COVID-19 is an RNA virus that has caused a pandemic leading to death and disability on a global scale. The virus gains entry into the cell using host protein angiotensin-converting enzyme-2 (ACE-2) receptor. The viral envelope fuses with the cell membrane through the endosomal pathway, allowing the viral particle to enter the host cell, where it can release its RNA and replicate. After an initial asymptomatic period, common presenting signs and symptoms of COVID-19 infection are non-specific and may include those of a common cold or influenza such as fever, dry cough, myalgia, headache and fatigue. Sore throat and nasal congestion may also be noted. Gastrointestinal and other symptoms may occur and loss of sense of taste and smell is a frequent early symptom that may distinguish COVID-19 from other respiratory infections. The virus is highly contagious and there is no cure. In order to avoid transmission, social distancing, mask wearing and reduced person-to-person interaction are key. Definitive diagnosis is based on reverse-transcription PCR of nasopharyngeal and oropharyngeal swab samples. The clinical spectrum of the disease ranges from mild to moderate or severe. In order to minimize spread of COVID-19 to both patients and healthcare workers, virtual evaluation of suspected cases is being widely implemented and has necessitated an adjustment to the new medium by all participants. The use of virtual technology for real-time telemedicine assessment for COVID-19 provisional diagnosis and categorization of severity allows patients to receive an appropriate level of care without endangering others. We created a protocol for implementing a remote visit using a computer or mobile device. This enables patient assessement without direct contact to determine the need to visit a healthcare facility or alternatively, to be managed at home. If stable, the patient can isolate and be monitored so that should their condition worsen, they can be directed to in-person care at a hospital. Vigilance in checking on the patient's condition is crucial because those who develop severe COVID-19 may not experience dyspnea and other signs of rapid deterioration until about 5-8 days after symptom onset.
- Covid-19
- diagnosis
- cytokine
- telemedicine
- physical examination
1. INTRODUCTION
COVID-19 has spread rapidly across the globe, causing significant loss-of-life. Outcomes vary widely from asymptomatic, to flu-like symptoms, to pneumonia and respiratory failure. Coagulopathy is now recognized as a marker of disease severity in patients with COVID-19. It is imperative that we understand why infections in certain individuals are so much more severe than in others. The most common complication that develops in COVID-19 is bilateral pneumonia. There is an urgent need to distinguish those patients who will have a mild disease course from those who are at-risk for respiratory failure and pulmonary intravascular coagulopathy and to reduce morbidity and mortality due to this virus. COVID-19 primarily infects respiratory epithelial cells and, through interaction with the extracellular domain of the angiotensin converting enzyme 2 (ACE2) receptor, airway epithelium is a key site for viral entry. Spread is person-to-person through droplets of saliva or nasal discharge during coughing, speaking or sneezing. It may also be acquired by contact with contaminated environmental surfaces. In order to avoid unnecessary exposure and potential transmission of COVID-19 in healthcare facilities and physician offices, telehealth has taken on an increasingly important role.
2. DIAGNOSIS
The most common presenting symptoms of COVID-19 are respiratory-related and often non-specific (Table 1). In some patients, initial symptoms are gastrointestinal with diarrhea and/or nausea and vomiting. The gold standard method for definitive diagnosis is presence of SARS-CoV-2 nucleic acid upon reverse transcription polymerase-chain-reaction (RT-PCR) testing of specimens obtained by nasopharyngeal swab sampling. For this type of detection, which can determine whether the infection is active and the patient is contagious, the window is short and limited to the period of viral excretion. Immunoassays, based on the presence or absence of antibodies against the virus in the blood, may be useful in later stages of infection.
Table 1. COVID-19 Symptoms: initially may present like a common cold or flu
|
|
|
|
|
|
|
|
|
|
|
** Highly suspicious of COVID-19
3. THE TELEHEALTH VISIT
The initial telehealth encounter for suspected COVID-19 is focused on acute patient assessment and management (Table 2, Table 3 and Table 4).
