Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Vivi Li and Version 1 by Bassam Odeh Al-Naami.
Sleep is crucial for human health from metabolic, mental, emotional, and social points of view; obtaining good sleep in terms of quality and duration is fundamental for maintaining a good life quality. Over the years, sSeveral systems have been proposed in the scientific literature and on the market to derive metrics used to quantify sleep quality as well as detect sleep disturbances and disorders. In this field, wearable systems have an important role in the discreet, accurate, and long-term detection of biophysical markers useful to determine sleep quality.
- sleep dysfunction
- sensors
- wearable devices
- EEG
- ECG
- EOG
- polysomnography
- sleep staging
1. Introduction
Sleep is a fundamental biological process for human life, as it plays a fundamental role in maintaining physical, psychological, emotional, and social health thanks to its restorative, regenerative, conservative, consolidating, and protective functions [1,2,3][1][2][3]. In fact, sleep’s poor quality or its insufficient duration can have both short- and long-term repercussions, such as a decrease in life’s quality, difficulty in concentrating, learning problems, bad mood, excessive daytime sleepiness, accidents of various types, weakening of the immune system, propensity to contract infections and diseases, etc. [4,5,6][4][5][6]. Numerous negative health impacts, such as an elevated risk of hypertension, diabetes, obesity, depression, heart attack, and stroke, have been associated with the cumulative long-term effects of sleep disturbances and sleep deprivation [7]. The most common sleep disorders, according to their prevalence, are the following: insomnia, sleep apnea, restless legs syndrome (RLS), hypersomnia, parasomnia, circadian rhythm disorders, obstructive sleep apnea, nocturnal, epilepsy, etc. [8,9,10,11][8][9][10][11]. Therefore, monitoring sleep and related disorders is crucial in preventing diseases [12,13,14][12][13][14].
Moreover, sleep health is a complex sleep-wakefulness pattern adaptable to individual, social, and environmental needs and supports physical and mental health [15]. Subjective satisfaction, optimal timing, adequate duration, high efficiency, and maintained attentiveness throughout waking hours are characteristics of healthy sleep. Thus, quantifying sleep health requires a set of measurable quantities related to physical, mental, and neurobehavioral well-being. These lasts can be classified into five dimensions: sleep duration, continuity, timing, alertness, sleepness, and satisfaction/quality. Some of them are based on subjective evaluation (e.g., satisfaction/quality); thus, sleep health can be quantified through subjective reports.
Wearable devices offer a valuable contribution in this area, as they allow collection, analysis, and transmission during sleep of vital and functional parameters, including body temperature, heart rate, respiratory rate, blood oxygen saturation, etc. [16,17,18,19,20,21][16][17][18][19][20][21]. Furthermore, these solutions are discreet and not bulky (contrary to the polysomnography exam, which remains the gold standard for recording electroencephalographic, respiratory, cardiac, and eye movements activities) and allow sleep monitoring even from home. Moreover, the recent spread of COVID-19 had a negative impact on sleep due to increased anxiety, insecurity, stress, fear, loneliness, depression, etc. These sleep alterations affect a wide portion of the global population, not only subjects who tested positive for this infection [22,23,24][22][23][24].
