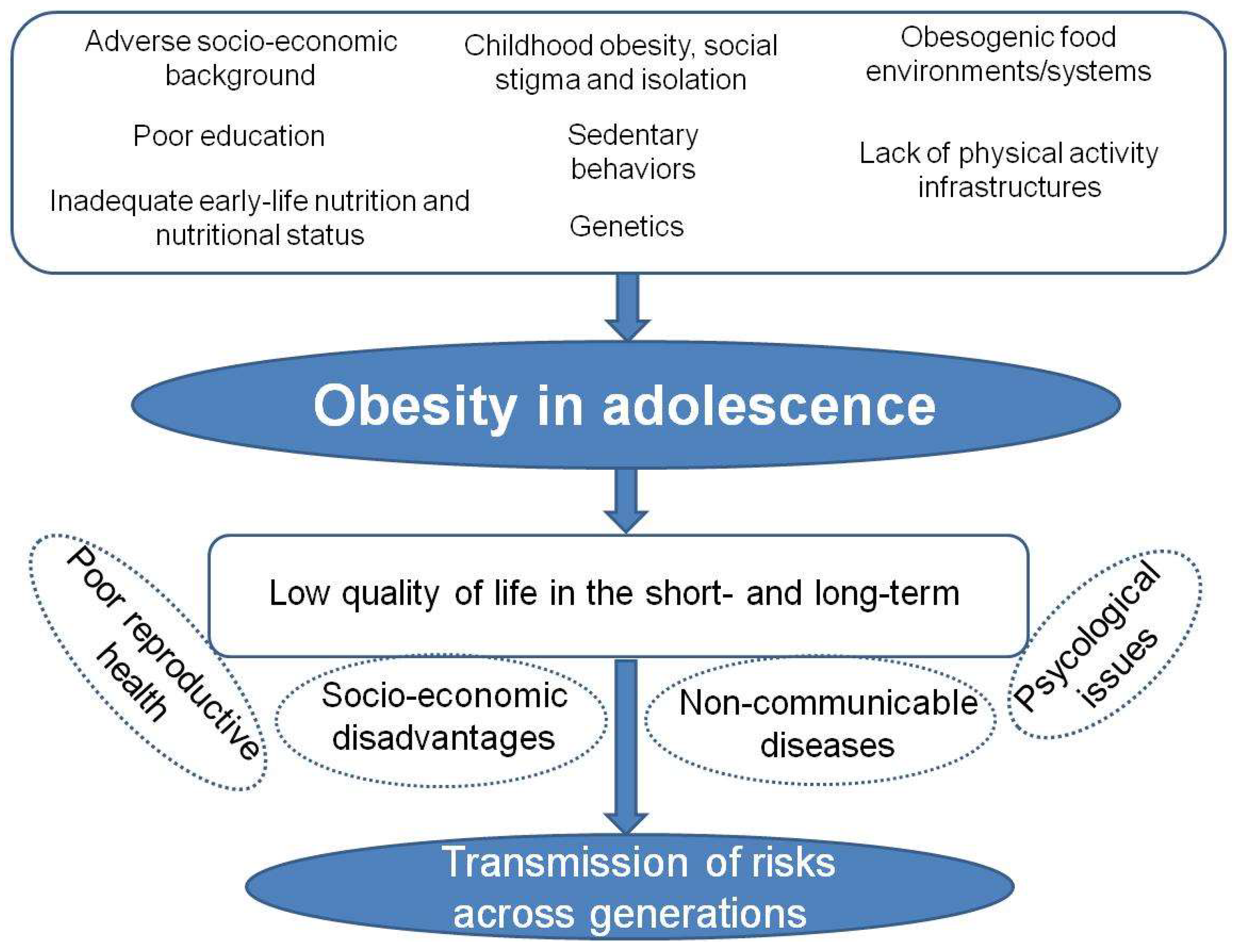
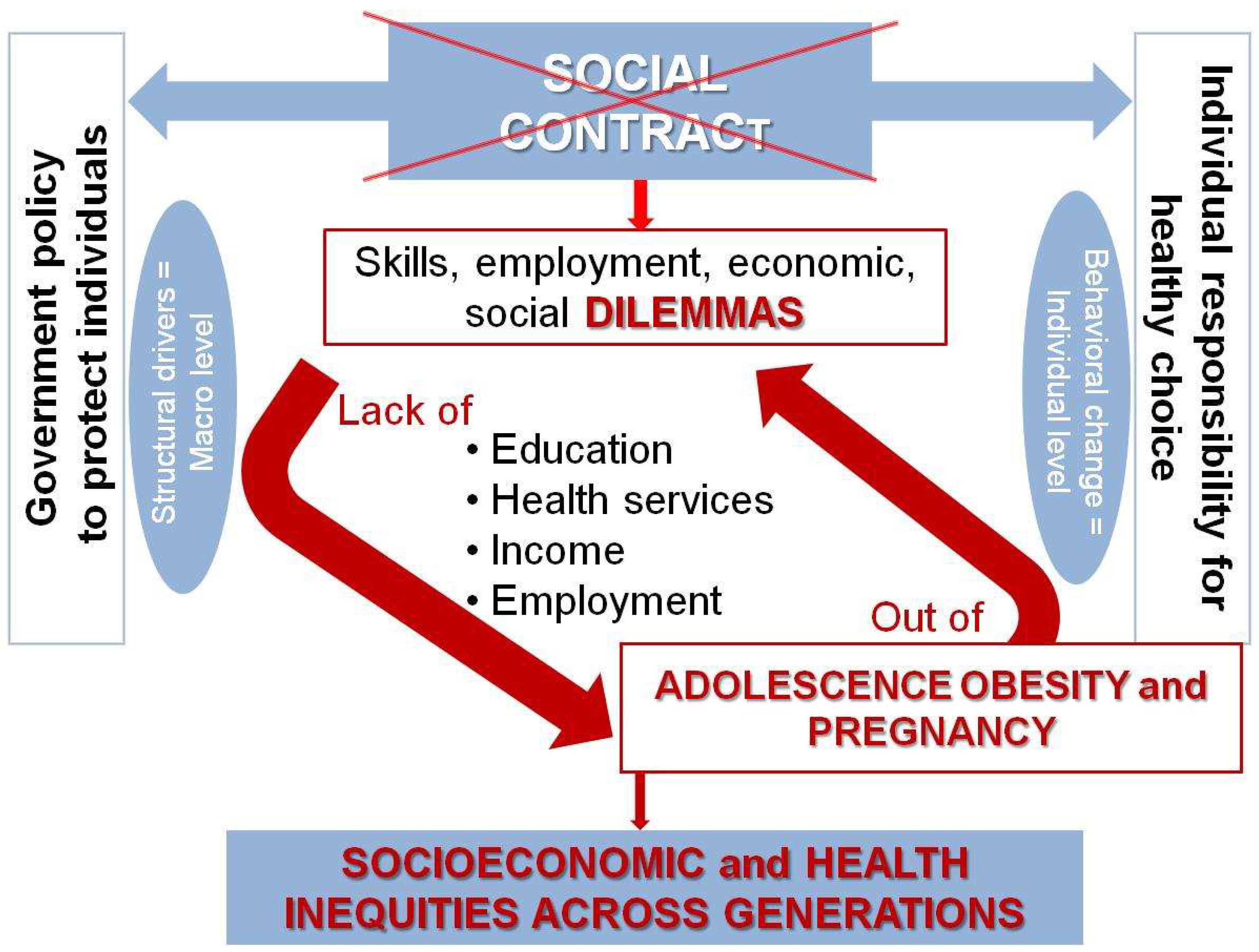
Adolescent health and well-being are of great concern worldwide, and adolescents encounter particular challenges, vulnerabilities and constraints. The dual challenges of adolescent parenthood and obesity are of public health relevance because of the life-altering health and socioeconomic effects on both the parents and the offspring. Prevention and treatment strategies at the individual and population levels have not been successful in the long term, suggesting that adolescent pregnancy and obesity cannot be managed by more of the same. Here, the researchers view adolescent obese pregnancy through the lens of the social contract with youth. The disruption of this contract is faced by today’s adolescents, with work, social and economic dilemmas which perpetuate socioeconomic and health inequities across generations. The lack of employment, education and social opportunities, together with obesogenic settings, increase vulnerability and exposure to lifelong health risks, affecting their offspring’s life chances too. To break such vicious circles of disadvantage and achieve sustainable solutions in real-world settings, strong efforts on the part of policymakers, healthcare providers and the community must be oriented towards guaranteeing equity and healthy nutrition and environments for today’s adolescents. The involvement of adolescents themselves in developing such programs is paramount, not only so that they feel a sense of agency but also to better meet their real life needs.
