Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Miguel-Angel Berciano-Guerrero and Version 2 by Catherine Yang.
Metastatic melanoma (MM) is a pathological entity with a very poor prognosis that had a low response rate to systemic treatments. In fact, the aggressiveness of melanoma is different depending on whether it debuts directly as metastatic disease or if what occurs is a relapse after a first diagnosis at an early stage, although the biological determinants are largely unknown. Another key aspect in the clinical management of metastatic melanoma at first diagnosis strives in the different prognosis of melanoma of unknown primary (MUP) compared to melanoma of known primary (MPK).
- metastatic melanoma
- first diagnosis
- MUP
1. Introduction
Previously, many efforts have been made to understand patterns of disease progression, providing information on risks that have helped improve monitoring and the efficacy of new adjuvant treatments [1][2][3][4][5][4,5,6,7,8]. More recently, additional studies are aiming to improve not only survival in the initial stages, with better diagnosis and adjuvant therapies that are more effective, but also the treatment of unresectable or metastatic disease, regardless of the initial stage at diagnosis. The arrival of immune checkpoint inhibitors (ICI) and targeted therapy (TT) with BRAF inhibitors/MEK inhibitors (BRAFi/MEKi) has triggered a paradigm shift, facilitating a better understanding of the molecular biology of these tumors. Melanoma is, to date, the most immunogenic tumor [6][9]. The high rate of neoantigens allows the tumor cells to respond better to therapies that act on the immune system and the tumor microenvironment (TME). Moreover, the immunological perturbation induced by ICI could influence the response to other subsequent therapies, suggested by better outcomes of TT after ICI [7][10]. However, more studies are needed to confirm this strategy.
2. Epidemiology of MM at First Diagnosis
Melanoma is a tumor with a low incidence rate, but high mortality. For 2022, the estimated number of new cases of melanoma in situ or invasive in the United States is 97,920 and 99,780, respectively, with an estimated number of deaths of 7650 patients. This indicates an annual decrease of 4%, due to recent improvements in treatments in both adjuvant and advanced disease treatments [8][11]. This trend can be observed in other countries in the world. Survival rates according to initial disease stage have been extensively described in large cohorts of patients [9][10][11][12][12,13,14,15], and the loss of efficacy towards advanced stages is a consolidated event (Table 1).Table 1.
Studies reporting data on metastatic melanoma at initial diagnosis.
4.2. Immunotherapy
The data from the pivotal studies with approved immunotherapeutic drugs that constitute the first line of treatment for metastatic melanoma are presented in Table 23.Table 23. Main pivotal studies of currently approved immunotherapy for metastatic melanoma.
Main pivotal studies of currently approved immunotherapy for metastatic melanoma.
| Clinical Trial | CHECKMATE-066 [29][30][31][39,40,41] | KEYNOTE-006 [32][33][42,43] | CHECKMATE-067 [34][35][44,45] | ||||
|---|---|---|---|---|---|---|---|
| All patients (n%) | 78 (9.6) | 810 (100) | 1191 (26.7) | ||||
| Experimental Drug | Nivo | 4459 | |||||
| Pem | Nivo-Ipi | Stage | Stage IV | Stage 0-IV | Stage IV | III-IV/Recurrence | |
| Control Drug | DTIC | Mean age (years) | 60.69 | 58.74 | 66 | 64.4 | |
| Ipi | Ipi/Nivo | ||||||
| Stage at randomization a,b (%) | Sex [n (%)] | ||||||
| III | NR | ||||||
| 3.1 | Men | 45 (9.3) | 485 (59.9) | - | |||
| IV (M1c) | 61% M1c | - | |||||
| 96.9 (66.2) | (58.9) | Women | 33 (10.2) | 325(40.1) | - | ||
| Stage IV at first diagnosis a,b | NR | - | |||||
| c | NR | NR | ECOG (%) | ||||
| mPFS a | 5.1 | 8.4 | 11.5 | 0–1 | |||
| mOS | 665 (55.8) | 2619 (58.7) | |||||
| a | 37.3 | 31.1 | 60.0 | 2 | 96 (8.1) | 248 (5.5) | |
| mOS by stage a,b: III M1a M1b M1c |
NR | NR | NR | 3–4 | 44 (3.7) | 91 (2.0) | |
| MUP patients | Mean time to recurrence (years) | 3.84 ± 5.19 | 4.94 ± 6.69 | ||||
| Included | |||||||
| Yes | Yes | Yes | Mutation type [n (%)] | ||||
| Outcomes | NR | NR | BRAF | 11 (21.6) | 51 (6.3) | 444 (37.3) | 1314 (42) |
| CKIT | 1 (16.7) | 6 (0.7) | - | - | |||
| NRAS | 0 | 1 (0.1) | - | - | |||
| MEK | 0 | 0 | - | - | |||
| GNAO | 0 | 0 | - | - | |||
| GNA11 | 0 | 0 | - | - | |||
| Metastatic [n (%)] | |||||||
| Yes | 11 (21.6) | 354 (44.0) | |||||
| No | 1 (16.7) | 454 (56.1) | |||||
| Resectable [n (%)] | |||||||
| Yes | 0 | 704 (86.9) | |||||
| No | 78 (73.6) | 106 (13.1) | |||||
| NR | Developed metastatic during course of disease | ||||||
| No | 78 (100) | 454 (56.0) | |||||
| Yes | 0 | 346 (42.7) | |||||
| Median Overall Survival [months (95% CI)] | |||||||
| Initially stage 0–II | 111.3 | ||||||
| Initially stage III | (95.6–131) | ||||||
| Initially stage IV | 76.3 (59.3–93.3) | ||||||
| 59.9 (38.2–81.7) | |||||||
| First Line Treatment (%) | |||||||
| Immunotherapy | 665 (73.1) | 1652 (73.5) | |||||
| BRAF inhibitor | 186 (20.4) | 393 (17.5) | |||||
| Clinical trial | 28 (3.1) | 106 (4.7) | |||||
| Chemotherapy | 19 (2.1) | 51 (2.3) | |||||
| Interferon | 5 (0.5) | 14 (0.6) | |||||
| IL-2 | 1 (0.1) | 4 (0.2) |
a TNM Classification according to the 7th edition.
