2. Extracellular Vesicles (EVs)
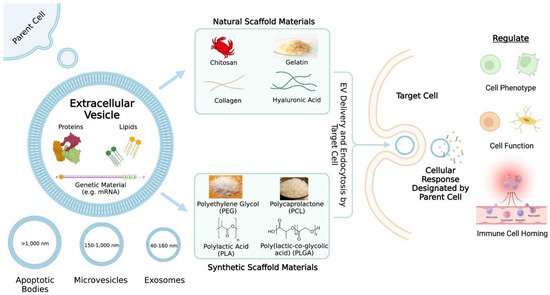
Extracellular vesicles are nanosized cell-derived membranous structures and can be categorized into several subclasses including exosomes (40–160 nm), microvesicles (150–1000 nm), and apoptotic bodies (>1000 nm)
[5] (
Figure 1). Exosomes are formed by the inward budding of endosomes and results in the generation of intraluminal vesicles within multivesicular bodies (MVBs)
[6]. When MVBs fuse with the plasma membrane, the intraluminal vesicles are released into the extracellular space and are then referred to as exosomes
[6]. It is unlikely that researchers will be able to capture live images of EV release in order to assign EVs to subclasses
[7]. Thus, the authors often refer to EV subclasses based on the physical characteristics (e.g., small EVs (sEVs)), biochemical composition (e.g., Annexin A5-stained EVs), conditions (e.g., hypoxic EVs), or cell of origin (e.g., hMSC EVs)
[7]. Ultimately, it is important to continue studying specific and reliable markers of EV subtypes, so that a consensus regarding nomenclature can be established.
Figure 1. An overview of extracellular vesicle (EV) delivery via scaffolds. The contents and categories of the extracellular vesicles as well as what the extracellular vesicles may regulate are described. Common natural and synthetic biomaterials for scaffold fabrication are highlighted.
3. Natural Biopolymer Scaffolds for Therapeutic EV Delivery
3.1. Sodium Alginate
Sodium alginate (SA) is a linear polysaccharide derived from brown seaweed
[8][55]. More specifically, SA is a derivative of alginic acid and is composed of α-1-guluornic (G) and 1,4-linked-β-D-mannuronic (M) monomers
[8][55]. Alginate has been used to deliver various classes of drugs including NSAIDs
[9][56], chemotherapeutics
[10][11][57,58], and anesthetics
[12][59]. Hormones such as insulin
[13][60] and salmon calcitonin
[14][61] have also been delivered via alginate. Furthermore, neuropeptides
[15][62], genetic material
[16][63], and probiotics
[17][64] have been delivered using alginate.
EV-laden alginate-based hydrogels have been studied for a wide range of therapeutic applications including diabetic wound healing
[18][37], peripheral nerve regeneration
[19][38], and myocardial infarction (MI)
[20][26]. Lv et al. delivered bone marrow mesenchymal stem cell (MSC)-derived small EVs (sEVs) to the heart using a natural sodium alginate hydrogel as a therapy for myocardial infarction. The hydrogels were embedded with sEVs by simply mixing the sEV solution with the sodium alginate solution prior to hydrogel formation with calcium chloride solution
[20][26]. Additionally, the authors found that hydrogels formed with 0.5% or 1% calcium chloride solutions resulted in nearly all of the sEVs being released by day 10 with a quick burst of sEV release during the first couple of days compared to a 2% calcium chloride solution
[20][26].
Lv et al. reasoned that hydrogels with a quicker sEV release profile would better suit a myocardial infarction model
[20][26]. The authors labeled sEVs and found through ex vivo imaging that sEVs embedded in the hydrogel (sEV-gel) were retained in the heart compared to freely injected sEVs
[20][26]. Lv et al. examined the expression levels of miRNAs (miR) related to anti-apoptosis and pro-angiogenesis and performed TUNEL staining; they found that treatment using the sEV-gel showed decreased cardiac cell apoptosis
[20][26]. Additionally, Lv et al. looked at the number of CD68+ macrophages as well as the ratio of CD206+ to CD68+ macrophages and found that the sEV-gel treatment promoted M1 to M2 macrophage polarization only a couple days after myocardial infarction
[20][26]. Furthermore, Lv et al. used CD31+ staining, α-SMA staining, and Western blotting to show that sEV-gel treatment promoted angiogenesis
[20][26]. Using echocardiography and histology, Lv et al. saw that the sEV-gel treatment resulted in improved cardiac function and enhanced scar thickness compared to only using sEVs
[20][26].