2. Importance of Sleep Monitoring
This section outlines an overview of sleep mechanisms and related disorders, stressing the importance of sleep monitoring to prevent such diseases [27,28,29][25][26][27]. Sleep is characterized scientifically by the individual behavior while asleep and the accompanying physiological changes occurring in the waking brain’s electrical cycles during sleep. A reduction or lack of mobility, slow eye movements, a distinctive sleeping body posture, lower reactivity to external stimuli, longer reaction time, heightened arousal threshold, diminished cognitive function, and unconscious but reversible state are the behavioral phenomena featuring sleep. Moreover, physiological changes may be measured using specific clinical tests involving the acquisition of several biosignals, such as EEG, EOG, EMG, or ECG. Sleep is classified into two main states: non-rapid eye movement (NREM) sleep, which is distinguished into three stages (i.e., N1, N2, N3), and rapid eye movement (REM) sleep. The first is defined by a gradual decrease in reactivity to stimulus, slow rolling eye movements, slightly reduced mobility, reversible unconscious state, and synchronized EEG characterized by slow-wave activity associated with spindles and K-complexes, as well as diminished muscular tone. The latter is characterized by fast eye movements, reduced reactivity to stimulus, muscular atonia, fast rhythms, and myoclonic jerks. In addition, other symptoms are desynchronized EEG featured by theta waves, periodic swings in blood pressure and heart rhythm, irregular respiration, phasic tongue movements, and may include a few episodes of apnea or hypopnea [27][25]. The two states alternate in a cyclic way (from 4 to 6 cycles during sleep, each lasting from 90 to 110 min, Figure 1). From 20% to 25% of total sleep duration in adults is spent in REM sleep, while the remaining 75–80% is spent in NREM sleep. In a healthy adult, there is a gradual progression from wakefulness to sleep onset, NREM sleep, and REM sleep [27][25]. Nevertheless, this trend is heavily affected by the nervous system’s maturation, changing from childhood to adulthood, as discussed in [27][25]. The hypothalamus’s suprachiasmatic nuclei master clock regulates the sleep-and-wake circadian rhythm. In addition, the neuroanatomical substrates of NREM sleep are primarily found in the ventrolateral preoptic nucleus of the hypothalamus, while those of REM sleep are found in the pons.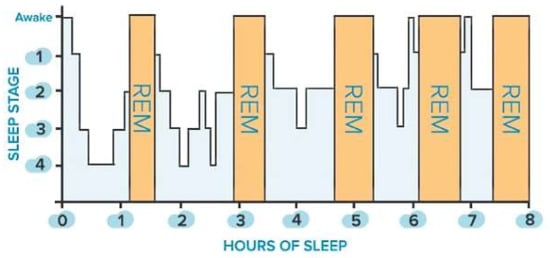
Figure 1.
Sleep stages of a healthy adult: non-rapid eye movement (NREM, blue bars) and rapid eye movement (REM, orange bars) stages.
3. Overview of Commercial Wearable Devices for Detecting Sleep Disorders
After introducing several wearable devices for sleep monitoring proposed in the scientific literature, this section will illustrate an overview of commercial devices on the market. The most popular devices put comfort ahead of precision. They are not well-adapted to monitor sleep disorders because they solely use heart rate, breathing, and body movement measures to determine sleep quality. In fact, these devices are aimed at healthy users, but they cannot be considered sufficiently reliable for diagnostic sleep disorders. In [49][36], Goldstein et al., presented a device called BrainBit, which can be placed on a user’s forehead to track sleep. The device has four EEG channels, with mechanisms for removing EMG and EOG signal components to monitor the electrical brain activity and bioelectricity of the forehead, face, head, and eye muscles [50][37]. The headband is composed of flexible and non-stretchable ribbon on which the golden dry electrodes, the battery, an integrated electronic board, and an elastic fabric band are placed, as shown in Figure 2.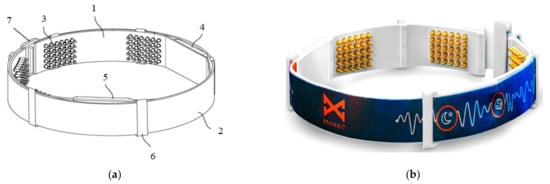
Figure 2.
Schematic (
a
) and real (
b) views of BrainBit (1: ribbon, 2: elastic band, 3: electrodes, 4: electronic module, 5: removable battery, 6: eyelet, 7: clasp) [49].
) views of BrainBit (1: ribbon, 2: elastic band, 3: electrodes, 4: electronic module, 5: removable battery, 6: eyelet, 7: clasp) [36].

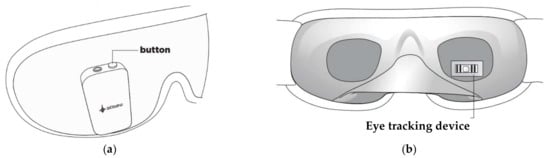
Figure 5.
