The unprecedented scale of the current SARS-CoV-2/COVID-19 pandemic has led to an extensive—yet fragmented—assessment of its endocrine repercussions; in many reports, the endocrine aspects of COVID-19 are lumped together in intensive care unit (ICU) patients and non-ICU patients.
- critical illness
- COVID-19
- SARS-CoV-2
- human
- blood
- plasma
1. Introduction
2. Non-COVID-19 Critical Illness
The central nervous system, the endocrine system, and the immune system work together to mount the body’s response to stress and harmful stimuli. Briefly, the endocrine changes of the acute phase of the response to stress involve the secretion of catecholamines, changes in the pulsatility of growth hormone (GH) secretion, an increase in cortisol, changes in thyroid hormones, the reduction in the concentration of sulfate dehydroepiandrosterone, the lowering of luteinizing hormone, an increase in prolactin, and increased resistance to insulin. Critical illness entails considerable stress to patients; the body’s reaction includes an immediate increase in pituitary stress hormones, adrenocorticotropin (ACTH), GH, and prolactin (Figure 1).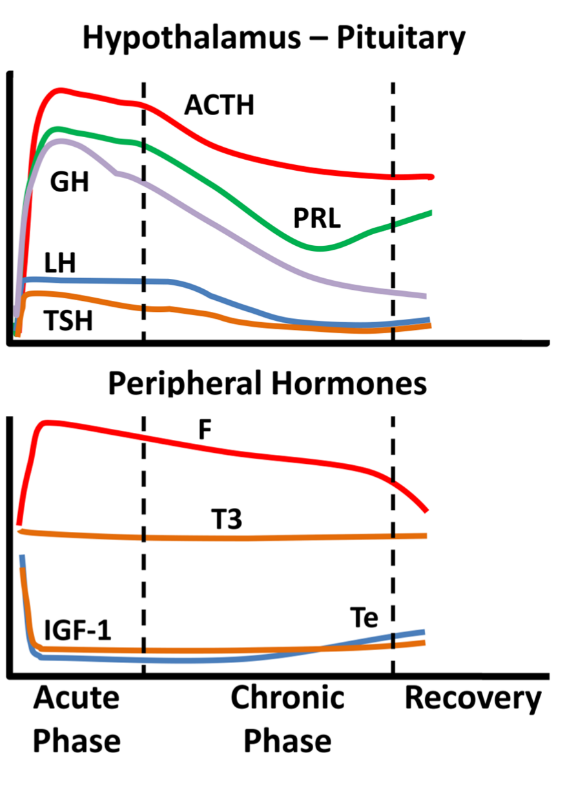
3. Endocrine Aspects of SARS-CoV-1 Infection
Scant data in a few published reports have been put forth regarding endocrine aspects of the serious infection caused by SARS-CoV-1. Low TSH, T3, cortisol, and estradiol as well as elevated prolactin (PRL), FSH, and LH blood levels have been reported. The thyroid was found to show extensive damage by the virus (with increased apoptosis and disturbed microarchitecture in follicular cells and absence of parafollicular cells), whereas in the pituitary glands of five patients, scant positive cells and diminished staining intensity of immunoreactivity for GH, TSH, and ACTH were noted; the inverse was noted for PRL, FSH, and LH. The relationship between SARS-CoV-1 and the adrenal glands is well-proven (the virus was found in the adrenal glands during autopsy studies). After recovery from infection, low ACTH and cortisol were noted in some patients. Nevertheless, this finding could not be ruled out as being an after-effect of glucocorticoid administration during active SARS-CoV-1 disease. Glucocorticoid administration could also be implicated in cases of patients with femoral neck osteonecrosis. Acute onset diabetes/hyperglycemia was observed in half of the patients in a small series with SARS-CoV-1 infection; the ACE2-virus-attaching protein has been found in pancreatic islets. Apparently, pancreatic islet cell function was compromised in the studied patients; in most of them normal glycemia was noted after three years of follow-up . The endocrine aspects of patients with SARS are summarized in Table 1.|
Affected Axis |
|
|---|---|
|
Hypothalamic–pituitary–thyroid |
Low TSH, low T3; Extensive thyroid gland damage; Diminished pituitary staining for TSH |
|
Hypothalamic–pituitary–growth |
Diminished pituitary staining for GH |
|
Hypothalamic–pituitary–adrenal |
Low F; Diminished pituitary staining for ACTH |
|
Hypothalamic–pituitary–gonadal |
Low E2; Elevated FSH, elevated LH; Increased pituitary staining for FSH, LH |
|
Hypothalamo-prolactin |
|
Affected Axis |
|||
|---|---|---|---|
|
Hypothalamic–pituitary–thyroid |
Low T3 or free T3, low free T4 and low TSH; NTIS or Thyrotoxicosis |
||
|
Hypothalamic–pituitary–growth |
Low IGF-1; Low IGF-1 and low GH associated with worse prognosis |
||
|
Hypothalamic–pituitary–adrenal |
High or low F |
||
|
Hypothalamic–pituitary–gonadal |
In women with high Te: worse prognosis; In men: high total Te or lower Te than control patients; low free Te and bioavailable Te, high E2 |
||
|
Elevated PRL; Increased pituitary staining for PRL |
|||
|
Glucose-insulin |
Acute onset transient diabetes/hyperglycemia; Impaired beta cell function |
Glucose-insulin |
Acute onset transient diabetes/hyperglycemia |
TSH: Thyroid Stimulating Hormone; T3: Triiodothyronine; F: Cortisol; ACTH: Adrenocorticotropic Hormone; E2: Estradiol; PRL: Prolactin; FSH: Follicle Stimulating Hormone; LH: Luteinizing Hormone; GH: Growth Hormone.
4. Endocrine Aspects of SARS-CoV-2 Infection
The thyroid gland and its function are among the most researched of endocrine aspects of Covid-19. A high serum cortisol level (above 31 μg/dL; 855 nmol/L) upon ICU admission was reported to be the harbinger of worse prognosis for Covid-19 patients. This is in contrast to a study, where cortisol was low in six of nine critically ill patients with Covid-19. TheVitamin D | |
Low (OH)25-vitamin-D3 |
TSH: Thyroid Stimulating Hormone; T4: Thyroxine; T3: Triiodothyronine; NTIS: Non-thyroidal illness syndrome; F: Cortisol; E2: Estradiol; FSH: Follicle Stimulating Hormone; LH: Luteinizing Hormone; GH: Growth Hormone; IGF-1: Insulin like Growth factor-1; Te: Testosterone.
References
- Van den Berghe, G. On the Neuroendocrinopathy of Critical Illness. Perspectives for Feeding and Novel Treatments. Am. J. Respir. Crit. Care Med. 2016, 194, 1337–1348.
- Ilias, I. Novel appearance of hyperglycemia/diabetes, associated with COVID-19. World J. Virol 2022, 11, 111–112.