- adolescents
- obesity
- pregnancy
- parental obesity
- nutrition
- social context
1. Introduction
2. How the Dilemmas from the Broken Social Contract Drive the Problems of Adolescent Pregnancy and Obesity
3. Conclusions and Future Directions
References
- Norris, S.A.; Frongillo, E.A.; Black, M.M.; Dong, Y.; Fall, C.; Lampl, M.; Liese, A.D.; Naguib, M.; Prentice, A.; Rochat, T.; et al. Nutrition in adolescent growth and development. Lancet 2022, 399, 172–184.
- Ross, D.A.; Hinton, R.; Melles-Brewer, M.; Engel, D.; Zeck, W.; Fagan, L.; Herat, J.; Phaladi, G.; Imbago-Jácome, D.; Anyona, P.; et al. Adolescent Well-Being: A Definition and Conceptual Framework. J. Adolesc. Health 2020, 67, 472–476.
- Child Health Initiative. PMNCH, Plan international, UNFPA, UNICEF, WHO, UN Major Group for Children and Youth Adolescents 2030: A Call to Action for Adolescent Wellbeing 2019. Available online: https://www.adolescents2030.org/ (accessed on 21 November 2021).
- Al-Jawaldeh, A.; Bekele, H.; de Silva, A.; Gomes, F.; Untoro, J.; Wickramasinghe, K.; Williams, J.; Branca, F. A new global policy framework for adolescent nutrition? Lancet 2022, 399, 125–127.
- Azzopardi, P.S.; Hearps, S.J.C.; Francis, K.L.; Kennedy, E.C.; Mokdad, A.H.; Kassebaum, N.J.; Lim, S.; Irvine, C.M.S.; Vos, T.; Brown, A.D.; et al. Progress in adolescent health and wellbeing: Tracking 12 headline indicators for 195 countries and territories, 1990–2016. Lancet 2019, 393, 1101–1118.
- WHO, UNICEF, Plan International, International Association for Adolescent Health, Partnership for Maternal, Newborn & Child Health, Child Health Initiative, UN Major Group for Children and Youth, UNFPA Adolescent Health—The Missing Population in Universal Health Coverage 2019. Available online: https://pmnch.who.int/resources/publications/m/item/adolescent-health---the-missing-population-in-universal-health-coverage. (accessed on 21 November 2021).
- Patton, G.C.; Neufeld, L.M.; Dogra, S.; Frongillo, E.A.; Hargreaves, D.; He, S.; Mates, E.; Menon, P.; Naguib, M.; Norris, S.A. Nourishing our future: The Lancet Series on adolescent nutrition. Lancet 2022, 399, 123–125.
- Blüher, M. Obesity: Global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 2019, 15, 288–298.
- Simmonds, M.; Llewellyn, A.; Owen, C.G.; Woolacott, N. Predicting adult obesity from childhood obesity: A systematic review and meta-analysis: Adult obesity from childhood obesity. Obes. Rev. 2016, 17, 95–107.
- Catalán, V.; Avilés-Olmos, I.; Rodríguez, A.; Becerril, S.; Fernández-Formoso, J.A.; Kiortsis, D.; Portincasa, P.; Gómez-Ambrosi, J.; Frühbeck, G. Time to Consider the “Exposome Hypothesis” in the Development of the Obesity Pandemic. Nutrients 2022, 14, 1597.