External (
a
) and internal (
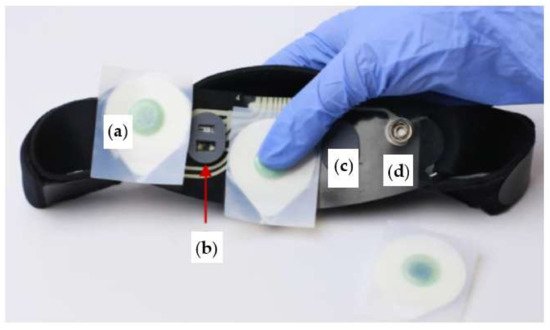
Figure 6.
Internal view of Sleep Profiler headband, consisting of EEG sensor (
a
), optical sensor (
b
), strip pad (
c
), and sensor snap (
Table 21. Comparison between the devices discussed above from the point of view of number and typology of the integrated sensors, gathered parameters, and cost.
| Device | Number of Parameters Detected | Integrated Sensors | Gathered Parameters |
Feedbacks/ Interventions |
Cost |
|---|---|---|---|---|---|
| BrainBit [50][37] |
4 | EEG, PPG, EMG, EOG | Brain activity, heart rate, body movement, eye movement |
Psychology and cognitive remediation | USD $499 |
| SmartSleep [67][54] |
1 | EEG | Brain activity | Audio tones to boost the slow wave | USD $399 |
| Muse S [53][40] |
4 | EEG, PPG, gyroscope, accelerometer | Brain activity, heart rate, breath rate, body movements |
Digital sleeping pills (sleep stories and meditation, ambient soundscape, nature and music biofeedbacks) | USD $399 |
| Dreem 2 [55][42] |
4 | EEG, PPG, gyroscope, accelerometer | Brain activity, heart rate, breath rate, body movement | CBT-I exercises | N.A. 1 |
| iBand+ [58][45] |
2 | EEG, accelerometer, gyroscope |
Brain activity, head movement |
Audio tones to induce sleep | USD $449 |
| Neuroon Open [59][46] |
4 | EEG, EOG, PPG, thermometer, |
Brain activity, eye movement, body temperature, blood oxygenation | Audio tones to induce sleep | N.A. 1 |
| Somni [60][47] |
2 | EOG, accelerometer | Eye movement, head movement | Audiovisual feedback to induce sleep | N.A. 1 |
| BrainLink Pro [61][48] |
4 | EEG, PPG, gyroscope thermometer, accelerometer, | Brain activity, heart rate, body temperature, head movement | No | USD $259 |
| Sleep Shepherd [62][49] |
2 | EEG, gyroscope, movement sensor | Brain activity head movement |
Binaural tones to induce sleep | N.A. 1 |
| Sleep Profiler [64][51] |
5 | EEG, EOG, EMG, accelerometer, ECG (optional), PPG (optional), nasal transducer (model SP29), pulse rate sensor (model SP29), oximeter (model SP29) | Brain activity, eye movement, head position, heart rate, quantitative snoring | No | N.A. 1 |
1 Not available.
References
- Worley, S.L. The Extraordinary Importance of Sleep. Pharm. Ther. 2018, 43, 758–763.
- Okano, K.; Kaczmarzyk, J.R.; Dave, N.; Gabrieli, J.D.E.; Grossman, J.C. Sleep Quality, Duration, and Consistency Are Associated with Better Academic Performance in College Students. NPJ Sci. Learn. 2019, 4, 16.
- Kapsi, S.; Katsantoni, S.; Drigas, A. The Role of Sleep and Impact on Brain and Learning. Int. J. Recent Contrib. Eng. Sci. IT (IJES) 2020, 8, 59–68.
- Garbarino, S.; Lanteri, P.; Bragazzi, N.L.; Magnavita, N.; Scoditti, E. Role of Sleep Deprivation in Immune-Related Disease Risk and Outcomes. Commun. Biol. 2021, 4, 1304.
- Gottlieb, D.J.; Ellenbogen, J.M.; Bianchi, M.T.; Czeisler, C.A. Sleep Deficiency and Motor Vehicle Crash Risk in the General Population: A Prospective Cohort Study. BMC Med. 2018, 16, 44.
