, 24–28 March 2014; pp. 8–13.
- Gogate, U.; Bakal, J. Healthcare monitoring system based on wireless sensor network for cardiac patients. Biomed. Pharmacol. J. 2018, 11, 1681.
- Arun, U.; Natarajan, S.; Rajanna, R.R. A novel IoT cloud-based real-time cardiac monitoring approach using NI myRIO-1900 for telemedicine applications. In Proceedings of the 2018 3rd International Conference on Circuits, Control, Communication and Computing (I4C), Bangalore, India, 3–5 October 2018; pp. 1–4.
- Pal, A.; Sinha, A.; Dutta Choudhury, A.; Chattopadyay, T.; Visvanathan, A. A robust heart rate detection using smart-phone video. In Proceedings of the 3rd ACM MobiHoc Workshop on Pervasive Wireless Healthcare, Bangalore, India, 29 July 2013; pp. 43–48.
- Gaoan, G.; Zhenmin, Z. Heart rate measurement via smart phone acceleration sensor. In Proceedings of the 2014 International Conference on Smart Computing, Hong Kong, China, 3–5 November 2014; pp. 295–300.
- Saha, R.; Biswas, S.; Sarmah, S.; Karmakar, S.; Das, P. A Working Prototype Using DS18B20 Temperature Sensor and Arduino for Health Monitoring. SN Comput. Sci. 2021, 2, 1–21.
- Adeniyi, E.A.; Ogundokun, R.O.; Awotunde, J.B. IoMT-based wearable body sensors network healthcare monitoring system. In IoT in Healthcare and Ambient Assisted Living; Springer: Berlin/Heidelberg, Germany, 2021; pp. 103–121.
- Fan, Z.; Zhou, Y.; Zhai, H.; Wang, Q.; He, H. A Smartphone-Based Biosensor for Non-Invasive Monitoring of Total Hemoglobin Concentration in Humans with High Accuracy. Biosensors 2022, 12, 781.
- Charlton, P.H.; Birrenkott, D.A.; Bonnici, T.; Pimentel, M.A.; Johnson, A.E.; Alastruey, J.; Tarassenko, L.; Watkinson, P.J.; Beale, R.; Clifton, D.A. Breathing rate estimation from the electrocardiogram and photoplethysmogram: A review. IEEE Rev. Biomed. Eng. 2017, 11, 2–20.
- Karlen, W.; Garde, A.; Myers, D.; Scheffer, C.; Ansermino, J.M.; Dumont, G.A. Estimation of respiratory rate from photoplethysmographic imaging videos compared to pulse oximetry. IEEE J. Biomed. Health Inform. 2015, 19, 1331–1338.
- Haghi, M.; Neubert, S.; Geissler, A.; Fleischer, H.; Stoll, N.; Stoll, R.; Thurow, K. A flexible and pervasive IoT-based healthcare platform for physiological and environmental parameters monitoring. IEEE Internet Things J. 2020, 7, 5628–5647.
- Pirani, E.Z.; Bulakiwala, F.; Kagalwala, M.; Kalolwala, M.; Raina, S. Android based assistive toolkit for alzheimer. Procedia Comput. Sci. 2016, 79, 143–151.
- Batsis, J.A.; Boateng, G.G.; Seo, L.M.; Petersen, C.L.; Fortuna, K.L.; Wechsler, E.V.; Peterson, R.J.; Cook, S.B.; Pidgeon, D.; Dokko, R.S. Development and usability assessment of a connected resistance exercise band application for strength-monitoring. World Acad. Sci. Eng. Technol. 2019, 13, 340.
- Wang, R.; Aung, M.S.; Abdullah, S.; Brian, R.; Campbell, A.T.; Choudhury, T.; Hauser, M.; Kane, J.; Merrill, M.; Scherer, E.A. CrossCheck: Toward passive sensing and detection of mental health changes in people with schizophrenia. In Proceedings of the 2016 ACM International Joint Conference on Pervasive and Ubiquitous Computing, Heidelberg, Germany, 12–16 September 2016; pp. 886–897.
- Ghatpande, N.S.; Apte, P.P.; Joshi, B.N.; Naik, S.S.; Bodas, D.; Sande, V.; Uttarwar, P.; Kulkarni, P.P. Development of a novel smartphone-based application for accurate and sensitive on-field hemoglobin measurement. RSC Adv. 2016, 6, 104067–104072.
- Li, P.; Lee, G.-H.; Kim, S.Y.; Kwon, S.Y.; Kim, H.-R.; Park, S. From diagnosis to treatment: Recent advances in patient-friendly biosensors and implantable devices. ACS Nano 2021, 15, 1960–2004.
