1. ALL Regimen vs. AML and Lymphoma Regimens
The most common treatment for
blastic plasmacytoid dendritic cell neoplasm (BPDCN
) is induction therapy based on regimens used for acute leukemia (both AML and ALL) or non-Hodgkin’s lymphoma (NHL). NHL regimens generally comprise CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone) or CHOP-like regimens. ALL regimens comprise hyper-CVAD (hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone alternating with high-dose methotrexate and cytarabine) regimens or high doses of methotrexate combined with asparaginase.
acute myeloid leukemia (AML)AML regimens usually comprise cytarabine combined with daunorubicin or idarubicin. In a retrospective study, Taylor et al. compared the use of these different regimens as a first-line treatment for BPDCN
[1][5]. Their study was based on 59 patients identified in three different centers in the United States. Patients treated with first-line lymphoid-type regimens showed improved progression-free survival (PFS) compared to those treated with myeloid regimens (2-year PFS; 40% vs. 11%, respectively;
p = 0.075). They also highlighted the impact of the regimen intensity used. Indeed, intensive regimens have led to a significantly increased PFS compared with non-intensive ones (2-year PFS; 45% vs. 11% respectively;
p = 0.034). Other retrospective studies also confirmed the positive outcome experienced by patients treated with lymphoid-type regimens
[2][3][4][5][6][6,7,8,9,10]. These studies have shown the necessity of consolidation to obtain prolonged survival. Laribi et al. showed that patients treated with lymphoid-type regimens followed by HSCT consolidation presented higher CR rates and lower relapse rates (ALL-type regimen: 94% achieved CR and 13% relapsed; NHL-type regimens: 100% achieved CR and 33% relapsed) than those treated with AML-type regimens followed by HSCT consolidation (88% achieved CR and 58% relapsed)
[3][7]. Thus, they confirmed that lymphoid-type treatments produce better outcomes; however, superior effects with a prolonged OS are only observed when consolidation is performed for eligible patients with HSCT. Based on collections established by the French BPDCN network, Garnache-Ottou’s group identified treatments received by patients in a series of 89 well-documented cases
[7][11]. They also demonstrated that leukemia-like regimens exhibited the highest response rate compared to less intense approaches with a median remission duration of 47 months in the AML-like (anthracyclines associated with cytarabine as in “5 1 7” AML treatments)/ALL-like (multi-drug associations as in ALL treatments)/AspaMTX (high-dose methotrexate with asparaginase) group compared with 7 months (
p = 5.038) in the CHOP-like (classical regimen used in the treatment of non-Hodgkin lymphomas and combining cyclophosphamide, doxorubicin, vincristine, and prednisone)/NOS group (all other drugs alone or in combination). Finally, in a recent publication on their website, the German Society of Hematology and Oncology published recommendations highlighting the use of leukemia regimens for eligible patients with BPDCN
[8][12].
Several cases have reported using multi-drug therapy combining methotrexate, L-asparaginase, and dexamethasone in this pathology
[9][13]. This combination is well-tolerated, with a response rate of approximately 70% for patients whose age and comorbidities allow for allo-HSCT
[9][10][11][13,14,15].
The Our
esearchers' team has previously demonstrated high efficacy of idarubicin on BPDCN primary cells with <1% of viable cells remaining after 18 h of treatment
[12][16]. Based on
the our
esearchers' previous results,
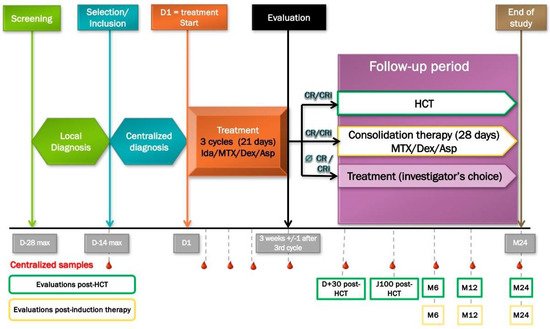
theywe proposed the first prospective phase II trial for patients with BPDCN to evaluate the effectiveness of three cycles of methotrexate, L-asparaginase, idarubicin, and dexamethasone for eligible patients, followed by allo-HSCT when CR is achieved (
Figure 1). This phase II study has been recruiting patients since January 2019 and has already included 20 patients with preliminary results for publishing soon (NCT03599960 Combination Chemotherapy in Patients with Newly Diagnosed BPDCN (LpDessai)). Preliminary data confirmed that the disease is a chemo-sensitive entity with a significant rate of first remissions and some adverse events with the need to monitor frail patients closely. The first security analysis emphasizes the remaining importance of adverse events in the frail population of BPDCN patients (unpublished data).
Figure 1. LpDessai clinical trial (NCT03599960) design. D, day; Ida, idarubicin; MTX, methotrexate; Dex, dexamethasone; Asp, asparaginase; CR, complete remission; Cri, complete remission with incomplete hematopoietic recovery; HCT, hematopoietic stem cell transplantation; M, month; wk, week.