Overall, the authors demonstrated that the sEV-gel treatment promoted angiogenesis, reduced cardiac apoptosis and fibrosis, and improved cardiac function after MI
[20][26]. This
enst
rudy highlights the importance of using a scaffold to allow for an appropriate, efficient, and locally concentrated delivery of EVs, for without some type of retention system, administered EVs will be quickly cleared by the body and will have a minimal therapeutic effect.
3.2. Silk Fibroin
Silk fibroin (SF) is a hydrophobic protein from the
Bombyx mori silkworm that self-assembles into strong and resilient materials
[21][22][65,66]. Silk fibroin on its own is biocompatible, has controllable biodegradability, and has tunable mechanical properties
[23][67]. It also causes minimal inflammation of host tissue, is low-cost, and easy to use
[23][67]. Anti-proliferative
[24][68], anti-inflammatory
[25][26][69,70], anabolic
[26][70], and anti-retroviral drugs
[27][71] have been delivered using silk fibroin. Additional drugs include anti-inflammatory compounds such as curcumin
[28][29][72,73] and chemotherapeutics
[30][31][74,75]. Aside from drug delivery, SF has been utilized for the delivery of antibodies
[32][76], proteins
[32][33][76,77], hormones (e.g., insulin)
[34][78], genetic material
[35][79], and cells (e.g., mesenchymal stem cells)
[36][80].
Cunnane et al. examined the effect of human adipose-derived mesenchymal stem cell EVs (hADMSC EVs) on vascular cells in vitro
[37][33]. They found that the application of these EVs on smooth muscle cells and endothelial cells increased proliferation as well as migration in a dose-dependent manner
[37][33]. Cunnane et al. then vacuum-seeded EVs into porous silk-based tubular scaffolds by turning mounted scaffolds within a vacuum chamber and infusing the scaffolds with an EV isolate. Using a micro bicinchoninic acid protein assay and fluorescent imaging, they found that this method of seeding retained a greater amount of protein and increased EV coverage, respectively, within the scaffold compared to the soak-loading method
[37][33].
Cunnane et al. implanted the silk-based scaffolds into rat aortas to study the remodeling capacity of the EV-doped scaffolds. After 8 weeks, the explants were stained for cell, collagen, and elastin distribution
[37][33]. Additionally, elastin and collagen content assays were performed to quantify protein deposition within each explant
[37][33]. Their in vivo findings showed that the inclusion of EVs in the scaffold wall improved patency and matrix deposition, including more elastin and collagen production, which is crucial for neo-tissue formation
[37][33]. This
enst
rudy demonstrates that EVs play an effective bioinstructive role when incorporated into and delivered by SF-based vascular grafts.
3.3. Chitosan
Chitosan is a cationic polysaccharide derived from chitin and is made up of diglucose amine and N-acetyl glucose amine groups
[38][39][40][81,82,83]. Antibiotics
[38][40][81,83], antivirals
[41][84], and immunosuppressants
[42][85] have been delivered using chitosan. Additionally, chitosan has been utilized to deliver insulin
[39][82] and genetic material
[43][44][45][86,87,88].
Chitosan-based scaffolds have been used to deliver EVs to improve bone defect repair
[46][41], corneal diseases
[47][42], skin wound healing
[48][32], and articular cartilage injuries
[49][43]. Wu et al. developed chitosan-based thermosensitive hydrogels laden with bone mesenchymal stem cell (BMSC)-derived sEVs to accelerate osteogenesis and angiogenesis. After isolating the sEVs, Wu et al. characterized the sEVs through analyzing the size distribution and morphology of the sEVs as well as through Western blotting to detect sEV-specific surface markers
[46][41]. The authors also ensured that the sEVs could be internalized by BMSCs and HUVECs
[46][41]. In vitro experimentation included examining the ALP activity of BMSCs when exposed to sEVs. The results indicated the early-stage osteogenic differentiation of BMSCs when exposed to sEVs, shown by elevated ALP activity in the sEV groups
[46][41]. Furthermore, Wu et al. found through examining the mRNA (
OCN, OPN, and
Runx2) and protein (OCN, OPN, and RUNX2) levels that BMSC-sEVs can upregulate osteogenic gene expression
[46][41]. The authors also studied the migratory capability of HUVECs exposed to sEVs and found that the proliferation of HUVECs exposed to sEVs increased compared to the control group
[46][41]. Furthermore, mRNA and protein levels relevant to angiogenesis increased in cells exposed to sEVs
[46][41]. Wu et al. added β-glycerphosphate to chitosan to formulate a thermosensitive injectable hydrogel, and they found that sEVs embedded in this hydrogel showed a good slow-release performance of 80% sEV release on day 8, with a slowed release rate thereafter
[46][41].