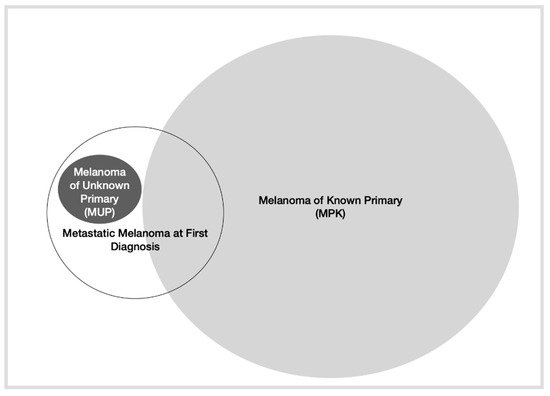
Figure 1.
Depiction of different types of presentation of metastatic melanoma.
3. Molecular Characterization of MM at First Diagnosis
In recent years, melanoma has been extensively characterized on a molecular basis in several studies. In fact, the latest World Health Organization (WHO) classification establishes nine categories of different melanoma subtypes, depending on the different driver mutations presented [23][26]. However, in routine practice, the most common mutations that have an approved therapeutic target (BRAF/MEK inhibition) are BRAF mutations, with other mutations that exceptionally require different treatment (NTRK fusions, etc.). Currently, efforts are being made to identify markers of efficacy and resistance to targeted therapy in metastatic melanoma [24][27]. The molecular characterization of patients with metastasis at presentation is not clear, nor is that of patients that present with MUP [25][28]. A recent article based on the nationwide Flatiron Health electronic database describes the frequency of BRAF mutations and the use of different therapeutic strategies depending on several factors, such as the stage at initial diagnosis [14][17]. Of the 4459 patients, 1191 had been diagnosed with stage IV at diagnosis, representing 26.7% of the total number of patients analyzed. These patients were diagnosed at a mean age of 66 years, presenting a good general condition (ECOG 0–1) and patterns of use of different systemic treatments similar to the general population (see Table 1). The only difference reported in this study is more frequent treatment with BRAF inhibitors in those patients who had a BRAF mutation and were initially diagnosed as stage IV, although these differences may be due to the high rate of patients excluded from the study. Additionally, the different patterns of use of treatments depending on the year can explain these differences. Therefore, the molecular characterization of patients with metastasis at the first diagnosis is not clearly defined. With these data, it would be difficult to explain whether patients presenting with stage IV at initial diagnosis have a cancer biology that is different from those diagnosed in earlier stages.4. Representation of MM at First Diagnosis in Pivotal Studies
To search for epidemiological data on how patients respond to different treatments depending on the initial stage at diagnosis, the rwesearchers reviewed published clinical trial information, as well as complementary material.4.1. Targeted Therapy
Currently, there are several studies that establish BRAF-targeted therapy as standard treatment for patients with metastatic melanoma who carry a BRAF mutation. The combinations vemurafenib-cobimetinib, dabrafenib-trametinib and encorafenib-binimetinib constitute the first line of treatment for patients with BRAF-mutated metastatic melanoma. The experience and knowledge accumulated over the last few years have elucidated that BRAF-mutated melanoma is a more aggressive tumor than BRAF wild-type melanoma, with greater growth rate and a greater capacity for metastasizing [a In experimental arm; b TNM Classification according to 7th edition; c At least 15.2% received adjuvant treatment; NR: Not reported; Nivo: nivolumab, DTIC: dacarbazine, Pem: pembrolizumab, Ipi: ipilimumab.
Information on patients diagnosed with stage IV at debut is not reported in any of the studies. Other similar clinical trials and their updates did not specify this subpopulation in their study population either [13][36][37][38][39][16,46,47,48,49].
Theoretically, it seems reasonable that immunotherapy may play an essential role in for the treatment of patients with MUP, given the implication of immunological mechanisms. However, there is no information regarding the MUP population reported in these studies.
In addition, therapeutic strategies that combine immunotherapy with several other drugs are currently being developed. However, none of the new combinations such as pembrolizumab with lenvatinib in the LEAP-004 study [40][50], bempegleukin and nivolumab in the PIVOT-02 study [41][51] or, more recently, nivolumab and relatlimab in the RELATIVITY-047 study [42][52] reported data on this subgroup of patients.
Similar to the targeted therapy studies, MUP patients were included in the trials with approved immunotherapy, but specific outcomes were not shown (Table 23).