2. Allo-HSCT
For many years, allo-HSCT has been the standard consolidation treatment for BPDCN patients who are fit for this therapy and achieve CR1. The results depend on the intensity of the conditioning regimen (myeloablative conditioning or reduced-intensity regimen), type of treatment, stage of disease, initial presentation, and age of patients. In a meta-analysis involving 128 patients, Kharfan-Dabaja et al. showed a pooled OS of 67% for patients allografted at CR1 versus 7% for patients who received an allo-HSCT beyond CR1
[13][17]. In the same way, a retrospective study based on 86 patients identified in the French BPDCN network highlighted the efficacy of allo-HSCT in CR1 with no regard to previous treatment received. Among the 30 patients who received allo-HSCT, only 10 (33%) relapsed after a median time of 12 months, whereas all patients receiving auto-HSCT relapsed after 2, 4, 7, and 17 months (4/4 (100%))
[7][11]. A recent study by Brüggen et al. confirmed the superiority of allo-HSCT over any type of chemotherapeutic regimen
[4][8]. In a clinical study involving 398 patients published in 2020, Laribi et al. showed that chemotherapy followed by allo-HSCT in CR1, and to a lesser extent auto-HSCT, was associated with a significantly better outcome
[3][7]. In the absence of a randomized controlled trial comparing allo-HSCT with conventional chemotherapy or novel therapies in patients with BPDCN, and according to all published data, the optimal approach to achieve a long-term remission is allograft in the first CR regardless of the regimen used to obtain this remission
[5][9]. However, whether novel targeted therapies can be used without allotransplants as a consolidation remains a pending question.
3. Auto-HSCT
Few studies or limited data of case reports are available for an autologous-HSCT (auto-HSCT) evaluation. The vast majority of studies have shown the superiority of allo-HSCT, especially in CR1. However, Aoki et al. showed in a study of 25 patients receiving auto-HSCT in CR1 a 4-year PFS and OS of 73% and 82%, respectively, which are superior to patients receiving allo-HSCT (PFS: 60% and OS: 69%)
[14][18]. Nevertheless, these positive results must be nuanced. Numerous other studies do not share the same conclusion, as highlighted by Garnache-Ottou et al., whose four patients treated with auto-HSCT relapsed compared to only 10/30 of patients treated with allo-HSCT
[7][11]. To date, it is difficult to recommend it as a standard approach for BPDCN due to the limited number of auto-HSCT cases. This issue can probably be discussed in patients without initial marrow involvement (for instance, isolated cutaneous presentation) who also obtained a CR on all involved sites.
4. BCL-2 Inhibition
Targeted therapies have been more developed and evaluated in recent years since they are less aggressive and present promising results. Among them, Montero et al. performed an in vitro and in vivo proof of concept for the efficacy of venetoclax in BPDCN models overexpressing BCL-2 protein and relying on it to survive
[15][19]. Numerous case reports
[16][17][20,21] and clinical trials have also reported good results with fast regression of skin nodules and disease control even after several lines of treatment. However, relapses occur often, and studies have been implemented to evaluate them in combination with other agents. One of the most studied combinations is with 5-azacytidine, already approved (since 2018) for treating newly diagnosed AML for patients >75 years old or with comorbidities and ineligible for intensive induction chemotherapy
[18][19][20][21][22][22,23,24,25,26]. Thus, a combination of hypomethylating agents is currently under investigation in two different clinical trials against BPDCN (NCT03113643 and NCT03404193). Its association with low-intensity chemotherapy was also presented by Di Nardo et al. as a viable salvage option even in relapsed or refractory (R/R) patients, particularly those presenting a
RUNX1 and/or
IDH1/2 mutation
[23][27]. In the same way, Cherry et al. compared venetoclax plus 5-azacytidine to an induction chemotherapy (IC) regimen in AML management. They showed that the OS for venetoclax associated with 5-azacytidine was more favorable than the IC regimen in a propensity-matched cohort of patients with equivalent baseline factors. They also identified variables that can guide treatment decisions, such as RUNX1 mutation, which favors venetoclax plus 5-azacytidine over the IC regimen
[24][28].
These results showed that targeting BCL-2 protein remains an interesting strategy but leads to good short-term results when used alone. In order to prolong their efficacy, their association with other molecules is required. A combination with cell therapy may be considered since several studies have shown the positive impact of venetoclax on immune cells, especially T cells
[25][26][27][28][29,30,31,32].