The in vivo micro-CT results of a calvarial defect model showed that hydrogels embedded with sEVs resulted in a greater area of newly formed bone compared to other groups
[46][41]. Histological staining showed that there was newly formed bone in the sEV-hydrogel and hydrogel-only groups compared to the control group, which resulted in a defect mainly filled with fibrotic connective tissue
[46][41]. Immunohistochemical staining of bone defect sections indicated more CD31+ in the sEV-hydrogel group compared to the hydrogel-only group, which indicated new vessel formation within the bone defect
[46][41]. Overall, the in vivo experimentation demonstrated that sEVs promote calvarial defect repair and enhanced osteogenesis and angiogenesis
[46][41].
Wu et al. examined the potential cause of their observed results by studying the relationship between miR-21 and SPRY2. After performing the reporter assays and rescue experiments, they found that the angiogenic protein levels in cells transfected with miR-21 mimics were higher than the control cells
[46][41]. These experiments indicated that exosomal miR-21 may promote HUVEC migration and angiogenesis by targeting SPRY2
[46][41].
Overall, Wu et al. successfully developed a thermosensitive injectable chitosan-based hydrogel laden with BMSC-derived sEVs. The hydrogel promoted bone healing and served as a scaffold for sEVs
[46][41]. The sEV-loaded hydrogel promoted bone healing in vivo by enhancing angiogenesis, which may be mediated by miR-21 expression upregulation in sEVs and the regulation of SPRY2 by miR-21
[46][41]. This
enst
rudy highlights the potential of delivering EVs via scaffolds to promote bone regeneration and the importance of understanding the mechanism behind positive results to continue improving the therapeutic outcomes.
3.4. Collagen
Collagen is the most abundant protein in mammals
[50][89] and is composed of three intertwined α-chains
[51][90]. Some of the functions of collagen include cell adhesion and migration, tissue repair, and scaffolding
[52][91]. Collagen has proven to be useful in medical applications as a delivery tool. Similar to the natural biopolymers discussed thus far, collagen has been utilized to deliver drugs
[53][54][92,93], cells
[55][56][94,95], and bioactive substances with antioxidant properties
[57][96]. It is also possible to deliver growth factors using collagen
[58][59][97,98].
Collagen-based scaffolds have been utilized for therapeutic purposes including bone regeneration
[60][39] and endometrium regeneration
[61][40]. Xin et al. designed a collagen scaffold containing umbilical cord-derived mesenchymal stem cell (UC-MSC)-derived exosomes for endometrial regeneration in a rat endometrium-damage model
[61][40]. The authors confirmed successful exosome extraction through TEM, NTA, and Western blot
[61][40]. Xin et al. added exosome suspension dropwise to the collagen scaffold, and they obtained a sustained release profile with a majority of exosomes being released within 14 days
[61][40].
Xin et al. examined short-term and long-term outcomes from a rat endometrium-damage model involving exosome-collagen, collagen-only, exosome-only, and no treatment (control) groups
[61][40]. Through H&E staining, Xin et al. found that transplantation of the exosome-collagen scaffold promoted endometrium regeneration and glandular reconstruction, which was related to rapid cell proliferation and re-epithelialization
[61][40]. Additionally, Xin et al. performed immunostaining and Masson’s trichrome staining and found that transplantation of the exosome-collagen resulted in excellent neovascularization, reduced fibrosis formation, and promoted collagen remodeling
[61][40]. Through immunohistochemical staining and subsequent software analysis, Xin et al. found that a high number of anti-estrogen receptor α (ERα) positive cells and anti-progesterone receptor (PR) positive cells were present 30 days after exosome-collagen treatment, which suggests the rapid functional recovery of the regenerated endometrium
[61][40]. Furthermore, Xin et al. showed through Evans blue staining that the implantation of the exosome-collagen scaffold resulted in the structural and functional reconstruction of endometrium that could support implantation and the development of embryos in vivo
[61][40].