- Peng, Z.; Dai, C.; Ba, Y.; Zhang, L.; Shao, Y.; Tian, J. Effect of Sleep Deprivation on the Working Memory-Related N2-P3 Components of the Event-Related Potential Waveform. Front. Neurosci. 2020, 14, 469.
- Institute of Medicine (US) Committee on Sleep Medicine and Research. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem; The National Academies Collection: Reports Funded by National Institutes of Health; Colten, H.R., Altevogt, B.M., Eds.; National Academies Press: Washington, DC, USA, 2006; ISBN 978-0-309-10111-0.
- Kales, A.; Soldatos, C.R.; Kales, J.D. Sleep Disorders: Insomnia, Sleepwalking, Night Terrors, Nightmares, and Enuresis. Ann. Intern. Med. 1987, 106, 582–592.
- Sack, R.L.; Auckley, D.; Auger, R.R.; Carskadon, M.A.; Wright, K.P., Jr.; Vitiello, M.V.; Zhdanova, I.V. Circadian Rhythm Sleep Disorders: Part I, Basic Principles, Shift Work and Jet Lag Disorders. Sleep 2007, 30, 1460–1483.
- Gigli, G.L.; Adorati, M.; Dolso, P.; Piani, A.; Valente, M.; Brotini, S.; Budai, R. Restless Legs Syndrome in End-Stage Renal Disease. Sleep Med. 2004, 5, 309–315.
- MedlinePlus. Sleep Disorders. Available online: https://medlineplus.gov/sleepdisorders.html (accessed on 15 July 2022).
- Kelly, J.M.; Strecker, R.E.; Bianchi, M.T. Recent Developments in Home Sleep-Monitoring Devices. ISRN Neurol 2012, 2012, 768794.
- Robbins, R.; Seixas, A.; Masters, L.W.; Chanko, N.; Diaby, F.; Vieira, D.; Jean-Louis, G. Sleep Tracking: A Systematic Review of the Research Using Commercially Available Technology. Curr. Sleep Med. Rep. 2019, 5, 156–163.
- Hussain, Z.; Sheng, Q.Z.; Zhang, W.E.; Ortiz, J.; Pouriyeh, S. A Review of the Non-Invasive Techniques for Monitoring Different Aspects of Sleep. ACM Trans. Comput. Healthc. 2022, 3, 24.
- Buysse, D.J. Sleep Health: Can We Define It? Does It Matter? Sleep 2014, 37, 9–17.
- De Fazio, R.; De Vittorio, M.; Visconti, P. A BLE-Connected Piezoresistive and Inertial Chest Band for Remote Monitoring of the Respiratory Activity by an Android Application: Hardware Design and Software Optimization. Future Internet 2022, 14, 183.
- De Fazio, R.; Al-Hinnawi, A.-R.; De Vittorio, M.; Visconti, P. An Energy-Autonomous Smart Shirt Employing Wearable Sensors for Users’ Safety and Protection in Hazardous Workplaces. Appl. Sci. 2022, 12, 2926.
- De Fazio, R.; Stabile, M.; De Vittorio, M.; Velázquez, R.; Visconti, P. An Overview of Wearable Piezoresistive and Inertial Sensors for Respiration Rate Monitoring. Electronics 2021, 10, 2178.
- Imtiaz, S.A. A Systematic Review of Sensing Technologies for Wearable Sleep Staging. Sensors 2021, 21, 1562.
- Schutte-Rodin, S.; Deak, M.C.; Khosla, S.; Goldstein, C.A.; Yurcheshen, M.; Chiang, A.; Gault, D.; Kern, J.; O’Hearn, D.; Ryals, S.; et al. Evaluating Consumer and Clinical Sleep Technologies: An American Academy of Sleep Medicine Update. J. Clin. Sleep Med. 2021, 17, 2275–2282.
- Chinoy, E.D.; Cuellar, J.A.; Jameson, J.T.; Markwald, R.R. Performance of Four Commercial Wearable Sleep-Tracking Devices Tested under Unrestricted Conditions at Home in Healthy Young Adults. Nat. Sci. Sleep 2022, 14, 493–516.