- Song, J.; Pandian, V.; Mauk, M.G.; Bau, H.H.; Cherry, S.; Tisi, L.C.; Liu, C. Smartphone-based mobile detection platform for molecular diagnostics and spatiotemporal disease mapping. Anal. Chem. 2018, 90, 4823–4831.
- Hussain, S.; Chen, X.; Wang, C.; Hao, Y.; Tian, X.; He, Y.; Li, J.; Shahid, M.; Iyer, P.K.; Gao, R. Aggregation and Binding-Directed FRET Modulation of Conjugated Polymer Materials for Selective and Point-of-Care Monitoring of Serum Albumins. Anal. Chem. 2022, 94, 10685–10694.
- Muthuraj, B.; Hussain, S.; Iyer, P.K. A rapid and sensitive detection of ferritin at a nanomolar level and disruption of amyloid β fibrils using fluorescent conjugated polymer. Polym. Chem. 2013, 4, 5096–5107.
- Lu, W.; Bai, W.; Zhang, H.; Xu, C.; Chiarelli, A.M.; Vázquez-Guardado, A.; Xie, Z.; Shen, H.; Nandoliya, K.; Zhao, H. Wireless, implantable catheter-type oximeter designed for cardiac oxygen saturation. Sci. Adv. 2021, 7, eabe0579.
- Muratyan, A.; Cheung, W.; Dibbo, S.V.; Vhaduri, S. Opportunistic multi-modal user authentication for health-tracking IoT wearables. In Proceedings of the The Fifth International Conference on Safety and Security with IoT, Da Nang, Vietnam, 25 April 2021; pp. 1–18.
- Fang, D.; Hu, J.; Wei, X.; Shao, H.; Luo, Y. A smart phone healthcare monitoring system for oxygen saturation and heart rate. In Proceedings of the 2014 International Conference on Cyber-Enabled Distributed Computing and Knowledge Discovery, Shanghai, China, 13–15 October 2014; pp. 245–247.
- Nemcova, A.; Jordanova, I.; Varecka, M.; Smisek, R.; Marsanova, L.; Smital, L.; Vitek, M. Monitoring of heart rate, blood oxygen saturation, and blood pressure using a smartphone. Biomed. Signal Process. Control 2020, 59, 101928.
- Singh, P. Internet of things based health monitoring system: Opportunities and challenges. Int. J. Adv. Res. Comput. Sci. 2018, 9, 224–228.
- Ko, J.; Lu, C.; Srivastava, M.B.; Stankovic, J.A.; Terzis, A.; Welsh, M. Wireless sensor networks for healthcare. Proc. IEEE 2010, 98, 1947–1960.
- Rashmi, I.; Sahana, M.; Sangeetha, R.; Shruthi, K. IOT based Patient Health Monitoring System to Remote Doctors using Embedded Technology. Int. J. Eng. Res. Technol. 2020, 8, 230–233.
- Prakash, B.; Nagesh, M.; Mukunda, D.; Gowda, C. Arm Based Health Care Monitoring Services Using Wireless Network. Int. Res. J. Mod. Eng. Technol. Sci. 2020, 2. Available online: https://www.researchgate.net/profile/Mukunda-D-S/publication/341607121_ARM_BASED_HEALTH_CARE_MONITORING_SERVICES_USING_WIRELESS_NETWORK/links/5eca2d6792851c11a884f973/ARM-BASED-HEALTH-CARE-MONITORING-SERVICES-USING-WIRELESS-NETWORK.pdf (accessed on 5 October 2022).
- Misbahuddin, S.; Al-Ahdal, A.R.; Malik, M.A. Low-Cost MPI Cluster Based Distributed in-Ward Patients Monitoring System. In Proceedings of the 2018 IEEE/ACS 15th International Conference on Computer Systems and Applications (AICCSA), Aqaba, Jordan, 28 October–1 November 2018; pp. 1–6.
- Patil, H.; Manohare, S.; Magdum, S.; Gore, M.S. Smart Healthcare Monitoring and Patient Report Generation System Using IOT. Int. J. Res. Appl. Sci. Eng. Technol. 2020, 8. Available online: https://www.academia.edu/43408033/Smart_Healthcare_Monitoring_and_Patient_Report_Generation_System_using_IOT (accessed on 5 October 2022).
- Mhatre, P.; Shaikh, A.; Khanvilkar, S. Non Invasive E-Health Care Monitoring System Using IOT. Int. J. Innov. Res. Technol. 2020, 6, 307–311.
- Zaman, F.; Lee, S.; Rahim, M.K.; Khan, S. Smart Antennas and Intelligent Sensors Based Systems: Enabling Technologies and Applications; Hindawi: London, UK, 2019; Volume 2019.
More