Xin et al. investigated the potential mechanisms behind the promising outcomes observed with exosome-collagen treatment. The authors found that exosome-collagen treatment promoted the macrophage infiltration within 7 days, with high numbers of M1 macrophages in the exosome-collagen and collagen-only groups within 3 days, likely due to the immunogenicity of the implanted collagen scaffold
[61][40]. Additionally, the exosome-collagen group showed the highest numbers of M2 macrophages within 7 days, indicating that exosome incorporation may have induced the polarization of macrophages to the M2 phenotype
[61][40]. Furthermore, Xin et al. examined the M1 and M2 macrophage-related cytokines. When looking at the M1-related cytokines, they found that the inclusion of exosomes in the scaffold eased inflammation due to the foreign body reaction to collagen within 7 days
[61][40]. Furthermore, there was an enhanced expression of M2-related cytokines with exosome-collagen transplantation. Altogether, transplantation of the exosome-collagen scaffold promoted M1 macrophage infiltration during the early stages of wound healing and induced macrophage transition from an M1 to a M2 phenotype during a later stage of healing
[61][40].
Through analyzing their RNA-Seq data against a publicly-available database, Xin et al. identified a top candidate related to macrophage immunomodulation (miR-223-3p), which has been reported to promote macrophage polarization to an M2 phenotype, as the key cargo within exosomes
[61][40]. Xin et al. believe that miR-223-3p may target
Stmn1 within macrophages to confer functional benefits
[61][40]. Overall, Xin et al. developed a local exosome chitosan-based delivery system that could promote endometrium regeneration and fertility restoration
[61][40]. They found that this system involved a mechanism-of-action related to M2 macrophage polarization with miRNA-223-3p serving as a top key component within exosomes
[61][40].
3.5. Hyaluronic Acid
Hyaluronic acid (HA) is a linear polysaccharide with repeating units of D-glucuronic acid and
N-acetyl-D-glucosamine
[51][90]. HA is characterized by a strong water binding ability and is found in the extracellular matrix
[51][90]. HA has been used to deliver anti-bacterial drugs
[62][99], immunosuppressants
[63][100], anabolic and anti-inflammatory compounds
[26][64][65][66][67][70,101,102,103,104]. The delivery of chemotherapeutics using hyaluronic acid have been well-studied
[68][69][70][71][105,106,107,108]. Examples of these delivered therapeutics include doxorubicin
[72][73][74][75][109,110,111,112], cisplatin
[76][113], and cantharidin
[77][114]. Additionally, anti-oxidants
[78][115], flavonols
[79][116], anti-photoaging agents
[80][117], and peptides
[81][118] have been delivered using HA. Furthermore, HA has been used to deliver cells (including cell secretome)
[82][83][119,120], genetic material
[75][112], growth factors
[65][84][102,121], and hormones
[85][122].
Hyaluronic acid-based scaffolds have been used to deliver EVs as a therapy for tendon repair
[86][45] and osteoarthritis cartilage injuries
[87][46]. K. Song et al. isolated exosomes from tendon derived stem cells (TDSC-Exos), loaded a hyaluronic acid scaffold with the exosomes, and studied the therapeutic effects of this system for tendon repair. The authors examined exosome size distribution, morphology, and the presence of exosome-related markers (CD9, CD63, CD81, and TSG101) using Western blot
[86][45]. They also used the protein concentration of exosomes as a representation of exosome concentration throughout the study
[86][45]. The authors then studied the effects of TDSC-Exos on the proliferation and function of tenocytes in vitro and found that high concentrations of exosomes (100 μg/mL) could protect tenocytes from oxidative stress and serum deprivation
[86][45]. Additionally, the treatment of tenocytes with TDSC-Exos increased type 1 collagen production and elevated tendon-specific marker (
Scx, Col1a1, and
Dcn) expression
[86][45]. The authors then produced a scaffold by irradiation, containing a uniform exosome distribution that could serve as a sustained exosome-release system (50% of exosomes retained after 14 days)
[86][45].