- Reinehr, T. Long-term effects of adolescent obesity: Time to act. Nat. Rev. Endocrinol. 2018, 14, 183–188.
- Raffoul, A.; Williams, L. Integrating Health at Every Size principles into adolescent care. Curr. Opin. Pediatrics 2021, 33, 361–367.
- Nemiary, D.; Shim, R.; Mattox, G.; Holden, K. The Relationship Between Obesity and Depression Among Adolescents. Psychiatr. Ann. 2012, 42, 305–308.
- Walders-Abramson, N.; Nadeau, K.J.; Kelsey, M.M.; Schmiege, S.J.; Ellert, S.; Cejka, A.; Bhatnagar, K.; Zeitler, P. Psychological Functioning in Adolescents with Obesity Co-Morbidities. Child. Obes. 2013, 9, 319–325.
- Fox, C.K.; Gross, A.C.; Rudser, K.D.; Foy, A.M.H.; Kelly, A.S. Depression, Anxiety, and Severity of Obesity in Adolescents: Is Emotional Eating the Link? Clin. Pediatr. 2016, 55, 1120–1125.
- World Health Organization. Adolescent Pregnancy. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/adolescent-pregnancy (accessed on 5 December 2021).
- Patton, G.C.; Olsson, C.A.; Skirbekk, V.; Saffery, R.; Wlodek, M.E.; Azzopardi, P.S.; Stonawski, M.; Rasmussen, B.; Spry, E.; Francis, K.; et al. Adolescence and the next generation. Nature 2018, 554, 458–466.
- Fleming, N.; O’Driscoll, T.; Becker, G.; Spitzer, R.F.; Allen, L.; Millar, D.; Brain, P.; Dalziel, N.; Dubuc, E.; Hakim, J.; et al. Adolescent Pregnancy Guidelines. J. Obstet. Gynaecol. Can. 2015, 37, 740–756.
- Del Ciampo, L.A.; Del Ciampo, I.R.L. Physical and Emotional Repercussions of Pregnancy during Adolescence. Asian J. Pediatric Res. 2020, 4, 17–22.
- Macedo, T.C.C.; Montagna, E.; Trevisan, C.M.; Zaia, V.; de Oliveira, R.; Barbosa, C.P.; Laganà, A.S.; Bianco, B. Prevalence of preeclampsia and eclampsia in adolescent pregnancy: A systematic review and meta-analysis of 291,247 adolescents worldwide since 1969. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 248, 177–186.
- Fall, C.H.D.; Sachdev, H.S.; Osmond, C.; Restrepo-Mendez, M.C.; Victora, C.; Martorell, R.; Stein, A.D.; Sinha, S.; Tandon, N.; Adair, L.; et al. Association between maternal age at childbirth and child and adult outcomes in the offspring: A prospective study in five low-income and middle-income countries (COHORTS collaboration). Lancet Glob. Health 2015, 3, e366–e377.
- Karaçam, Z.; Kizilca Çakaloz, D.; Demir, R. The impact of adolescent pregnancy on maternal and infant health in Turkey: Systematic review and meta-analysis. J. Gynecol. Obstet. Hum. Reprod. 2021, 50, 102093.
- Sámano, R.; Chico-Barba, G.; Martínez-Rojano, H.; Hernández-Trejo, M.; Birch, M.; López-Vázquez, M.; García-López, G.E.; Díaz de León, J.; Mendoza-González, C.V. Factors Associated With Weight, Length, and BMI Change in Adolescents’ Offspring in Their First Year of Life. Front. Pediatr. 2021, 9, 709933.
- World Health Organization. Review of Social Determinants and the Health Divide in the WHO European Region: Final Report; Regional Office for Europe: Denmark Copenhagen, 2013; Available online: https://www.euro.who.int/en/publications/abstracts/review-of-social-determinants-and-the-health-divide-in-the-who-european-region.-final-report. (accessed on 5 December 2021).
- Clark, H.; Ghebreyesus, T.A.; Albrectsen, A.-B.; Alcocer, J.; Alden, E.; Azoulay, A.; Billingsley, S.; Blum, R.W.; Bhushan, R.; Byanyima, W.; et al. Uniting for adolescents in COVID-19 and beyond. BMJ 2021, 372, n719.