Table 2. Telemedicine Evaluation
|
|
|
|
|
Table 3. Covid-19 Assessment Questions
| Two highest priority questions (Yes to either one) - -Do you have a cough? -Do you have shortness of breath or difficulty breathing? |
| Seven high priority questions (Yes to any two) – -Do you have a fever? -Do you have chills? -Do you have repeated shaking with chills? -Do you have muscle pain? -Do you have headache? -Do you have sore throat? -Do you have new loss of taste or smell? |
| Key symptoms that raise the index of suspicion for Covid-19 infection: |
| Answering yes to one of the highest priority questions or |
| Answering yes to 2 of the high priority questions |
Table 4. The Telemedicine Medical History
| Follows pattern of standard medical history - Chief complaint: Reason for the visit in the patient’s own words. -History of Present Illness (HPI): What symptoms are you experiencing and how long have you had these symptoms? |
| In addition to the symptoms covered earlier, are you experiencing any of the following? ♦ Diarrhea ♦ Abdominal pain ♦ Nausea or vomiting -Significant past medical history -Medications -Allergies -Family history |
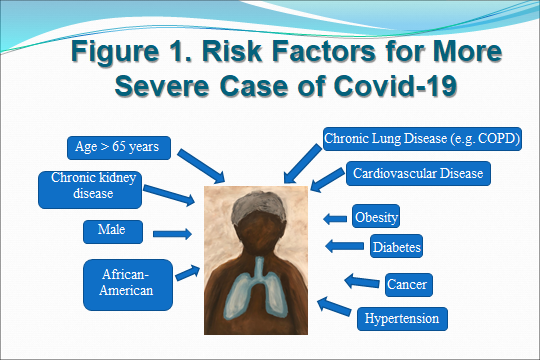
Particular attention should be given to specific aspects of the medical history and patient characteristics that increase vulnerability to severe illness from this viral infection. It has been established that certain groups of individuals are at a higher risk of developing serious complications from COVID‐19. Increased age and comorbidities are risk factors for becoming severely or critically ill (Figure 1).
The physical examination performed virtually cannot be as extensive as face-to-face, but substantial information can be gleaned, especially with the assistance of the patient (Table 5). The physician can observe the overall appearance and determine whether breathing is labored. Color of skin and mucous membranes can be visualized. Patient can report temperature and pulse and perhaps blood pressure.
Table 5. The Telemedicine Physical Exam
| Patient/Caregiver Facilitated Physical Exam -General: No apparent distress, nontoxic appearing -Head: Normocephalic, atraumatic -Eyes: Extraocular movements intact, no scleral icterus, pupils symmetrical, constricted or dilated -Ears: External ears normal -Neck: Full range of motion, trachea midline -Respiratory: Distress or use of accessory respiratory muscles** Listen for cough or wheezing. -Extremities: Full range of motion -Abdomen - Facilitated: nondistended and nontender -Neurologic: Alert, without focal deficits, normal gait - Psychologic: Normal mood and affect; appropriate relation with provider via camera |
4. LABORATORY TESTING
A large number of studies have shown that key hematologic data may be helpful in predicting who is likely to have a poor outcome from COVID-19 so that more aggressive measures can be instituted for these patients. A hypercoagulable state with propensity to form micro- and macro-thromboses is an ominous sign reflected in elevated D-dimer. Inflammatory markers such as C-reactive protein may also signal a more difficult course. Lab tests routinely administered in COVID-19 can be found in Table 6.
Table 6. COVID-19 Laboratory Testing
| Not all patients will require blood tests. |
| Lab tests relevant for these patients include: - Covid-19 PCR - CBC - Comprehensive Metabolic Panel - D-dimer (>2 times normal may be at higher risk of poor outcomes with thrombotic events, coagulopathy) - Erythrocyte sedimentation rate - C-reactive protein - Covid-19 IgG - Creatine kinase-MB fraction and troponin may also be measured as markers of possible myocardial injury |
5. CONCLUSIONS
The urgent need to evaluate persons for COVID-19 infection while limiting spread of this infectious disease has accelerated use of telemedicine and virtual visits by physicians, healthcare providers and patients. Telemedicine is a form of real-time, audio and visual communication that has shown its value during the pandemic and that will need to be scrutinized formally in well-designed studies with the goal of optimizing delivery and attaining the best possible outcomes.
In order to maintain good health through this pandemic and in general, see recommendations in Table 7.
Table 7. Advice for Health Maintenance During Pandemic
| - Balanced, nutritious diet and good hydration - Fewer processed, high-salt or high-sugar foods - Adequate vitamin D and C - Exercise – move your body as much as you can: dance, exercise classes online, yoga, Pilates, tai chi, stretching - Exercise on flat surfaces free of tripping hazards while wearing proper footwear. - Entertaining activities: painting, drawing, coloring, music, movies and time outdoors with social distancing - Video visits with friends and relatives –scheduled and part of routine - Do not neglect ongoing health needs. Consult with your doctor and dentist to ensure care delivery in a timely manner. |
