Brucellosis caused by Brucella spp. is transmitted by direct or indirect contact with infected animals or their secretions and through the consumption of infected animal meat and unpasteurized milk/milk products. Brucellosis is classified as one of the top neglected zoonosis by the World Health Organization (WHO), and despite this, it does not attract the appropriate attention it requires from both the Federal and State ministries of health in Nigeria. 15.8% (7178/45,363) seroprevalence of brucellosis was recorded in northern Nigeria as against 8.7% (1902/21,740) iCurrently, there is a lack of coordinated national data on the southern part. Brucella abortus, B. melitensis, B. suis, and B. canis were reported in 27 of the 36 stateprevalence and distribution of human and animal brucellosis.
- human and animal brucellosis
- Brucella
- Nigeria
- prevalence and seroprevalence
- systemic review and meta-analysis
1. Introduction
2. Human and AnDimal Brucellosis iscussion Nigeria
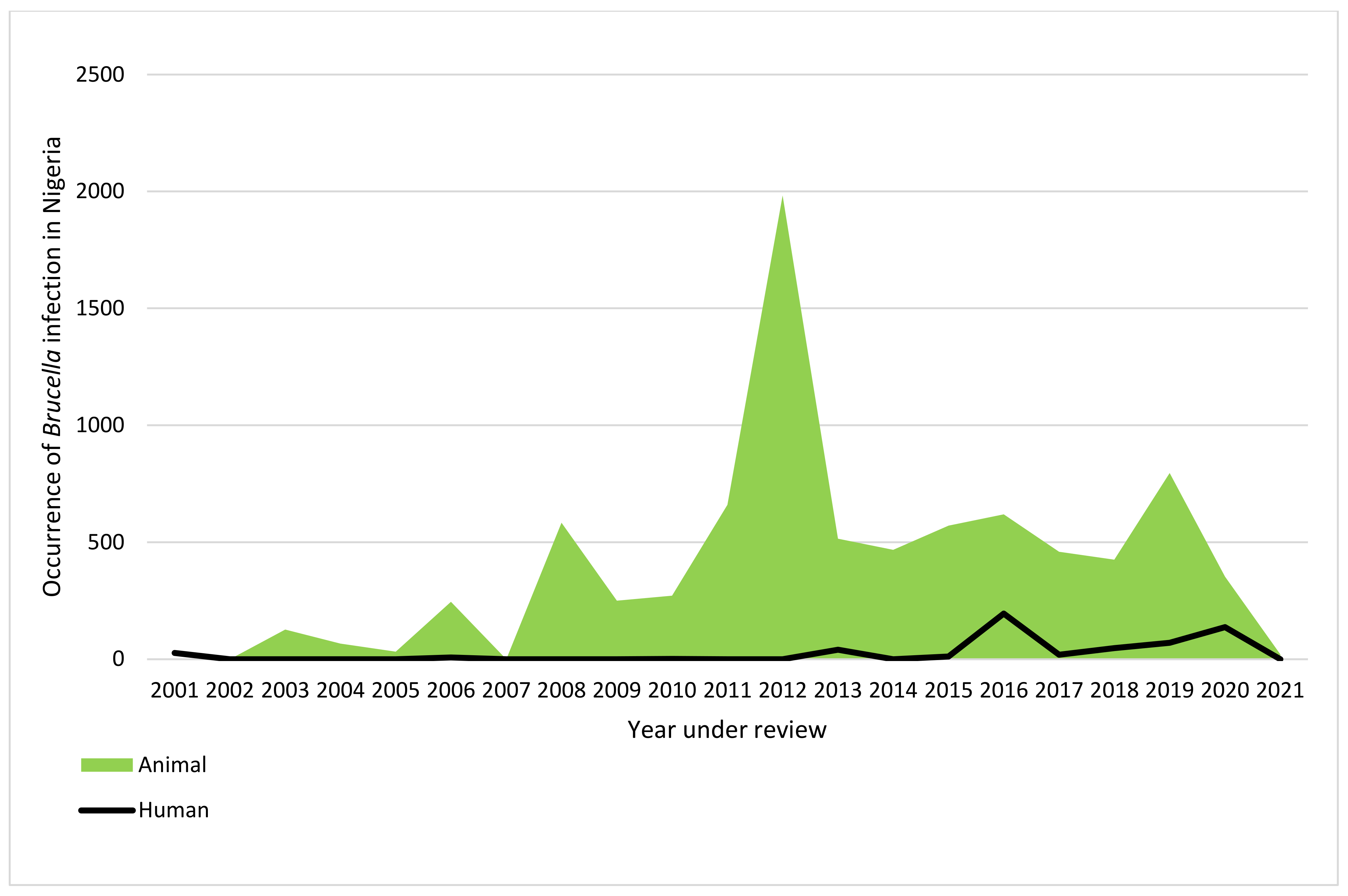
The economic burden in the livestock industry arising from brucellosis and its morbidity in humans has made this zoonotic disease a global public health challenge [14][111]. The main objective of this enstrudy was to systematically review the literature reporting brucellosis and perform a meta-analysis to estimate the national prevalence of brucellosis in Nigeria. To the best of our knowledge, this is the first exhaustive systemic review on human and animal brucellosis in Nigeria. Of the 99 publications accessed, 14 publications reported Brucella infection in humans from 11 states of the 36 states in Nigeria, including the federal capital territory. The remaining 25 states either do not have reports because of the lack of interest in brucellosis, or the reported cases do not meet the inclusion criteria of this revientryw. Most of the studies on human brucellosis were from high-risk occupational groups, especially abattoir workers. The national prevalence of human brucellosis in Nigeria for all methods revealed in this entryreview was 17.6%. However, based on the Rose Bengal plate test (RBPT), as reported by about 80% of the publications accessed for human brucellosis, the seroprevalence of the disease in Nigeria was 15.7% (493/3144). This is similar to the 15.8% recorded in Cameroon [15][112], but lower when compared to the sub-national study in other sub-Saharan African countries, such as the 44% prevalence recorded in Kenya [16][113], 31.5% prevalence in Ethiopia [17][114] and 17% in Uganda [18][115]. Similarly, the prevalence of human brucellosis is also higher in northern African countries such as Egypt, with a prevalence of 23.9% [19][116]. The prevalence is higher in Nigeria compared to the prevalence of 1.41% reported in Tanzania [20][117] and the 3.0% national prevalence in Kenya [21][118]. The high prevalence of human brucellosis from this rentryview has demonstrated the fact that brucellosis is endemic with a high burden in Nigeria and requires the attention of policymakers and stakeholders in the health sector. The high burden of human brucellosis in Nigeria, as seen in this entrstudy, can be attributed to several factors, which include nomadic pastoralists who run open grazing, abattoir workers, especially those slaughtering animals who are in constant contact with animal blood without personal protective equipment (PPE) (Figure 16), and the love of Nigerians for the consumption of animals’ intestinal parts, which are the most likely source of zoonotic transmission of the disease in Nigeria. Unfortunately, the animals that are ready for slaughter in Nigeria’s abattoirs are sometimes not screened for brucellosis. The spectrum of clinical presentation of human brucellosis, which mimics several other febrile illnesses such as rheumatic fever, typhoid, and malaria, has resulted in several misdiagnoses of this disease since malaria and typhoid fever are also endemic in Nigeria. Additionally, brucellosis is not routinely screened in private and public health care facilities, which obscures the detection and true prevalence of the disease.
