Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Stanislav Kotlyarov and Version 2 by Lindsay Dong.
Chronic obstructive pulmonary disease (COPD) is a widespread socially significant disease. The development of COPD involves the innate immune system. The regulation of the innate lung immune system is related to the gut microbiota. This connection is due to the production by gut microorganisms of short-chain fatty acids (SCFAs) such as acetate, propionate, and butyrate. Nutritional disturbances and changes in the structure of the intestinal microbiota lead to a decrease in SCFAs production and their effect on pulmonary immunity. The presence of a metabolic and immune axis linking the lungs and gut plays an important role in the pathogenesis of COPD.
- COPD
- gut microbiota
- short-chain fatty acids
1. Introduction
Chronic obstructive pulmonary disease (COPD) is one of the most common respiratory diseases of social significance [1]. It is an important cause of health care seeking, hospitalizations, and disability [2][3][2,3]. Epidemiological studies show unfavorable trends in the prevalence of COPD in many countries [4][5][4,5]. The urgency of the problem is also increased by the fact that COPD is among the leading causes of death in the world. Moreover, treatment and rehabilitation of patients remain an unsolved problem in many respects, which requires new more detailed data on pathophysiological mechanisms of disease development and on those parts of pathogenesis, which can be effectively influenced for therapeutic purposes.
The development and progression of the disease is associated with exposure to tobacco smoke components and exogenous aeropollutants [6][7][8][6,7,8]. Inflammation in the bronchial tree is known to underlie the pathogenesis of COPD and is characterised by the involvement of many cells, including macrophages and neutrophils [9]. Prolonged persistent inflammation is associated with impaired immune mechanisms that provide a balance between maintaining and resolving inflammation [10].
It is known that COPD is a disease characterized by both pulmonary and extrapulmonary clinical heterogeneity [11][12][11,12]. Moreover, some features of the clinical picture and phenotypes of COPD are related to nutrition. Body mass index (BMI) is considered as one of the important markers in assessing the prognosis of COPD [13]. Lower body weight is associated with a greater risk of adverse outcome, whereas excess body weight has an even better prognosis [14]. This phenomenon has been called the “obesity paradox” [15][16][17][15,16,17]. The course of COPD, in which higher energy requirements lead to loss of fat and muscle tissue, is thought to be prognostically unfavorable [18][19][18,19]. The increased energy requirement may be related both to respiration and to the maintenance of inflammation in the bronchi. Dietary modification is considered an important tool that can improve the clinical course of COPD [20]. It is suggested that the nature of nutrition may be related to the pathophysiological mechanisms of COPD not only through the influence on energy and metabolic processes, but also through the regulation of some immune mechanisms [21].
A growing body of evidence supports a metabolic and immune axis linking the gut and lungs [22][23][22,23]. These links are bidirectional, and the gut microbiome is one of the central links in this interaction. The gut is the site of localization of much of the commensal bacterial mass [24][25][24,25]. This microbiome is metabolically active, participating in the production of many substances, such as, short-chain fatty acids (SCFAs) [26]. Accumulating evidence suggests that SCFAs can be considered as a leading link in the metabolic and immune axis between the gut and lungs. Indeed, SCFAs exhibit a variety of functions in immune defence, making them a potentially important target for clinical and experimental research.
2. Short-Chain Fatty Acids in the Pathogenesis of COPD
The presence of SCFAs in the sputum confirms the connection between the lungs and the intestine [27][82]. SCFAs are thought to contribute to the maintenance of lung immunometabolic tone [28][74]. As already noted, SCFAs can act on various parts of the innate immune defenses of the lungs. In addition to the described anti-inflammatory effects, the protective role of butyrate and propionate may include the restoration and maintenance of the barrier function of damaged airway epithelium by increasing the expression of ZO-1 dense contact proteins [29][127]. This seems important given the development of airway epithelial barrier dysfunction and impaired tight cell contacts in smoking and COPD [30][128]. In this regard, the regulation of barrier function under the influence of SCFAs may have some clinical significance [29][127]. The results showed differences in the composition of the gut microbiome in COPD and in healthy individuals. This is consistent with lower overall levels of SCFAs in the stage III-IV COPD group than in patients with stage I-II COPD and in healthy individuals [31][129]. Experimental data indicate that transplantation of fecal microbiota to mice led to inflammation in the lungs and increased IL-1β and TNF-α in plasma. At the same time, additional exposure to smoke from the biomass led to an accelerated decrease in lung function, emphysematous changes, airway remodeling, and mucus hypersecretion. These changes were accompanied by higher levels of claudin 1, α smooth-muscle actin (α-SMA), neutrophil elastase (NE) and matrix metalloproteinase 2 (MMP-2), and MUC5AC. In addition, gut microbiota obtained from stage III-IV COPD patients decreased body weight in recipient mice [31][129]. Thus, SCFAs are an important part of the immunological axis linking the gut microbiota and the lungs, which has implications in the pathogenesis of COPD (Figure 13).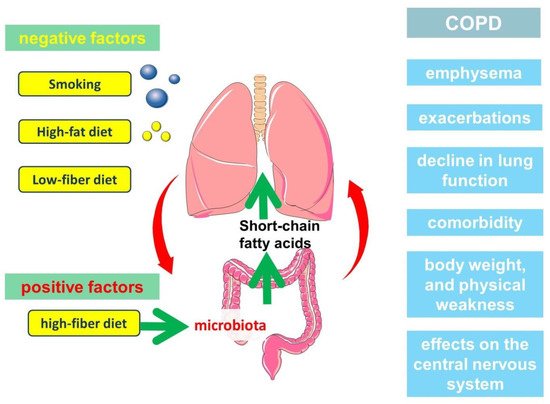
Figure 13.