Song et al. then created a rat tendon defect model and used the hyaluronic scaffold (pHA) or the hyaluronic scaffold containing exosomes (pHA-TDSC-Exos) to fill the gap in the patellar tendons
[86][45]. Not only did they see decreased wound visibility with the pHA-TDSC-Exos group, but the authors found through H&E staining that the wound healing outcomes of this group were significantly better than the pHA and control groups and could enhance tendon repair in this model
[86][45]. Masson trichrome staining showed better collagen fiber arrangement with the pHA-TDSC-Exos group, and immunohistochemistry was used to show that this group promoted the early repair of the injured tendon with earlier type III collagen presence and reduction during the tendon healing process compared to the other groups
[86][45]. Furthermore, pHA-TDSC-Exos facilitated the restoration of the biomechanical properties of the injured tendon
[86][45].
With increasing evidence of the important roles miRNAs play during tissue repair, Song et al. performed RNA sequencing to find miRNAs that were expressed significantly higher in TDSC-Exos compared to tenocytes and chose to focus on miR-144-3p
[86][45]. Song et al. showed that miR-144-3p enhanced cell proliferation and migration. They found that miR-144-3p from TDSC-Exos played an important role in tendon repair by targeting ARID1A in tenocytes
[86][45]. ARID1A is a key component of the switch/sucrose non-fermentable ATP-dependent chromatin-remodeling complex, which plays a critical role in cell cycle modulation
[86][45]. MiR-144-3p is only one potential mechanism by which TDSC-Exos may exert therapeutic effects
[86][45]. Overall, Song et al. showed that TDSC-derived exosomes could promote tendon repair and that miR-144-3p transferred from these exosomes enhanced tenocyte proliferation and migration by targeting ARID1A.
3.6. Gelatin
Gelatin is a widely used natural biopolymer in regenerative medicine and tissue engineering
[88][123]. Similar to the natural biopolymers discussed above, gelatin has been utilized to deliver various types of drugs including anti-fungal/anti-yeast drugs
[89][124], anti-inflammatory agents
[90][91][92][125,126,127], antibiotics
[93][94][95][128,129,130], and chemotherapeutics
[96][97][98][99][131,132,133,134]. Other factors such as probiotics
[100][135], vitamins
[101][136], peptides
[102][137], and ions
[103][104][138,139] have been delivered using gelatin. Furthermore, researchers have used gelatin to deliver cells
[105][106][107][140,141,142], signaling molecules
[108][109][143,144], and genetic material
[110][111][145,146].
Gelatin-based scaffolds have been utilized for bone regenerative purposes
[112][44]. Man et al. epigenetically enhanced osteoblast-derived EVs with the histone deacetylase inhibitor Trichostatin A (TSA) to promote EV osteoinductive potency
[112][44]. In this study, Man et al. used gelatin methacryloyl (GelMA) functionalized with synthetic nanoclay laponite (LAP) (GelMA-LAP), which binds, stabilizes, and improves biofactor retention
[112][44]. They characterized these enhanced EVs (TSA-EVs) using TEM imaging, nano-flow cytometry, single-particle phenotyping, measuring EV protein content, and EV release kinetics from the GelMA-LAP hydrogel
[112][44]. The authors also found that the TSA-EVs released from the GelMA-LAP hydrogel were internalized by hBMSCs, and these EVs promoted hBMSC proliferation and migration
[112][44]. Furthermore, the authors found that these released TSA-EVs enhanced histone acetylation and mineralization of hBMSCs
[112][44]. Man et al. went further to evaluate the effects of TSA-EVs on hBMSC extracellular matrix mineralization within the GelMA-LAP hydrogels by assessing the ALP activity, collagen production, and calcium deposition
[112][44]. There was enhanced ALP activity in the hBMSCs within the TSA-EV hydrogels compared to the untreated osteoblast-EVs (MO-EV) and EV-free groups
[112][44]. hBMSC collagen production within the hydrogel was evaluated through picrosirius red staining, and TSA-EV treatment resulted in the greatest collagen content with a high dosage of TSA-EVs (50 µg/mL) (TSA-EV-50), resulting in the greatest collagen production
[112][44]. Furthermore, TSA-EV-50 gels resulted in greater calcium deposition compared to other groups, as found through alizarin red staining
[112][44].