Limitations: ReseaOurchers' inability to determine the prevalence of the disease based on certain variables such as age, sex, cattle herds, breeds of animals, and mortality rate both in humans and animals are part of the limitations of this entryreview. The use of serological methods, as seen in this entryreview, is of national importance because of their usefulness in detecting antibodies against Brucella species. However, the results are only reliable when the diagnostic methods and procedures are properly conducted and the outcomes are well interpreted. Interestingly, serological methods have several shortcomings, including the antisera’s ability to cross-react with other bacterial pathogens such as Escherichia coli 0157, Salmonella Urbana group N, Francisella tularensis, and Yersinia enterocolitica 0:9 [130].
Conclusions: This systentry mic review revealed a national prevalence of 19.2% of human Brucella infection and 13.1% prevalence of Brucella infection in common domestic animals, respectively, from 2001 to 2021. This enstrudy also indicated that only 27 states, including the FCT, reported brucellosis in Nigeria across the six geopolitical zones. Researchers'Our study also revealed the highest occurrence of brucellosis is in Northern Nigeria. Four Brucella species, B. abortus, B. melitensis, B. suis, and B. canis, have been reported in Nigeria. Culture and molecular methods of detection of brucellosis and reports of antimicrobial susceptibility testing remain a conjecture. This rentryview will help researchers redirect their research focus and serve as a guide for policymakers on measures for managing brucellosis in Nigeria and other sub-Saharan countries.The need for improved sanitary conditions of the abattoirs, the use of personal protective equipment by animal handlers, vaccination of animals against bovine brucellosis, and ranching of animals to curb the spread of the disease should be paramount to all the stakeholders.
Table S1:
Published report on human and animal brucellosis in Nigeria (2001–2021) arranged according to zone, state, authors, year of study, type of samples, number of samples, number of positive samples, the methods used and identified Brucella spp.
- Brucellosis in Humans and Animals; World Health Organization: Geneva, Switzerland, 2006.
- Ducrotoya, M.; Bertub, W.J.; Matopec, G.; Cadmusd, S.; Conde-Álvareze, R.; Gusib, A.M.; Welburna, S.; Ocholib, R.; Blascof, J.M.; et al. Brucellosis in Sub-Saharan Africa: Current challenges for management, diagnosis and control. Acta Tropica. 2017, 165, 179–193.
- Bennett, N.J.; Bronze, M.S. Brucellosis. Emedicine Medscape 2021; pp. 1–33. Available online: https://emedicine.medscape.com/article/213430-print Accessed April, 2022
- World Health Organization. Home/Newsroom/Fact sheets/Detail/Brucellosis; World Health Organization:Geneva, Switzerland, 2020.
- Rossetti, C.A.; Arenas-Gamboa, A.M.; Maurizio, E. Caprine brucellosis: A historically neglected disease with significant impact on public health. PLOS Negl. Trop. Dis. 2017, 11, e0005692. https://doi.org/10.1371/journal.pntd.0005692.
- Bosilkovski, M.; Keramat, F.; Arapovic, J. The current therapeutic strategies in human brucellosis. Infection 2021, 49, 823–832. https//doi.org/10.1007/s15010-921-01586-w.
- Cadmus, S.I.; Akporube, K.A.; Ola-Daniel, F.; Adelakun, O.D.; Akinseye, V.O. Seroprevalence and associated factors of brucellosis and Q-fever in cattle from Ibarapa area, Oyo state, south-western Nigeria. Pan Afr. Med. J. 2020, 36, 370. https://doi.org/10.11604/pamj.2020.36.370.24925.
- Wareth, G.; Dadar, M.; Ali, H.; Hamdy, M.E.R.; Al‐Talhy, A.M.; Elkharsawi, A.R.; El Tawab, A.A.A.; Neubauer, H. The perspective of antibiotic therapeutic challenges of brucellosis in the Middle East and North African countries: Current situation and therapeutic management. Emerg. Dis. 2022, 1, 1–16. https://doi.org/10.1111/tbed.14502.
- El-Diasty, M.; El-Said, R.; Abdelkhalek, A. Seroprevalence and molecular diagnosis of sheep brucellosis in Dakahlia governorate, Egypt. J. Vet. Res. 2021, 1, 34–39. https://doi.org/10.51585/gjvr.2021.0006.
- McDermott, J.J.; Arimi, S. Brucellosis in sub-Saharan Africa: epidemiology, control and impact. Microbiol. 2002, 90, 111–134. https://doi.org/10.1016/s0378-1135(02)00249-3.
- United Nations, Department of Economic and Social Affairs, Population Division. World Population Prospects 2019: Highlights; ST/ESA/SER.A/423; United Nations:
- Adamu, N.N.; Ajogi, I. Serological investigations of camels (Camelus dromedarius) slaughtered at Kano municipal abattoir for evidence of brucellosis. Vet. 1999, 18, 45–48.
- Ducrotoy, M.J.; Bertu, W.J.; Ocholi, R.A.; Gusi, A.M.; Bryssinckx, W.; Welburn, S.; Moriyón, I. Brucellosis as an Emerging Threat in Developing Economies: Lessons from Nigeria. PLoS Negl. Trop. Dis. 2014, 8, e3008. https://doi.org/10.1371/journal.pntd.0003008.
- Aworh, M.K.; Okolocha, E.C.; Awosanya, E.J.; Fasina, F.O. Sero-prevalence and intrinsic factors associated with Brucella infection in food animals slaughtered at abattoirs in Abuja, Nigeria. BMC Res. Notes 2017, 10, 499. https://doi.org/10.1186/s13104-017-2827-y.
- Ogugua, A.; Akinseye, V.; Ayoola, M.; Oyesola, O.; Shima, F.; Tijjani, A.; Musa, A.N.A.; Adesokan, H.; Perrett, L.; Taylor, A.; et al. Seroprevalence and risk factors of brucellosis in goats in selected states in Nigeria and the public health implications. J. Med. Med Sci. 2014, 43 (Suppl. 1), 121–129.
- Ehizibolo, D.O.; Gusi, A.M.; Ehizibolo, P.O.; Mbuk, E.U.; Ocholi, R.A. Serologic Prevalence of Brucellosis in Horse Stables in Two Northern States of Nigeria. Equine Sci. 2011, 22, 17–19. https://doi.org/10.1294/jes.22.17.