5. Epigenetic Dysregulation Targeting
To better describe and understand BPDCN, Sapienza et al. studied whole-exome sequencing (WES) and its genetic characteristics. Several epigenetic modifiers were identified as bearing mutations, such as
ASXL1 and
TET2 [29][30][33,34]. Therefore,
thwe
researchers sstudied hypomethylating agents for BPDCN patient treatment, which showed promising results. The most commonly tested was the 5-azacytidine, approved by the FDA for the treatment of myelodysplastic syndrome in 2004
[31][35]. Although it showed good results as a monotherapy, more studies have reported its use in association with other treatments. Its capacity to modulate gene expression by hypomethylation may be used to overcome resistance issues and thus enhance other treatment efficacy. A resistance to tagraxofusp, a CD123-targeted therapy, was described by Lane et al. in a BPDCN model
[32][36]. This resistance works through the
DPH1 expression loss required for the efficacy of tagraxofusp. Azacytidine restored
DPH1 expression and thus the cell’s sensitivity to tagraxofusp. Its evaluation in a clinical trial with tagraxofusp is currently in progress (NCT03113643). It was also evaluated in association with venetoclax in two clinical trials and has been widely used in case reports, as this combination shows good results (NCT04216524 and NCT03113643).
6. Multiple Myeloma-Based Regimens
6.1. NF-κB Inhibition
Previous alternative treatment options targeted the NF-κB pathway. It is an interesting approach since BPDCN exhibits constitutive activation of the NF-κB pathway
[33][37]. Moreover, NF-κB inhibition in BPDCN cell lines using either an experimental specific inhibitor JSH23 or the clinical drug bortezomib interferes in vitro with leukemic cell proliferation and survival
[34][38].
The Our
esearchers' team confirmed that bortezomib inhibits the phosphorylation of the RelA NF-κB subunit efficiently into two BPDCN cell lines in vitro and in vivo.
The researchersWe demonstrated that bortezomib could be associated with other drugs used in different chemotherapy regimens (i.e., a histone deacetylase vorinostat (SAHA) and statins) to improve its impact on BDPCN cell death
[35][39]. In 2019, Marmouset et al. also described a promising combination of lenalidomide/bortezomib and dexamethasone with two complete responses and one complete remission
[36][40] after five cycles of this chemotherapy. These results justify using bortezomib in combination with other chemotherapies for treating BPDCN patients.
6.2. CD38 Targeting
A recent case report showed an encouraging clinical response in an elderly BPDCN patient treated with daratumumab-based therapy after prior azacytidine-venetoclax. Daratumumab is an anti-CD38 monoclonal human immunoglobulin G1 antibody that induces cell death and has important immunomodulatory activities in myeloma, which may also play a role in BPDCN
[37][41].
7. CD123-Targeted Therapies
7.1. Tagraxofusp
In the area of targeted therapies, target choice is a key point. For BPDCN, one largely described target was highly overexpressed by 100% of the patients. This target of choice was the alpha subunit of the IL3 receptor, called CD123. Among all the therapies developed to target it, SL-401 is the most described. Based on several clinical trials, it received US FDA approval for untreated or relapsed or refractory (R/R) BPDCN patients in December 2018
[38][42]. Afterward, it received EU approval in January 2021. The first clinical trial was led by Frankel et al., who presented an ORR of 78% (7/9 patients) comprising five CRs and two PRs
[39][43]. Some toxicities were noted but presented as manageable. Pemmaraju et al. led a prospective and multi-institutional study to confirm these first results on both frontline (FL) and R/R BPDCN patients. They observed 90% of ORR in the FL group, with 72% of patients presenting a CR or CRc. The OV at 2 years was 52%, and 45% of the patients were bridged to HSCT. In the R/R group, 67% of ORR was observed with an OS of 8.5 months. For the entire trial, 20% of patients presented CLS, causing two deaths
[40][44].
Currently, SL-401 is in several clinical trials on CD123 hemopathies in combination with azacytidine and venetoclax to enhance its efficacy
[41][45] (NCT03113643 and NCT04216524).
7.2. Other Therapies Targeting CD123
IMGN632 (Immunogen, Waltham, MA, USA) is a humanized monoclonal antibody targeting CD123, fused to a potent DNA alkylating agent. It was shown to be active in vitro and in vivo against BPDCN models, and studies suggested that normal hematopoietic stem cells should be preserved at their low expression of CD123
[42][46]. IMGN632 is currently being tested alone on untreated or R/R BPDCN patients; the first results showed an ORR of 30% (7/23) and CRc of 22% (NCT03386513)
[43][47]. No grade 3 or higher adverse events were noted (except for one patient). Th
ate study is still ongoing in Europe and the US. Based on this preliminary evidence, IMGN632 received a Breakthrough Therapy Designation in October 2020 for the treatment of BPDCN.
The surface expression of CD123 makes it a good target for immunotherapy, such as CAR-T cells (chimerix antigen receptor). Thus, since the beginning of the 2010s, numerous teams have worked on developing CD123-directed CAR-T cells and demonstrated their efficacy in AML and BPDCN. More academic teams and private companies are working on developing such products
[44][45][46][48,49,50]. Almost 30 trials are ongoing, evaluating CD123 CAR-T cells, mainly in AML, but some include BPDCN patients. No trials have ended, but some high toxicities are noticeable, such as cytokine release syndrome and capillary leak syndrome (due to the targeting of normal cells expressing CD123 at a low level) (NCT03203369). Thus, some works and trials are now adding a safety part in the CAR construct to limit toxicity (NCT02159495 and NCT04109482)
[47][48][51,52].