Man et al. believe that the osteoinductive effect of TSA-EVs within the GelMA-LAP hydrogel is due to the 3D matrix (rather than a 2D matrix). More specifically, the 3D matrix elicits an altered cellular response to chemical and physical stimulation, so hBMSCs within the GelMA-LAP hydrogels may be more receptive to osteoinductive stimulation, which is induced by TSA-EVs compared to hBMSCs in 2D culture
[112][44]. Additionally, the 3D microenvironment of the GelMA-LAP hydrogel may have altered the epigenetic landscape of encapsulated hBMSCs, which may have primed the cells with enhanced differentiation capacity compared to the 2D cultured cells
[112][44]. Finally, the 3D microenvironment of the hydrogel and ECM produced by the hBMSCs likely influenced the sequestering of bioactive factors (e.g., EVs) within the secretome, which would further facilitate mineralization within the GelMA-LAP hydrogel
[112][44]. Altogether, these findings demonstrate the improved therapeutic potential of epigenetically enhanced EVs delivered via a gelatin-based scaffold for bone regeneration.
4. Synthetic Biopolymer Scaffolds for Therapeutic EV Delivery
4.1. Polyethylene Glycol (PEG)
PEG is an FDA-approved, hydrophilic, and flexible polymer that has been proven to be safe for use in biomedical applications
[113][150]. PEG has been used to deliver chemotherapeutics
[113][114][115][116][117][118][119][120][121][122][150,151,152,153,154,155,156,157,158,159], anti-inflammatory drugs
[123][160], antibiotics
[124][125][161,162], and bisphosphonates
[126][163]. Additionally, vitamins
[127][164], phenols
[128][165], and hormones
[129][166] have been delivered using PEG. Furthermore, PEG has been utilized for cell
[130][167], signaling molecule
[108][143], and genetic material delivery
[131][132][133][168,169,170].
Exosomes have been delivered via PEG hydrogels for cutaneous wound healing
[134][135][47,171]. Additionally, macrophages adopt polarization states in response to the local microenvironment
[134][47]. Based on Kwak et al.’s miRNA-sequencing data, exosomes derived from M1 macrophages (M1-Exos) and M2 macrophages (M2-Exos) contain proteins and miRNAs that are capable of shifting macrophage polarity
[134][47]. Thus, Kwak et al. utilized M2-Exos to induce the reprogramming of nearby proinflammatory M1 macrophages toward an anti-inflammatory M2 phenotype
[134][47]. They then encapsulated the M2-Exos in hydrolytically degradable PEG hydrogels (M2-Exogel) and found that the degradation time was adjustable from 6 to 27 days through controlling the crosslinking density and tightness
[134][47].
Kwak et al. used a full-thickness excisional wound model to assess the therapeutic effects of the M2-Exogel in vivo. They treated the wounds with saline, hydrogel alone, free exosomes, or M2-Exogel. Using immunohistochemistry and cytokine expression analyses, Kwak et al. showed the successful local transition of M1 macrophages to M2 macrophages within the lesion for more than 6 days
[134][47]. The M2-Exogel served as a long-term supply of the critical concentration of exosomes needed to initiate and sustain the reprogramming of M1 to M2 macrophages, ultimately contributing to improved wound healing
[134][47]. Kwak et al. found that localizing M2-Exos in the hydrogel led to rapid wound closure and increased healing quality compared to other groups
[134][47]. More specifically, the wound size significantly decreased after day 8 in the M2-Exogel group compared to other groups
[134][47]. Furthermore, they stained closed wound tissues with Masson’s trichrome and saw that the M2-Exogels produced superior results in the stable closure of full-thickness skin wounds as well as enhanced the dermal adipogenesis and hair follicle regeneration compared to freely injected exosomes
[134][47]. Altogether, the PEG hydrogel-based exosome delivery system serves as a method to locally regulate the polarization state of macrophages, which is critical for tissue homeostasis and proper wound repair
[134][47].
4.2. Polycaprolactone (PCL)
PCL is a linear, hydrophobic, aliphatic polyester with high mechanical strength and is biocompatible as well as biodegradable
[136][137][172,173]. Chemotherapeutics
[117][120][122][138][139][140][141][142][143][154,157,159,174,175,176,177,178,179], antimicrobials
[125][144][145][162,180,181], and anti-inflammatory drugs
[123][146][160,182] have been delivered using PCL. Furthermore, PCL has been used for the delivery of hypotensive agents
[147][183], protease inhibitors
[148][184], anticonvulsants
[136][172], and sulfonylureas
[149][185]. In addition to drug delivery, PCL has been used to deliver polyphenols
[150][186], antiretrovirals, and hormones
[151][187]. Similar to the previously discussed biopolymers, the delivery of genetic material
[132][152][153][169,188,189], growth factors
[154][190], and cells
[155][191] using PCL has been studied.