- Alhaji, N.B.; Wungak, Y.S.; Bertu, W.J.; Serological survey of bovine brucellosis in Fulani nomadic cattle breeds (Bos indicus) of North-central Nigeria: Potential risk factors and zoonotic implications. Acta Trop. 2016, 153: 28-35. doi: 10.1016/j.actatropica.2015.10.003. Epub 2015 Oct 14. PMID: 26464048.
- Bertu, W.J.; Ajogi, I.; Bale, J.O.O.; Kwaga, J.K.P.; Ocholi, R.A. Sero-epidemiology of brucellosis in small ruminants in Plateau State, Nigeria. J. Microbiol. Res. 2010, 4, 1935–1938.
- Bamidele, F.; Gidado, S.; Edukugho, A.; Cadmus, S. Seroprevalence of Brucellosis in abattoir workers and slaughtered cattle in Ilorin metropolis Kwara State Nigeria. J. Infect. Dis. 2020, 101, 532–533. https://doi.org/10.1016/j.ijid.2020.09.1379.
- Baba, A.Y.; Ameen, S.A.; Ambali, H.M.; Adah, A.D.; Abdulmajeed, I.; Furo, N.A.; Kadir, R.A.; Olajide, E.O. Seroprevalence of brucellosis in horses in Ilorin metropolis, Kwara State, Nigeria. Vet. Biomed. Sci. 2019, 2, 210–217.
- Bertu, W.; Ocholi, R.; Gusi, A.; Ngulukun, S.; Ducrotoy, M.; Moriyon, I. Isolation of brucella strains in cattle from sedentary and nomadic communities and its public health implication. J. Infect. Dis. 2020, 101, 533. https://doi.org/10.1016/j.ijid.2020.09.1380.
- Ndumari, W.; Se-ember, A.D.; Oluwatosin, A.; Terzugwe, T. Seroprevalence of Brucellosis in Nigerian Breed of Dog in North Bank Area of Makurdi, Benue State Nigeria. J. Intern. Med. Geriatr. 2020, 2, 80–86.
- Bertu, W.J.; Dapar, M.; Gusi, A.M.; Ngulukun, S.S.; Leo, S.; Jw, L.D. 2010. Prevalence of Brucella antibodies in marketed milk in Jos and environs. J. Food. Sci. 2010, 4, 62–64.
- Wungak, Y.S.; Aworh, M.K.F.; Maurice, N.; Balami, A.G.; Danmarwa, A.; Danthe, H.D. Serological survey of antibodies against Brucella abortus in cattle in Jos south local government area. J. Vet. Sci. 2011, 8, 39–43.
- Momoh, H.A.; Ijale, G.O.; Ajogi, I.; Okolocha, E.C. Risk factors and level of awareness of canine brucellosis in Jos, Plateau State, Nigeria. Vet. Med. Anim. Health 2015, 7, 39–44.
- Agada, C.A.; Goden, C.P.; Ogugua, J.O. Prevalence of bovine brucellosis and analysis of risk factors in resident cattle herds of Kanke Local Government Area, Plateau State, Nigeria. Vet. J. 2017, 38, 104–116.
- Dawang, N.D.; Danahap, L.S.; Nash, K.N.; Oluseye, E.; Kalejaye, O. Occurrence of Brucella spp in slaughtered sheep and goats in Jos main abattoir, Jos, Plateau State, Nigeria. J. Nat. Sci. AJNS 2016, 17, 1119–1104.
- Alhaji, N.B.; Wungak, Y. Epizootiological survey of bovine brucellosis in nomadic pastoral camps in Niger state, Nigeria. Vet. J. 2013, 34, 795–800.
- Agada, C.; Ogugua, A.; Anzaku, E. Occurrence of brucellosis in small ruminants slaughtered in Lafia central abattoir, Nasarawa State, Nigeria. Sokoto J. Vet. Sci. 2018, 16, 16–23. https://doi.org/10.4314/sokjvs.v16i1.3.
- Aworh, M.; Okolocha, E.; Kwaga, J.; Fasina, F.; Lazarus, D.; Suleman, I.; Poggensee, G.; Nguku, P.; Nsubuga, P. Human brucellosis: seroprevalence and associated exposure factors among abattoir workers in Abuja, Nigeria—2011. Pan Afr. Med. J. 2013, 16, 103. https://doi.org/10.11604/pamj.2013.16.103.2143.
- Agada, C.; Mohammed, J.; Okoh, A.E.J.; Ogugua, J.A. Prevalence and risk factors associated with brucellosis among high-risk individuals in Lafia, Nasarawa state, Nigeria. J. One Health 2018, 4, 45–51. https://doi.org/10.14202/ijoh.2018.45-51.
- Ngbede, E.O.; Momoh, A.H.; Bala, R.S.; Madaki, B.D.; Maurice, N.A. An abattoir-based study on sero-diagnosis of swine brucellosis in Makurdi, Benue State, North-Central Nigeria. Adv. Vet. Res. 2013, 3, 57–59.
- Bertu, W.J.; Ocholi, R.A.; Gusi, A.M.; Abdullahi, S.; Zwandor, N.J.; Durbi, I.A.A.; Opara, J.; Okewole, P.A. Brucella abortus infection in a multispecies livestock farm in Nigeria. J. Biotec. Food Sci. 2015, 3, 36–40.
- Ior, D.D.; Chukwu, C.C. Prevalence of Brucella antibodies in marketed cow milk in Benue State, Nigeria. J. Microbiol. Res. 2015, 9, 1752–1757.
- Cadmus, S.; Adesokan, H.; Oluwayelu, D.; Idris, A.; Stack, J. Short Communication: Brucella Abortus Antibodies in The Sera of Indigenous and Exotic Avian Species In Nigeria. Anim. Health Prod. Afr. 2011, 58, 382–384. https://doi.org/10.4314/bahpa.v58i4.64236.
- Ocholi, R.; Kwaga, J.; Ajogi, I.; Bale, J. Phenotypic characterization of Brucella strains isolated from livestock in Nigeria. Microbiol. 2004, 103, 47–53. https://doi.org/10.1016/j.vetmic.2004.06.012.
- Gusi, A.M.; Bertu, W.J.; De Miguel, M.J.; Dieste-Pérez, L.; Smits, H.L.; Ocholi, R.A.; Blasco, J.M.; Moriyon, I.; Muñoz, P.M. Comparative performance of lateral flow immunochromatography, iELISA and Rose Bengal tests for the diagnosis of cattle, sheep, goat and swine brucellosis. PLOS Neglected Trop. Dis. 2019, 13, e0007509. https://doi.org/10.1371/journal.pntd.0007509.
- Tijjani, A.O.; Junaidu, A.U.; Salihu, M.D.; Farouq, A.A.; Faleke, O.O.; Adamu, S.G.; Musa, H.I.; Hambali, I.U. Serological survey for Brucella antibodies in donkeys of north-eastern Nigeria. Anim. Health Prod. 2017, 49, 1211–1216. https://doi.org/10.1007/s11250-017-1318-4.