The participation of short-chain fatty acids in the pathogenesis of the clinically heterogeneous course of COPD.
2.1. Role of Short-Chain Fatty Acids in the Development of Emphysema
Emphysema is an important clinical phenotype of COPD. Numerous studies are devoted to the analysis of pathogenetic mechanisms of its development, among which of interest are the works studying the relationship of emphysema with nutrition. It is important to know about the development of emphysema during prolonged starvation, which was shown in the study of Warsaw ghetto prisoners, as well as observations in patients with anorexia nervosa [32][33][142,143]. These data, reinforced by experimental animal models, confirmed the link between nutrient deficiency and alveolar tissue destruction that leads to emphysema [34][144]. There are various explanations that justify these connections. Interestingly, anorexia nervosa is characterized by a decrease in intestinal microbial diversity, which is associated with the production of SCFAs, including butyrate and propionate [35][36][145,146].
A high-fiber diet has been shown to help prevent the progression of emphysema caused by cigarette smoke exposure. This is because a high-fiber diet changes the composition of the gut microbial community, resulting in increased production of SCFAs (acetate, propionate, and butyrate). SCFAs attenuated the pathological changes associated with the progression of emphysema and influenced the inflammatory response caused by cigarette smoke exposure [37][147]. Mice with emphysema that received fermentable fiber (pectin) were shown to have less inflammation than mice with emphysema that received nonfermentable fiber such as cellulose. This corresponded to lower concentrations of acetate, propionate, and butyrate in the emphysema group compared with the other groups. At the same time, macrophage and neutrophil counts were lower in the high fiber (cellulose and pectin) group than in the emphysema group [37][147]. In addition, inflammatory cytokine levels were lower in the high-fiber (cellulose and pectin) diet. In another study, butyrate was shown to reduce hypoxia-induced accumulation of alveolar (mainly CD68+) and interstitial (CD68+ and CD163+) macrophages in rat lungs [38][148].
The key events leading to emphysema are considered to be interalveolar septal avascularization, which is associated with the apoptosis of endothelial cells and alveolar epithelial cells [39][149]. In this regard, the information about butyrate participation in endothelial cell function is of interest. The anti-inflammatory properties of butyrate are in part related to its effect on the activation of NF-kB and PPARalpha and the associated expression of VCAM-1 and ICAM-1 [38][40][85,148]. In addition, butyrate inhibited the activation of endothelial NRLP3 inflammasome in endothelial cells [41][150]. Butyrate has also been shown to be involved in the inhibition of angiogenesis through HIF-1α as well as through the inhibition of vascular endothelial growth factor (VEGF) and cyclooxygenase-2 (COX-2) [38][42][43][148,151,152]. Butyrate has also been shown to enhance the expression of tight junction proteins in pulmonary microvascular endothelial cells, affecting endothelial barrier function [38][148].
The effects of butyrate in endothelial cells are also related to NO production [44][153]. It has been shown that butyrate and acetate, can improve AngII-induced endothelial dysfunction through increased NO bioavailability [45][154]. The reduction of reactive oxygen species (ROS) levels in the vascular wall and the subsequent prevention of NO inactivation represent a key mechanism through which SCFAs act on endothelial function [45][154]. These findings are of interest given the frequent association of COPD with atherosclerosis.
Thus, the production of SCFAs by the intestinal microbiota may be one possible mechanism in the prevention of emphysema. It was found that a serum peptide-based enteral diet can suppress elastase-induced emphysema in mice by altering SCFAs levels in the cecum [46][155]. Modulation of the gut microbiota by prebiotics and transplantation of fecal microbiota from a high-fiber diet altered the composition of the gut microbiota, attenuating smoking-induced emphysema [47][156]. This was associated with a decrease in local and systemic inflammation through production of SCFAs, which protect against alveolar destruction and cellular apoptosis. The levels of IL-6 and IFN-γ in bronchoalveolar lavage fluid (BALF) were lowest in the high-fiber diet group, and the local concentration of SCFAs was markedly higher in mice with emphysema following fecal microbiota transplantation and the high-fiber diet than in mice with emphysema [47][156]. And the high-fiber diet had a more protective effect against emphysema than the high-protein diet [47][156].