- Alimoradi, Z.; Broström, A.; Tsang, H.W.H.; Griffiths, M.D.; Haghayegh, S.; Ohayon, M.M.; Lin, C.-Y.; Pakpour, A.H. Sleep Problems during COVID-19 Pandemic and Its’ Association to Psychological Distress: A Systematic Review and Meta-Analysis. eClinicalMedicine 2021, 36, 100916.
- Lin, Y.N.; Liu, Z.R.; Li, S.Q.; Li, C.X.; Zhang, L.; Li, N.; Sun, X.W.; Li, H.P.; Zhou, J.P.; Li, Q.Y. Burden of Sleep Disturbance During COVID-19 Pandemic: A Systematic Review. Nat. Sci. Sleep 2021, 13, 933–966.
- Islam, M.K.; Molla, M.M.A.; Hasan, P.; Sharif, M.M.; Hossain, F.S.; Amin, M.R.; Rahman, M.R. Persistence of Sleep Disturbance among Post-COVID Patients: Findings from a 2-Month Follow-up Study in a Bangladeshi Cohort. J. Med. Virol. 2022, 94, 971–978.
- Chokroverty, S. Overview of Sleep & Sleep Disorders. Indian J. Med. Res. 2010, 131, 126–140.
- Thorpy, M.J. Classification of Sleep Disorders. Neurotherapeutics 2012, 9, 687–701.
- Surantha, N.; Kusuma, G.P.; Isa, S.M. Internet of Things for Sleep Quality Monitoring System: A Survey. In Proceedings of the 2016 11th International Conference on Knowledge, Information and Creativity Support Systems (KICSS), Yogyakarta, Indonesia, 10–11 November 2016; IEEE: Piscataway, NJ, USA, 2016; pp. 1–6.
- Wickboldt, A.T.; Bowen, A.F.; Kaye, A.J.; Kaye, A.M.; Bueno, F.R.; Kaye, A.D. Sleep Physiology, Abnormal States, and Therapeutic Interventions. Ochsner J. 2012, 12, 123–134.
- Chesson, A.L., Jr.; Ferber, R.A.; Fry, J.M.; Grigg-Damberger, M.; Hartse, K.M.; Hurwitz, T.D.; Johnson, S.; Kader, G.A.; Littner, M.; Rosen, G.; et al. The Indications for Polysomnography and Related Procedures. Sleep 1997, 20, 423–487.
- Dijk, D.-J.; Neri, D.F.; Wyatt, J.K.; Ronda, J.M.; Riel, E.; Ritz-De Cecco, A.; Hughes, R.J.; Elliott, A.R.; Prisk, G.K.; West, J.B.; et al. Sleep, Performance, Circadian Rhythms, and Light-Dark Cycles during Two Space Shuttle Flights. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 2001, 281, 1647–1664.
- Oh, C.-M.; Kim, H.Y.; Na, H.K.; Cho, K.H.; Chu, M.K. The Effect of Anxiety and Depression on Sleep Quality of Individuals with High Risk for Insomnia: A Population-Based Study. Front. Neurol. 2019, 10, 849.
- Silvani, A.; Dampney, R.A.L. Central Control of Cardiovascular Function during Sleep. Am. J. Physiol.-Heart Circ. Physiol. 2013, 305, H1683–H1692.
- Somers, V.K.; Dyken, M.E.; Mark, A.L.; Abboud, F.M. Sympathetic-Nerve Activity during Sleep in Normal Subjects. N. Engl. J. Med. 1993, 328, 303–307.
- Murali, N.S.; Svatikova, A.; Somers, V.K. Cardiovascular Physiology and Sleep. Front. Biosci. 2003, 8, s636–s652.
- Anusha, A.S.; Preejith, S.P.; Akl, T.J.; Sivaprakasam, M. Electrodermal Activity Based Autonomic Sleep Staging Using Wrist Wearable. Biomed. Signal Process. Control 2022, 75, 103562.