- Adamu, S.G.; Hassan, M.; Ardo, M.B. Seroprevalence of Brucella antibodies in Donkeys (Equus asinus) in Yobe south senatorial zone, Northeastern Nigeria. Equine Sci. 2020, 31, 5–10. https://doi.org/10.1294/jes.31.5.
- Mai, H.M.; Irons, P.C.; Kabir, J.; Thompson, P.N. A large seroprevalence survey of brucellosis in cattle herds under diverse production systems in northern Nigeria. BMC Vet. Res. 2012, 8, 144. https://doi.org/10.1186/1746-6148-8-144.
- Adamu, N.B.; Adamu, S.G.; Jajere, M.S.; Atsanda, N.N.; Mustapha, F.B.; Mama, M. Serological survey of brucellosis in slaughtered local chicken, guinea fowl, duck and turkey in North eastern Nigeria. J. of poultry sci. 2014. 13, 6:340-342:
- Ocholi, R.A.; Kwaga, J.K.; Ajogi, I.; Bale, J.O. Abortion due to Brucella abortus in sheep in Nigeria. Sci. Tech. 2005, 24, 973–979.
- Olufemi, O.T.; Dantala, D.B.; Shinggu, P.; Dike, U.A.; Otolorin, G.R.; Nwuku, J.A.; Baba-Onoja, E.B.T.; Jatau, T.D.; Amama, F.I. Seroprevalence of Brucellosis and Associated Risk Factors among Indigenous Breeds of Goats in Wukari, Taraba State, Nigeria. Pathog. 2008, 1, 5257926. https://doi.org/10.1155/2018/5257926.
- Jajere, S.M.; Atsanda, N.N.; Bitrus, A.A.; Hamisu, T.M.; Ayo, A.O. Seroprevalence of brucellosis among cattle slaughtered in three municipal abattoirs of Gombe state, Northeastern Nigeria. World 2016, 9, 1082–1086. https://doi.org/10.14202/vetworld.2016.1082-1086.
- Baba, M.M.;Sarkindared, S.E.;Brisibe, F. Serological evidence of brucellosis among predisposed patients with pyrexia of unknown origin in the north eastern Nigeria. Central Eur. J. Public Health 2001, 9, 158–161.
- Ardo, M.B.; Abubakar, D.M. Seroprevalence of horse (Equus caballus) brucellosis on the Mambilla plateau of Taraba State, Nigeria. Equine Sci. 2016, 27, 1–6. https://doi.org/10.1294/jes.27.1.
- Sadiq, M.A.; Ajogi, I.; Bale, J.O.O.; Mosimabale, F.B.; Tijjani, A.N.; Auwal, M.S.; Mustapha, A.R.; Kudi, A.C. Epidemiological investigation of brucellosis in one humped camel (Camelus dromedarius) in Lake Chad area of Borno state, Nigeria. Camel Pract. Res. 2010, 17, 2: 1-6.
- Mai, H.M.; Irons, P.C.; Thompson, P.N. Brucellosis, genital campylobacteriosis and other factors affecting calving rate of cattle in three states of Northern Nigeria. BMC Vet. Res. 2015, 20, 7. https://doi.org/10.1186/s12917-015-0317-9.
- Ibrahim, Y.; Mai, H.M.; Kalla, D.J.U.; Kabir, J.; Nathaniel, J. Seroprevalence and potential risk factors of bovine brucellosis at the livestock-wildlife interface area of Yankari game reserve, Bauchi State, Nigeria. J. Anim. Prod. 2019, 46, 33–44. https://doi.org/10.51791/njap.v46i4.292.
- Atsanda, N.; Liba, J.; Francis, M.; Malgwi, H. Serological survey of brucellosis among internally displaced persons in Maiduguri, North eastern Nigeria. Sokoto J. Vet. Sci. 2018, 16, 61–65. https://doi.org/10.4314/sokjvs.v16i3.9.
- Sadiq, M.A.; Ajogi, I.; Bale, J.O.O.; Mosimabale, F.B.; Tijjani, A.N.; Kaikabo, A.A. Serological survey of antibodies against Brucella organism in one-humped camels (Camelus dromedarius) in Lake Chad area of Borno state, North-eastern Nigeria. Nig. Vet. J. 2011, 32, 1: 45-48.
- Audu, Y.; Maikai, B.V.; Okolocha, E.C. Survey for Brucella antibodies in dogs in Billiri local government area of Gombe State, Nigeria. Res. J. 2018, 6, 43.
- Adamu, S.G.; Atsanda, N.N.; Tijjani, A.O.; Usur, A.M.; Sule, A.G.; Gulani, I.A. Epidemiological study of bovine brucellosis in three senatorial zones of Bauchi State, Nigeria. World 2016, 9, 48–52. https://doi.org/10.14202/vetworld.2016.48-52.
- Adamu, S.; Tijjani, A.; Adamu, N.; Atsanda, N.; Ali, S.; Gashua, M.; Simon, C. Seroprevalence of Brucellosis in one-humped camel (Camelus dromedarius) herds in Yobe State, Nigeria. J. Livest. Res. 2014, 4, 36–42. https://doi.org/10.5455/ijlr.20140626045141.
- Sadiq, M.A.; Tijjani, A.-N.; Auwal, M.S.; Mustapha, A.R.; Gulani, I. Serological Prevalence of Brucellosis among Donkeys (Equus asinus) in Some Local Government Areas of Yobe State, Nigeria. Equine Vet. Sci. 2013, 33, 150–154. https://doi.org/10.1016/j.jevs.2012.05.071.
- Adamu, N.B.; Adeniyi, S.O.; Adamu, S.G.; Bale, J.O.O.; Okoh, A.E.J.; Umaru, G.A.; Umar, Y.A. Seroprevalence of brucellosis among livestock workers at Maiduguri cattle market, Borno State, North-Eastern, Nigeria. Public Health Epidemiol. 2015, 7, 253–257.
- Igawe, P.B.; Okolocha, E.; Kia, G.S.; Irmiya, I.B.; Balogun, M.S.; Nguku, P.; Bugun, I.I. Seroprevalence of brucellosis and associated exposure factors among in Bauchi state, Nigeria. Pan Afr. Med. J. 2020, 35, 33. https://doi.org/10.11604/pamj.2020.35.33.18134.
- Gusi, A.M.; Ocholi, R.A.; Bertu, W.J.; Moses, H.; Ibrahim, L.; Mwankon, E.; Wungak, Y.; Woma, T.Y.; Wularamu, H.G.; Madu, G.A.; et al. Sero-prevalence of camel brucellosis in three abbatoirs of Nothern Nigeria. Vet. Med. Anim. Health 2016, 8, 15–20. https://doi.org/10.5897/jvmah2015.0380.
- Adamu, M.; Mshelia, G.D.; Adamu, N.; Ouda, L.; Egwu, G.O. Studies on farmer awareness on caprine abortion and the presence of Brucella abortus and Brucella melitensis in selected flocks in an arid zone of Nigeria. Vet. Med. Anim. Health 2012, 4, 17–21.