Synthetic biopolymer-based scaffolds containing EVs have been used to improve vascular performance and functionality (
Table 1). Wei et al. were interested in using heparin-functionalized vascular PCL grafts to enhance anti-thrombogenicity. The authors fabricated the tubular PCL grafts using electrospinning, modified the grafts with heparin, and loaded MSC-derived small EVs (MSC-sEVs) by soaking the scaffolds in sEV solution
[156][49]. The authors observed a uniform distribution of sEVs on the grafts using a confocal laser scanning microscope
[156][49].
Wei et al. examined the in vivo stability of the grafts by in vivo imaging using labeled sEVs and found that the bioluminescence intensities were higher in the heparinized scaffold group
[156][49]. The authors then studied the performance of the PCL vascular grafts modified with heparin and loaded with sEVs in a hyperlipidemia rat model
[156][49]. sEVs play many roles in this model. Wei et al. found that heparin enhanced anti-thrombogenicity while the addition of immunomodulatory sEVs inhibited thrombosis and calcification, which therefore improved the patency of the graft
[156][49]. The patency rate was measured using color doppler ultrasound, and H&E and von Kossa staining was used for calcification detection
[156][49]. Additionally, bioactive molecules (e.g., VEGF and miRNA 126) from the MSC-sEVs enhanced endothelium and vascular smooth muscle regeneration, shown through H&E staining and immunofluorescence staining with the CD31 antibody, α-SMA antibody, and myosin heavy chain
[156][49]. Furthermore, flow cytometric analysis revealed that sEVs induced polarization from pro-inflammatory and atherogenic M1 macrophages to anti-inflammatory and anti-osteogenic M2c macrophages
[156][49]. This
enst
rudy further highlights how synthetic biomaterials can be enhanced using EVs to create translational scaffolds for regenerative medicine.
4.3. Poly(Lactic-Co-Glycolic Acid) (PLGA)
PLGA is a copolymer that is similar to PCL in that it is a biocompatible, biodegradable, and flexible biopolymer
[157][158][192,193]. The delivery of antibiotics
[159][160][161][162][163][194,195,196,197,198] and chemotherapeutics
[164][165][166][167][168][169][199,200,201,202,203,204] using PLGA has been well-studied. Dopamine agonists
[170][205], anticonvulsants
[171][206], statins
[172][207], and immunosuppressants
[173][208] have also been delivered using PLGA. Furthermore, growth factors
[174][209], various proteins
[175][176][177][210,211,212], hormones
[178][179][213,214], genetic material
[180][215], and vaccines
[181][216] have been delivered using PLGA.
PLGA scaffolds containing EVs have been studied to improve bone defects
[182][52] and chronic kidney disease
[183][51]. Ko et al. designed a PLGA-based scaffold to deliver stem cell-derived EVs for kidney regeneration. The composite scaffold was composed of PLGA, magnesium hydroxide, and decellularized porcine kidney extracellular matrix, and polydeoxyribonucleotide (PDRN) and was fabricated using ice particle leaching
[183][51]. The scaffold was enhanced with EVs that were derived from TNF-α/IFN-γ-primed UC-MSCs (TI-EVs)
[183][51]. Ko et al. characterized the EVs by shape and size. They then studied the effector molecules within the EVs; more specifically, Ko et al. focused on proteins within TI-EVs and unprimed EVs (UC-EVs). The results indicated that treating UC-MSCs with TNF-α/IFN-γ enhanced the cellular uptake capabilities of secreted EVs and induced changes in protein cargo, which is indicative of kidney tissue regeneration
[183][51].