- Bhutta, Z.A.; Boerma, T.; Black, M.M.; Victora, C.G.; Kruk, M.E.; Black, R.E. Optimising child and adolescent health and development in the post-pandemic world. Lancet 2022, 399, 1759–1761.
- Buonsenso, D.; Roland, D.; De Rose, C.; Vásquez-Hoyos, P.; Ramly, B.; Chakakala-Chaziya, J.N.; Munro, A.; González-Dambrauskas, S. Schools Closures During the COVID-19 Pandemic: A Catastrophic Global Situation. Pediatric Infect. Dis. J. 2021, 40, e146–e150.
- Larki, M.; Sharifi, F.; Roudsari, R.L. Women’s Reproductive Health and Rights Through the Lens of the COVID-19 Pandemic. Sultan Qaboos Univ. Med. J. 2021, 21, e166–e171.
- Carducci, B.; Keats, E.C.; Ruel, M.; Haddad, L.; Osendarp, S.J.M.; Bhutta, Z.A. Food systems, diets and nutrition in the wake of COVID-19. Nat. Food 2021, 2, 68–70.
- Kumar, N.; Ramphul, K.; Gonzalez Mejias, S.; Lohana, P.; Verma, R.; Ramphul, Y.; Sonaye, R. The impact of COVID-19 lockdown on children and adolescents and possible solutions: A perspective. Arch. Med. Sci. Atheroscler. Dis. 2021, 6, 115–119.
- Stavridou, A.; Kapsali, E.; Panagouli, E.; Thirios, A.; Polychronis, K.; Bacopoulou, F.; Psaltopoulou, T.; Tsolia, M.; Sergentanis, T.N.; Tsitsika, A. Obesity in Children and Adolescents during COVID-19 Pandemic. Children 2021, 8, 135.
- Bowman, B.; Pickard, S. Peace, Protest and Precarity: Making Conceptual Sense of Young People’s Non-violent Dissent in a Period of Intersecting Crises. JAYS 2021, 4, 493–510.
- Romanello, M.; McGushin, A.; Di Napoli, C.; Drummond, P.; Hughes, N.; Jamart, L.; Kennard, H.; Lampard, P.; Solano Rodriguez, B.; Arnell, N.; et al. The 2021 report of the Lancet Countdown on health and climate change: Code red for a healthy future. Lancet 2021, 398, 1619–1662.
- Hickman, C.; Marks, E.; Pihkala, P.; Clayton, S.; Lewandowski, R.E.; Mayall, E.E.; Wray, B.; Mellor, C.; van Susteren, L. Climate anxiety in children and young people and their beliefs about government responses to climate change: A global survey. Lancet Planet. Health 2021, 5, e863–e873.
- Watts, N.; Amann, M.; Arnell, N.; Ayeb-Karlsson, S.; Belesova, K.; Boykoff, M.; Byass, P.; Cai, W.; Campbell-Lendrum, D.; Capstick, S.; et al. The 2019 report of The Lancet Countdown on health and climate change: Ensuring that the health of a child born today is not defined by a changing climate. Lancet 2019, 394, 1836–1878.
- Swinburn, B.A.; Kraak, V.I.; Allender, S.; Atkins, V.J.; Baker, P.I.; Bogard, J.R.; Brinsden, H.; Calvillo, A.; De Schutter, O.; Devarajan, R.; et al. The Global Syndemic of Obesity, Undernutrition, and Climate Change: The Lancet Commission report. Lancet 2019, 393, 791–846.
- Loewe, M.; Zintl, T.; Houdret, A. The social contract as a tool of analysis: Introduction to the special issue on “Framing the evolution of new social contracts in Middle Eastern and North African countries”. World Dev. 2021, 145, 104982.
- Low, F.M.; Gluckman, P.D.; Hanson, M.A. Maternal and child health: Is making ‘healthy choices’ an oxymoron? Glob Health Promot 2021, 28, 66–69.