- Junaidu, A.U.; Oboegbulem, S.I.; Salihu, M.D. Serological survey of Brucella antibodies in breeding herds. Microbiol. Biotechnol. Res. 2011, 11, 60–65.
- Nathaniel, J.; Kalla, D.J.U.; Mai, H.M.; Ibrahim, Y.; Mujitaba, M.A.; Amaduruonye, W.; Akinsola, K.L.; Obasi, E.N.; Suleiman, Y. Seroprevalence of brucellosis in donkeys (Equus asinus) and assessment of donkey management practices in Gamawa local government area, Bauchi state, Nigeria. J. Anim. Sci. 2019, 21, 134–144.
- Akinseye, V.O.; Adesokan, H.K.; Ogugua, A.J.; Adedoyin, F.J.; Otu, P.I.; Kwaghe, A.V.; Kolawole, N.O.; Okoro, O.J.; Agada, C.; Tade, A.O.; et al. Sero-epidemiological survey and risk factors associated with bovine brucellosis among slaughtered cattle in Nigeria. Onderstepoort J. Vet. Res. 2016, 83, 1002. https://doi.org/10.4102/ojvr.v83i1.1002.
- Salisu, U.; Kudi, C.; Bale, J.; Babashani, M.; Kaltungo, B.; Saidu, S.; Asambe, A.; Baba, A. Seroprevalence of Brucella antibodies in camels in Katsina State, Nigeria. Anim. Health Prod. 2017, 49, 1041–1046. https://doi.org/10.1007/s11250-017-1297-5.
- Adamu, S.G.; Kabir, J.; Umoh, J.U.; Raji, M.A. Seroprevalence of brucellosis and Q fever (Coxiellosis) in cattle herds in Maigana and Birnin Gwari agro-ecological zone of Kaduna State, Nigeria. Anim. Health Prod. 2018, 50, 1583–1589. https://doi.org/10.1007/s11250-018-1598-3.
- Kaltungo, B.Y.; Saidu, S.N.A.; Sackey, A.K.B.; Kazeem, H.M. Serological Evidence of Brucellosis in Goats in Kaduna North Senatorial District of Kaduna State, Nigeria. ISRN Vet. Sci. 2013, 2013, 963673. https://doi.org/10.1155/2013/963673.
- Obiako, O.R.; Ogoina, D.; Danbauchi, S.S.; Kwaifa, S.I.; Chom, N.D.; Nwokorie, E. Neurobrucellosis—a case report and review of literature. J. Clin. Pract. 2010, 13, 347–350.
- Mohammed, F.U.; Ibrahim, S.; Ajogi, I.; Olaniyi, B.J.O. Prevalence of Bovine Brucellosis and Risk Factors Assessment in Cattle Herds in Jigawa State. ISRN Vet. Sci. 2011, 27, 132897. https://doi.org/10.5402/2011/132897.
- Junaidu, A.U.; Salihu, M.D.; Gulumbe, M.L. Seroprevalence of Brucellosis in sheep in Sokoto city abattoir. J. Biol. Sci. 2006, 9, 2696–2698.
- Buhari, H.U.; Sn, A.S.; Mohammed, G.; Raji, M.A. Serological evaluation of bovine brucellosis in the North Senatorial District of Kaduna State, Nigeria. J. Vet. Sci. 2016, 5, 24–28.
- Onoja, I.I.; Mshelia, W.P.; Andrew, A.; Usman, B.; Sambo, K.W. A Case of Brucellosis in a One and Half-year-old Uda Sheep in Zaria. Sahel J. Vet. Sci. 2012, 11, 7–10.
- Junaidu, A.U.; Garba, B. Seroprevalence of Brucella antibodies in horses in Sokoto metropolis, Nigeria. Anim. Sci. Vet. Med. 2019, 4, 173–177.
- Adesiyun, A.G.; Folagbade, O.B.; Olayinka, A.T.; Randawa, A.; Bawa, U. Seroprevalence of brucellosis among women with miscarriage at Ahmadu Bello University Teaching Hospital, Zaria. J. Obstet. Gynaecol. 2017, 34, 145–151. https://doi.org/10.4103/tjog.tjog_29_17.
- Shu'Aibu, G.; Kabir, J.; Umoh, J.; Raji, M.; Tijjani, A.; Umaru, G. Seroprevalence of Brucellosis in sheep in Maigana and Birnin Gwari agro-ecological zones of Kaduna State, Nigeria. Vet. J. 2018, 39, 240–249. https://doi.org/10.4314/nvj.v39i3.7.
- Mohammed, F.; Ibrahim, S.; Musa, G.; Kaltungo, B.; Danbirni, S.; Kwaga, J. Brucella infection in migratory cattle herds in Jigawa State Nigeria: A cross sectional study. Sokoto J. Vet. Sci. 2020, 14, 191–194. https://doi.org/10.4314/sokjvs.v18i4.2.
- Onoja, I.I.; Ajani, A.J.; Mshelia, W.P.; Andrew, A.; Ogunkoya, A.B.; Achi, C.R.; Sambo, K.W. Brucellosis outbreak in a flock of seventeen sheep in Zaria. Sokoto J. Vet. Sci. 2008, 7, 2.
- Cadmus, S.; Salam, S.P.; Adesokan, H.K.; Akporube, K.; Ola-Daniel, F.; Awosanya, E.J. Seroprevalence of brucellosis and Q fever infections amongst pastoralists and their cattle herds in Sokoto State, Nigeria. PLoS ONE 2021, 16, e0254530. https://doi.org/10.1371/journal.pone.0254530.
- Kaltungo, B.; Saidu, S.; Kudi, C.; Isma’Il, M.; Jacob, R.; Salisu, U.; Baba, Y.; Buhari, H. Geo-spatial distribution of Brucella melitensis infection in selected local government areas of Katsina and Sokoto States, Nigeria. Vet. J. 2019, 40, 95–103. https://doi.org/10.4314/nvj.v40i2.1.
- Yusuf, Y.; Abdulrasheed, A. Survey on Bovine Brucellosis in Sokoto Metropolitan Abattoir, Nigeria. Anim. Vet. Adv. 2019, 18, 143–146. https://doi.org/10.36478/javaa.2019.143.146.
- Junaidu, A.U.; Garba, H.S. Application of competitive ELISA (cELISA) Rose Bengal plate test (RBPT) and serum agglutination test (SAT) for detection of antibodies to Brucella infection in slaughter cattle in Sokoto, Nigeria. Sahel J. Vet. Sci. 2006, 5, 9–12.
- Buhari, H.; Saidu, S.; Kudi, C.; Okolocha, E.; Kaltungo, B. Seroprevalence of Brucella infection in small ruminants from two institutional farms and a slaughter slab in Zaria, Nigeria. Sokoto J. Vet. Sci. 2020, 18, 91–99. https://doi.org/10.4314/sokjvs.v18i2.5.