In a partial nephrectomy mouse model, the scaffold containing PDRN and EVs induced glomerular regeneration and the restoration of kidney function
[183][51]. More specifically, the kidney developmental factors (Pax2, Wt1, and Emx2) increased in expression with PME/PDRN/TI-EV scaffold treatment
[183][51]. Additionally, there was an increase in the population of Pax2-expressing host cells, which indicates that the scaffold can facilitate host renal stem/progenitor cell infiltration
[183][51]. Furthermore, there was an increased expression of pro-angiogenic growth factors (FGF2, HGF, and VEGF) in the PME/PDRN/TI-EV scaffold group
[183][51]. Ko et al. determined the total number of functional glomeruli using H&E staining, with the PME/PDRN/TI-EV group showing the best results
[183][51]. They then examined renal function recovery by evaluating the serum creatinine and blood urea nitrogen (BUN) levels. They found significantly better metabolic function in the PME/PDRN/TI-EV group
[183][51]. Furthermore, the glomerular filtration rate (GFR) was restored in the PME/PDRN/TI-EV group (227.2 μL/min) to a level similar to that of native mice (232.5 μL/min)
[183][51]. These results show structural and functional kidney tissue regeneration with the use of the PME/PDRN/TI-EV scaffold. Overall, the biochemical cues from TI-EVs and PDRN as well as the biophysical cues from the PLGA scaffold serve as potential tissue engineering platforms for kidney tissue regeneration
[183][51].
4.4. Poly(L-Lactide) (PLLA)
PLLA degrades by nonenzymatic hydrolysis and its by-products are eliminated via normal cell metabolism
[184][217]. Thus, it is biodegradable and biocompatible. The delivery of antibiotics
[185][186][187][188][218,219,220,221] and chemotherapeutics
[189][190][191][192][193][222,223,224,225,226] using PLLA has been frequently studied as well as anti-inflammatory drugs
[194][227], anti-psychotics
[195][228], acetylcholinesterase inhibitors
[196][229], and ocular disease therapeutics
[197][198][230,231]. In addition to drug delivery, cells
[199][200][232,233], growth factors
[201][202][203][204][234,235,236,237], and genetic material
[205][238] have been delivered using PLLA. Furthermore, PLLA has been utilized to deliver hormones and fertilizer
[206][239].
Swanson et al. engineered a biodegradable PLLA-based delivery platform to control the release of exosomes from microspheres to promote craniofacial bone healing. More specifically, they used PLGA and PEG triblock copolymer microspheres to encapsulate and control the timed release of human dental pulp stem cell (hDPSC)-derived exosomes
[207][54]. This delivery platform was integrated with a 3D tissue engineered PLLA scaffold. They found that microspheres containing exosomes demonstrated a linear and consistent release profile over a longer period of time when attached to a PLLA scaffold compared to freely suspended microspheres
[207][54]. They also found through NTA and TEM that the exosomes maintained their characteristic diameter and morphology throughout their encapsulation and release
[207][54]. Furthermore, Swanson et al. confirmed the in vitro bioactivity of the exosome-containing microspheres by culturing mouse BMSCs on nanofibrous scaffolds functionalized with the microspheres. They used the colorimetric calcium assay to examine hydroxyapatite mineralization and energy dispersive X-ray spectroscopy (EDX) to determine the spatial distribution of elements in the construct
[207][54]. It was found that microsphere-functionalized constructs and groups treated with exogenous exosomes showed an increased calcium phosphate content and a decreased proportion of organic components as minerals was deposited
[207][54].
Furthermore, the authors demonstrated exosome functionality in vivo by implanting constructs in mice and subsequent staining (Masson’s Trichrome and von Kossa staining). This revealed that constructs with exosome-containing microspheres increased hECM deposition and promoted early mineralization compared to blank microsphere constructs and blank scaffolds, which attributes the function to the exosomes
[207][54]. Furthermore, the constructs were used in a calvarial bone defect model. After 8 weeks, the functionalized constructs were laden with cells, collagen-rich matrix, marrow-containing bone tissue, and were integrated with the host at 8 weeks
[207][54]. Additionally, the µCT of the skulls showed that localized delivery of the exosomes via microspheres in the scaffold resulted in the best regenerative outcome among the treatment groups
[207][54].
Overall, the functionalized scaffold system was able to recruit endogenous cells and stimulate bone tissue neogenesis in vivo
[207][54]. The exosomes used in this
enst
rudy provided pro-mineralization cues that guided local progenitor cells toward osteogenic differentiation both in vitro and in vivo
[207][54]. By incorporating exosomes into a synthetic biopolymer-based scaffold, researchers can work toward overcoming the inherent lack of biochemical cues in synthetic biomaterials to achieve therapeutic effects such as bone healing.