- United Nations Population Fund. Motherhood in Childhood: Facing the Challenge of Adolescent Pregnancy: The State of World Population 2013; United Nations Population Fund: 2013. New York: 2013. Available online: https://www.unfpa.org/sites/default/files/pub-pdf/EN-SWOP2013.pdf (accessed on 5 December 2021).
- Bearak, J.; Popinchalk, A.; Ganatra, B.; Moller, A.-B.; Tunçalp, Ö.; Beavin, C.; Kwok, L.; Alkema, L. Unintended pregnancy and abortion by income, region, and the legal status of abortion: Estimates from a comprehensive model for 1990–2019. Lancet Glob. Health 2020, 8, e1152–e1161.
- Staatz, C.B.; Kelly, Y.; Lacey, R.E.; Hardy, R. Area-level and family-level socioeconomic position and body composition trajectories: Longitudinal analysis of the UK Millennium Cohort Study. Lancet Public Health 2021, 6, e598–e607.
- Dalrymple, K.V.; Vogel, C.; Godfrey, K.M.; Baird, J.; Harvey, N.C.; Hanson, M.A.; Cooper, C.; Inskip, H.M.; Crozier, S.R. Longitudinal dietary trajectories from preconception to mid-childhood in women and children in the Southampton Women’s Survey and their relation to offspring adiposity: A group-based trajectory modelling approach. Int. J. Obes. 2022, 46, 758–766.
- Tester, J.M.; Rosas, L.G.; Leung, C.W. Food Insecurity and Pediatric Obesity: A Double Whammy in the Era of COVID-19. Curr. Obes. Rep. 2020, 9, 442–450.
- Iguacel, I.; Gasch-Gallén, Á.; Ayala-Marín, A.M.; De Miguel-Etayo, P.; Moreno, L.A. Social vulnerabilities as risk factor of childhood obesity development and their role in prevention programs. Int. J. Obes. 2021, 45, 1–11.
- Kennedy, E.; Binder, G.; Humphries-Waa, K.; Tidhar, T.; Cini, K.; Comrie-Thomson, L.; Vaughan, C.; Francis, K.; Scott, N.; Wulan, N.; et al. Gender inequalities in health and wellbeing across the first two decades of life: An analysis of 40 low-income and middle-income countries in the Asia-Pacific region. Lancet Glob. Health 2020, 8, e1473–e1488.
- Meier Magistretti, C.; Reichlin, B. Salutogenesis and the Sense of Coherence in Young Adults Not in Education, Employment, or Training (NEET). In The Handbook of Salutogenesis; Mittelmark, M.B., Bauer, G.F., Vaandrager, L., Pelikan, J.M., Sagy, S., Eriksson, M., Lindström, B., Meier Magistretti, C., Eds.; Springer International Publishing: Cham, Switzerland, 2022; pp. 151–165. ISBN 978-3-030-79514-6. (accessed on 26 January 2022).
- Chandler, R.F.; Santos Lozada, A.R. Health status among NEET adolescents and young adults in the United States, 2016–2018. SSM—Popul. Health 2021, 14, 100814.
- Sun, X.; McHale, S.M.; Updegraff, K.A. Maternal and paternal resources across childhood and adolescence as predictors of young adult achievement. J. Vocat. Behav. 2017, 100, 111–123.
- Pinto e Silva, J.; Surita, F. Pregnancy in Adolescence—A Challenge Beyond Public Health Policies. Rev. Bras. Ginecol. Obs. 2017, 39, 041–043.
- Symeonaki, M.; Parsanoglou, D.; Stamatopoulou, G. The Evolution of Early Job Insecurity in Europe. SAGE Open 2019, 9, 215824401984518.
- Awad, A. From school to employment; the dilemma of youth in Sub–Saharan Africa. Int. J. Adolesc. Youth 2020, 25, 945–964.
- Eurofound. Impact of COVID-19 on Young People in EU. Publications Office of the European Unit, Luxemburg. 2021. Available online: https://www.eurofound.europa.eu/sites/default/files/ef_publication/field_ef_document/ef20036en.pdf. (accessed on 20 January 2022).