- Dogo, R.; Maikai, B.V.; Musa, J.A.; Tizhe, J.Q. Brucella Prevalence in Goats and Farmers’ Awareness and Practices towards Brucella Infection in Giwa Area of Kaduna State Nigeria. Microbiol. Res. J. 2016, 16, 1–12. https://doi.org/10.9734/bmrj/2016/27092.
- Zubairu, A.; Ardo, M.; Mai, H. Seroprevalence of ruminant brucellosis in three selected local government areas of Taraba state. Sokoto J. Vet. Sci. 2014, 12, 51–56. https://doi.org/10.4314/sokjvs.v12i1.8.
- Farouk, U.M.; Bale, J.O.O.; Kwaga, J.K.P.; Abdullahi, U.S.; Ibrahim, S.; Madobi, I.S. Preliminary study on brucellosis in cattle in Jigawa state Nigeria. In Proceedings of the 54th Annual Congress of the Nigerian Veterinary Medical Association, Printed by University Press Limited Zaria, Kaduna State, Nigeria, 2017; pp. 66–71.
- Lawal, N.; Egwu, G.O.; Tambuwal, F.M.; Junaidu, A.U.; Abubakar, M.B.; Magaji, A.A.; Rabi’u, M.A.; Saulawa, M.A.; Mamuda, A.; Jibrin, M.S.; et al. 2012. Prevalence of Brucella abortus antibodies in bovine serum from gusau modern abattoir, Zamfara state, Nigeria. J. Microbiol. 2012, 1, 91–96.
- Kaltungo, B.Y.; Saidu, S.N.A.; Sackey, A.K.B.; Kazeem, H.M. Sero-prevalence of brucellosis in sheep in North Senatorial District of Kaduna State, Nigeria. Asian Pac. J. Trop. Dis. 2015, 5, 163–168. https://doi.org/10.1016/s2222-1808(14)60646-0.
- Bale, J.O.O.; Nuru, S.; Addo, P.B.; Adeyinka, I.A. Bacteriological investigation of sheep and goats milk for brucellosis in government farms in Northern Nigeria. J. Anim. Prod. 2013, 30, 107–116.
- Mbuk, E.U.; Ajogi, I.; Bale, J.; Umoh, J.U. Prevalence of Brucella Antibodies in Migratory Fulani Cattle Herds in Kaduna State, Nigeria. Vet. J. 2011, 32, 1. https://doi.org/10.4314/nvj.v32i1.68999.
- Osinubi, M.; Ajogi, I.; Ehizibol, O. Brucella abortus agglutinins in dogs in Zaria, Nigeria. Vet. J. 2004, 25, 35–38. https://doi.org/10.4314/nvj.v25i1.3464.
- Ekere, S.O.; Njoga, E.O.; Onunkwo, J.I.; Njoga, U.J. Brucella seropositivity in slaughter food animals and role of slaughterhouse workers in spread of Brucella infection in Southeast Nigeria. World 2018, 11, 1171–1178. https://doi.org/10.14202/vetworld.2018.1171-1178.
- Anyaoha, C.O.; Majesty-Alukagberie, L.O.; Ugochukwu, I.C.I.; Nwanta, J.A.; Anene, B.M.; Oboegbulam, S.I. Seroprevalencia y factores de riesgo de la brucelosis en perros de los Estados Enugu y Anambra, Nigeria. Med. Vet. 2020, 1, 45–59.
- Ogbodo, S.O.; Isiofia, O.P.; Uzodinma, B.A. Co-existence and seroprevalence of brucellosis in a malaria-endemic metropolis of south-eastern Nigeria. Exp. Res. 2016, 4, 2.
- Onunkwo, J.I.; Njoga, E.O.; Njoga, U.J.; Ezeokafor, E.; Ekere, S.O. Brucella seropositivity in chicken and risk factors for Brucella infection at the animal-human interface in Anambra State, Nigeria. J. One Health 2018, 4, 28–34. https://doi.org/10.14202/ijoh.2018.28-34.
- Onunkwo, J.; Njoga, E.; Nwanta, J.; Shoyinka, S.; Onyenwe, I.; Eze, J. Serological Survey of Porcine Brucella Infection in SouthEast, Nigeria. Vet. J. 2011, 32, 1. https://doi.org/10.4314/nvj.v32i1.68989.
- Njoga, E.O.; Onunkwo, J.I.; Ekere, S.O.; Njoga, U.J.; Okoro, W.N. Seroepidemiology of Equine Brucellosis and Role of Horse Carcass Processors in Spread of Brucella Infection in Enugu State, Nigeria. J. Curr. Res. Rev. 2018, 10, 39–45. https://doi.org/10.31782/ijcrr.2018.10106.
- Bello-Onaghise, G.; Vaikosen, S.E.; Evivie, S.E. abortion cases in pig farms in Benin city and some surrounding communities in Edo State, Nigeria. J. Agri. Food Env. 2012, 8, 37–42.
- Owowo, E.E.; Antia, U.E.; Christopher, M.A.; Okon, I.E. Sero-Prevalence of Brucellosis among Nomadic Herdsmen, Abattoir and Livestock Workers in Niger-Delta Region, Nigeria. Biosci. Med. 2019, 7, 32–41. https://doi.org/10.4236/jbm.2019.710003.
- Maurice, N.A. Bacteriological and serological studies of bovine brucellosis in Obudu cattle ranch, Cross River State. Nigeria. J. Exp. Biol. 2013, 3, 484–488.
- Cadmus, S.I.B.; Adesokan, H.K.; Ajala, O.O.; Odetokun, W.O.; Perrett, L.L.; Stack, J.A. Seroprevalence of Brucella abortus and B. canis in household dogs in southwestern Nigeria: a preliminary report. S. Afr. Vet. Assoc. 2011, 82, 56–57. https://doi.org/10.4102/jsava.v82i1.35.
- Ayoola, M.C.; Akinseye, V.O.; Cadmus, E.; Awosanya, E.; Popoola, O.A.; Akinyemi, O.O.; Perrett, L.; Taylor, A.; Stack, J.; Moriyon, I.; et al. Prevalence of bovine brucellosis in slaughtered cattle and barriers to better protection of abattoir workers in Ibadan, South-Western Nigeria. Pan Afr. Med. J. 2017, 28, 68. https://doi.org/10.11604/pamj.2017.28.68.10925.
- Ukwueze, K.O.; Ishola, O.O.; Dairo, M.D.; Awosanya, E.J.; Cadmus, S.I. Seroprevalence of brucellosis and associated factors among livestock slaughtered in Oko-Oba abattoir, Lagos State, southwestern Nigeria. Pan Afr. Med. J. 2020, 36, 53. https://doi.org/10.11604/pamj.2020.36.53.21094.
- Cadmus, S.I.; Alabi, P.I.; Adesokan, H.K.; Dale, E.J.; Stack, J.A. Serological investigation of bovine brucellosis in three cattle production systems in Yewa Division, south-western Nigeria. S. Afr. Vet. Assoc. 2013, 84, E1–E6. https://doi.org/10.4102/jsava.v84i1.217.