- Goldstein, B.; Sakharov, V.; Bulanov, S. Personal Apparatus for Conducting Electroencephalography. U.S. Patent WO2021183940A1, 13 March 2020.
- Brainbit. Brainbit Manual. Available online: http://brainbit.com/ (accessed on 3 March 2022).
- Lopez-Gordo, M.A.; Sanchez-Morillo, D.; Valle, F.P. Dry EEG Electrodes. Sensors 2014, 14, 12847–12870.
- Diep, C.; Garcia-Molina, G.; Jasko, J.; Manousakis, J.; Ostrowski, L.; White, D.; Anderson, C. Acoustic Enhancement of Slow Wave Sleep on Consecutive Nights Improves Alertness and Attention in Chronically Short Sleepers. Sleep Med. 2021, 81, 69–79.
- Muse™. Headband Manual. Available online: https://choosemuse.com/ (accessed on 3 March 2022).
- Western University, Canada. Assessing the Effects of the Muse Sleep Intervention on Sleep; Western University: London, ON, Canada, 2021. Available online: https://clinicaltrials.gov (accessed on 10 February 2022).
- Dreem|Sleep Pioneers. Available online: https://dreem.com/en/ (accessed on 3 March 2022).
- da Costa, T.D.; Vara, M.D.F.F.; Cristino, C.S.; Zanella, T.Z.; Neto, G.N.N.; Nohama, P. Breathing Monitoring and Pattern Recognition with Wearable Sensors; IntechOpen: London, UK, 2019; ISBN 978-1-78984-497-9.
- Arnal, P.J.; Thorey, V.; Debellemaniere, E.; Ballard, M.E.; Bou Hernandez, A.; Guillot, A.; Jourde, H.; Harris, M.; Guillard, M.; Van Beers, P.; et al. The Dreem Headband Compared to Polysomnography for Electroencephalographic Signal Acquisition and Sleep Staging. Sleep 2020, 43, zsaa097.
- IBand+ EEG Headband|Sleep Improvement & Lucid Dreaming Wearable Device. Available online: https://www.ibandplus.com/ (accessed on 4 March 2022).
- Neuroon Open: World’s Smartest Sleep Tracker. Available online: https://www.indiegogo.com/projects/2172509 (accessed on 4 March 2022).
- Somni Mask—The Easiest Way to Lucid Dreaming. Available online: https://somni.org/ (accessed on 14 March 2022).
- BrainLink by Macrotellect|Healthy Brainwaves for Everyone. Available online: http://www.macrotellect.com/ (accessed on 15 March 2022).
- Sleep Shepherd: Sleep Optimizer and Tracker. Available online: https://sleepshepherd.com/ (accessed on 14 March 2022).
- Kim, Y.; Moon, J.; Lee, H.-J.; Bae, C.-S.; Sohn, S. Integration of Electroencephalography Based Services into Consumer Electronics. In Proceedings of the 2012 IEEE 16th International Symposium on Consumer Electronics, Harrisburg, PA, USA, 4–6 June 2012; pp. 1–2.
- Sleep Profiler™ Specifications. Available online: https://www.advancedbrainmonitoring.com/products/sleep-profiler#section-specification (accessed on 14 March 2022).
- Levendowski, D.J.; Hamilton, G.S.; St. Louis, E.K.; Penzel, T.; Dawson, D.; Westbrook, P.R. A Comparison between Auto-Scored Apnea-Hypopnea Index and Oxygen Desaturation Index in the Characterization of Positional Obstructive Sleep Apnea. Nat. Sci. Sleep 2019, 11, 69–78.
- Levendowski, D.J.; Ferini-Strambi, L.; Gamaldo, C.; Cetel, M.; Rosenberg, R.; Westbrook, P.R. The Accuracy, Night-to-Night Variability, and Stability of Frontopolar Sleep Electroencephalography Biomarkers. J. Clin. Sleep Med. 2017, 13, 791–803.
- SmartSleep Deep Sleep Headband. Available online: https://www.usa.philips.com/c-e/smartsleep/deep-sleep-headband.html (accessed on 28 February 2022).
More