- Ayinmode, A.; Akinseye, V.; Schares, G.; Cadmus, S. Serological survey of toxoplasmosis, neosporosis, and brucellosis among cattle herds in Oyo State, south-western Nigeria. J. Infect. Dis. 2017, 11, 95–101. https://doi.org/10.21010/ajid.v11i2.13.
- Cadmus, S.; Adesokan, H.; Stack, J. The use of the milk ring test and rose bengal test in brucellosis control and eradication in Nigeria. S. Afr. Vet. Assoc. 2008, 79, 113–115. https://doi.org/10.4102/jsava.v79i3.256.
- Cadmus, S.I.; Adesokan, H.K.; Adedokun, B.O.; Stack, J.A. eroprevalence of bovine brucellosis in trade cattle slaughtered in Ibadan, Nigeria, from 2004-2006. S. Afr. Vet. Assoc. 2010, 81, 50–53. https://doi.org/10.4102/jsava.v81i1.96.
- Adeyemi, A.K. Survey of Brucellosis among People at Risk in Lagos, Nigeria. Master’s Dissertation, University of South Africa, 2018.
- Cadmus, S.; Osikoya, I.; Adesokan, H. Brucellosis in trade cattle in Lagos state: An investigation of two Abattoirs. Vet. J. 2008, 29, 4. https://doi.org/10.4314/nvj.v29i4.65151.
- Bwala, D.G.; McCrindle, C.; Fasina, F.O.; Ijagbone, I. Abattoir characteristics and seroprevalence of bovine brucellosis in cattle slaughtered at Bodija Municipal Abattoir, Ibadan, Nigeria. Vet. Med. Anim. Health 2015, 7, 164–168.
- Ogugua, A.J.; Akinseye, V.O.; Cadmus, E.O.; Awosanya, E.A.J.; Alabi, P.I.; Idowu, O.S.; Akinade, S.A.; Dale, E.J.; Perrett, L.; Taylor, A.; et al. Prevalence and risk factors associated with bovine brucellosis in herds under extensive production system in southwestern Nigeria. Anim. Health Prod. 2018, 50, 1573–1582. https://doi.org/10.1007/s11250-018-1597-4.
- Comfort, A.M.; Joseph, O.A.; Oluwatoyin, A.V.; Joshua, T.O.; Folusho, B.M.; Julianah, A.F.; Kehinde, A.H.; Olutayo, O.T.; Olusoji, A.J.; Ihuaku, O.P.; et al. Sero-epidemiological survey and risk factors associated with brucellosis in dogs in south-western Nigeria. Pan Afr. Med. J. 2016, 23, https://doi.org/10.11604/pamj.2016.23.29.7794.
- Cadmus, S.; Ijagbone, I.; Oputa, H.; Adesokan, H.; Stack, J. Serological survey of Brucellosis in livestock animals and workers in Ibadan, Nigeria. J. Biomed. Res. 2009, 9, 3. https://doi.org/10.4314/ajbr.v9i3.48900.
- Dean, A.S.; Crump, L.; Greter, H.; Hattendorf, J.; Schelling, E.; Zinsstag, J. Clinical Manifestations of Human Brucellosis: A Systematic Review and Meta-Analysis. PLOS Negl. Trop. Dis. 2012, 6, e1929. https://doi.org/10.1371/journal.pntd.0001929.
- Laine, C.G.; Wade, A.; Scott, H.M.; Krecek, R.C.; Arenas-Gamboa, A.M. Scoping review of brucellosis in Cameroon: Where do we stand, and where are we going?. PLoS ONE 2020, 15, e0239854. https://doi.org/10.1371/journal.pone.0239854.
- Kahariri, S.M.; Kitala, P.M.; Muchemi, G.M.; Njenga, K.; Nanyingi, M. Sero-prevalence and risk factors for human brucellosis in Marsabit county, Kenya (2014). PAMJ One Health 2021, 4, 9. https://doi.org/10.11604/pamj-oh.2021.4.9.27024.
- Mehari, S.; Zerfu, B.; Desta, K. Prevalence and risk factors of human brucellosis and malaria among patients with fever in malaria-endemic areas, attending health institutes in Awra and Gulina district, Afar Region, Ethiopia. BMC Infect. Dis. 2021, 21, https://doi.org/10.1186/s12879-021-06654-y.
- Tumwine, G.; Matovu, E.; Kabasa, J.D.; Owiny, D.O.; Majalija, S. Human brucellosis: sero-prevalence and associated risk factors in agro-pastoral communities of Kiboga District, Central Uganda. BMC Public Health 2015, 15, 900. https://doi.org/10.1186/s12889-015-2242-z.
- Diab, M.S.; Zidan, S.A.A.; Hassan, N.A.A.; Elaadli, H.; Bayoumi, A.M. Seroprevalence and Associated Risk Factors of Brucellosis in Livestock and Residents of New Valley Governorate, Egypt. World's Vet. J. 2020, 10, 531–539. https://doi.org/10.54203/scil.2020.wvj64.
- Sagamiko, F.D.; Mfune, R.L.; Hang’Ombe, B.M.; Karimuribo, E.D.; Mwanza, A.M.; Sindato, C.; Muma, J.B. Seroprevalence of human Brucellosis and associated risk factors among high-risk occupations in Mbeya Region of Tanzania. Epidemiol. Res. 2020, 6, 1. https://doi.org/10.5430/jer.v6n1p1.
- Njeru, J.; Wareth, G.; Melzer, F.; Henning, K.; Pletz, M.W.; Heller, R.; Neubauer, H. Systematic review of brucellosis in Kenya: disease frequency in humans and animals and risk factors for human infection. BMC Public Health 2016, 16, 853. https://doi.org/10.1186/s12889-016-3532-9.
- Bale, J.O.; Kumi-Diaka, J. Serological and bacteriological study of bovine Brucellae from livestock investigation and breeding centers in Nigeria. Vet. J. 1981, 37, 256–261.
- Gameel, S.E.A.M.; Mohamed, S.O.; Mustafa, A.A.; Azwai, S.M. Prevalence of camel brucellosis in Libya. Anim. Health Prod. 1993, 25, 91–93. https://doi.org/10.1007/bf02236513.
- Lucero, N.E.; Ayala, S.M.; Escobar, G.I.; Jacob, N.R. Brucella isolated in humans and animals in Latin America from 1968 to 2006. Infect. 2008, 136, 496–503. https://doi.org/10.1017/s0950268807008795.
- Minharro, S.; Mol, J.P.S.; Dorneles, E.M.S.; Pauletti, R.B.; Neubauer, H.; Melzer, F.; Poester, F.P.; Dasso, M.G.; Pinheiro, E.S.; Filho, P.M.S.; et al. Biotyping and Genotyping (MLVA16) of Brucella abortus Isolated from Cattle in Brazil, 1977 to 2008. PLoS ONE 2013, 8, e81152. https://doi.org/10.1371/journal.pone.0081152.
- Sanogo, M.; Thys, E.; Achi, Y.L.; Fretin, D.; Michel, P.; Abatih, E.; Berkvens, D.; Saegerman, C. Bayesian estimation of the true prevalence, sensitivity and specificity of the Rose Bengal and indirect ELISA tests in the diagnosis of bovine brucellosis. J. 2013, 195, 114–120. https://doi.org/10.1016/j.tvjl.2012.06.007.
- Liu, F.; Li, J.-M.; Zeng, F.-L.; Zong, Y.; Leng, X.; Shi, K.; Diao, N.-C.; Li, D.; Li, B.-Y.; Zhao, Q.; et al. Prevalence and Risk Factors of Brucellosis, Chlamydiosis, and Bluetongue Among Sika Deer in Jilin Province in China. Vector Borne Zoonotic Dis. 2018, 18, 226–230. https://doi.org/10.1089/vbz.2017.2226.
- Alton, G.G.; Jones, L.M.; Angus, R.D.; Verger, J.M. Techniques for the Brucellosis Laboratory; INRA: Paris, France, 1988.
- Bricker, B.J.; Ewalt, D.R.; Halling, S.M. Brucella ‘HOOF-Prints’: strain typing by multi-locus analysis of variable number tandem repeats (VNTRs). BMC Microbiol. 2003, 3, 15. https://doi.org/10.1186/1471-2180-3-15.
- Le Flèche, P.; Jacques, I.; Grayon, M.; Al Dahouk, S.; Bouchon, P.; Denoeud, F.; Nöckler, K.; Neubauer, H.; Guilloteau, L.A.; Vergnaud, G. Evaluation and selection of tandem repeat loci for a Brucella MLVA typing assay. BMC Microbiol. 2006, 6, 9–14. https://doi.org/10.1186/1471-2180-6-9.
- Robinson, R. Emergency Prevention System for Transboundary Animal and Plant Pests and Diseases. In Guidelines for Coordinated Human and Animal Brucellosis Surveillance; Food and Agriculture Organization of the United Nations: Rome, Italy, 2003.
- World Organization for Animal Health (OIE). Bovine Brucellosis. In Manual of Diagnostic Test and Vaccines for Terrestrial Animals; OIE: Paris, France, 2009; Chapter 2.4.3., pp. 1–35.
- Khan, M.Z.; Zahoor, M. An Overview of Brucellosis in Cattle and Humans, and its Serological and Molecular Diagnosis in Control Strategies. Med. Infect. Dis. 2018, 3, 65. https://doi.org/10.3390/tropicalmed3020065.
| Region | State | No of Samples Tested | No of Positive Sample | Seroprevalence % |
Detection Methods | Brucella Type | Reference | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RBPT | SAT | cELISA | iELISA | IgM | IgG | IgG/IgM ELISA |
Brucella spp. | Brucella abortus | Brucella melitensis |
||||||
| NC | Kwara | 189 | 42 | 22.2% | 42 | 0 | 0 | 0 | 0 | 0 | 0 | 42 | 0 | 0 | [42] |
| Abuja | 224 | 40 | 17.9% | 40 | 0 | 0 | 0 | 22 | 18 | 0 | 40 | 0 | 0 | [43] | |
| Nasarawa | 160 | 16 | 10% | 16 | 0 | 0 | 0 | 0 | 0 | 0 | 16 | 0 | 0 | [44] | |
| Total | 573 | 98 | 17.1% | 98 | 0 | 0 | 0 | 22 | 18 | 0 | 98 | 0 | 0 | ||
| NE | Bauchi | 285 | 95 | 33.3% | 95 | 0 | 0 | 0 | 6 | 18 | 0 | 95 | 0 | 0 | [45] |
| Not indicated | 500 | 26 | 5.2% | 26 | 0 | 0 | 0 | 0 | 0 | 0 | 26 | 0 | 0 | [46] | |
| Borno | 106 | 4 | 3.8% | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 0 | 0 | [47] | |
| Borno | 100 | 11 | 11% | 11 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 11 | 0 | [48] | |
| Total | 990 | 136 | 13.7% | 136 | 0 | 0 | 0 | 6 | 18 | 0 | 125 | 11 | 0 | ||
| NW | Kaduna | 1 | 1 | 100% | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | [49] |
| Kaduna | 100 | 19 | 19% | 0 | 0 | 0 | 19 | 0 | 0 | 0 | 19 | 0 | 0 | [50] | |
| Sokoto | 137 | 1 | 0.7% | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | [51] | |
| Total | 238 | 21 | 8.8% | 1 | 1 | 0 | 19 | 0 | 0 | 0 | 19 | 2 | 0 | ||
| SE | Enugu | 682 | 195 | 28.6% | 195 | 0 | 0 | 0 | 0 | 0 | 0 | 195 | 0 | 0 | [41] |
| Total | 682 | 195 | 28.6% | 195 | 0 | 0 | 0 | 0 | 0 | 0 | 195 | 0 | 0 | ||
| SS | Akwa Ibom | 228 | 70 | 30.7% | 29 | 0 | 0 | 0 | 0 | 41 | 0 | 0 | 0 | 70 | [52] |
| Total | 228 | 70 | 30.7% | 29 | 0 | 0 | 0 | 0 | 41 | 0 | 0 | 0 | 70 | ||
| SW | Lagos | 422 | 27 | 6.4% | 27 | 0 | 0 | 3 | 0 | 0 | 0 | 27 | 0 | 0 | [53] |
| Oyo | 11 | 7 | 63.6% | 7 | 0 | 0 | 0 | 0 | 0 | 0 | 7 | 0 | 0 | [54] | |
| Total | 433 | 34 | 7.9% | 34 | 0 | 0 | 3 | 0 | 0 | 0 | 34 | 0 | 0 | ||
| Grand Total | 3144 | 554 | 17.6% | 493 | 1 | 0 | 22 | 28 | 77 | 0 | 471 | 13 | 70 | ||
Author Contributions: Conceptualization, K.O.A. (Kabiru O. Akinyemi); methodology, C.O.F. K.O.A. (Kabiru O. Akinyemi) and K.O.A. (Kehinde O. Amisu); software, C.O.F.; validation, K.O.A. (Kabiru O. Akinyemi), C.O.F. and G.W.; formal analysis, C.O.F.; investigation, C.O.F.; resources, K.O.A. (Kabiru O. Akinyemi), C.O.F. and G.W.; data curation, K.O.A. (Kabiru O. Akinyemi) and C.O.F.; writing—original draft preparation, C.O.F.; writing review and editing, K.O.A. (Kabiru O. Akinyemi) and G.W.; visualization, K.O.A. (Kabiru O. Akinyemi), G.W., K.O.A. (Kehinde O. Amisu) and C.O.F.; supervision, K.O.A. (Kabiru O. Akinyemi); co-supervision, K.O.A. (Kehinde O. Amisu); project administration, Lagos State University funding acquisition, None. All authors have read and agreed to the published version of the manuscript.
References
- Corbel, M.J.
