Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Andrea Piccioni and Version 4 by Camila Xu.
It quickly became obvious that emergency ultrasound, or point of care ultrasound (POCUS), has some very interesting aspects in the context of the emergency room (ER), allowing the physician to immediately obtain images of the patient during the first visit and thus rule out major pathologies immediately. Chest pain often is associated with dyspnea or shortness of breath (SOB), which is in itself one of the most common causes of emergency room access. The origin of these symptoms is often sought in heart and lung diseases.
- POCUS
- point of care ultrasound
- emergency medicine
- ultrasound
1. POCUS in Chest Pain: What Role Could It Have?
Over the last twenty years, ultrasound has gained growing importance in the emergency department. Initially, ultrasounds were usually performed on trauma patients to evaluate whether patients needed surgery when CT (computed tomography) scans were not as widely spread as they are now [1].
It quickly became obvious that emergency ultrasound, or point of care ultrasound (POCUS), has some very interesting aspects in the context of the emergency room (ER), allowing the physician to immediately obtain images of the patient during the first visit and thus rule out major pathologies immediately [2].
Ultrasound has gained popularity in many different conditions and clinical presentations, from critically ill patients [3] to patients with musculoskeletal pain [4].
While on the one hand ultrasound presents a number of advantages, it also presents some potential pitfalls, particularly because it is highly influenced by the operator’s ability to perform it [5].
However, particularly in overcrowded ERs, ultrasound can aid the emergency physician in the diagnosis and stratification of patients.
Chest pain is one of the main causes of admission to the emergency room, and it has been estimated that about 1 million people refer to the ER for this reason in Italy every year. It has been estimated that in about half of the cases the cause is cardiac, yet in the other half it is not [6]. While acute coronary syndrome (ACS) is the first cause that needs to be ruled out, there are a number of other conditions that can present with chest pain [7]. Additionally, the characterization of the pain, which should in theory aid the staff towards the correct diagnosis, is not reliable in a large number of patients due to a number of psychosocial and physiological factors [6].
2. Cardiac Causes
As discussed above, chest pain is the second most frequent cause of accessing the emergency room [7]. In case of suspicion of ischemic chest pain, the patient is evaluated with a 12-lead electrocardiogram and troponin dosage, which are necessary for the diagnosis of ACS [8][9]. In the event of major changes in the ECG (electrocardiogram) or troponin values, the patient is urgently evaluated by the cardiologist. Once the diagnosis of ACS has been ruled out, there are many other cardiac clinical pictures in which the help of ultrasound can be decisive for the emergency room physician. There are, indeed, many other heart diseases that can occur in the emergency room with chest pain, such as aortic dissection, pericarditis, and pulmonary embolism. The use of echocardiography by the emergency physician has several advantages, such as a targeted and early evaluation, and is rapid and non-invasive. However, this method, which has been spreading rapidly for several years, does not yet have a good degree of overall accuracy [9][10]. Another condition in which echocardiography can help the physician is the finding of hypoechoic material between the two layers of the pericardium, which allows reusearchers to make a diagnosis of pericardial effusion (Figure 1). Another advantage is that the ultrasound performed in the emergency room by the emergency doctor has a very high sensitivity (96%) and specificity (98%) towards this pathology [10][14].
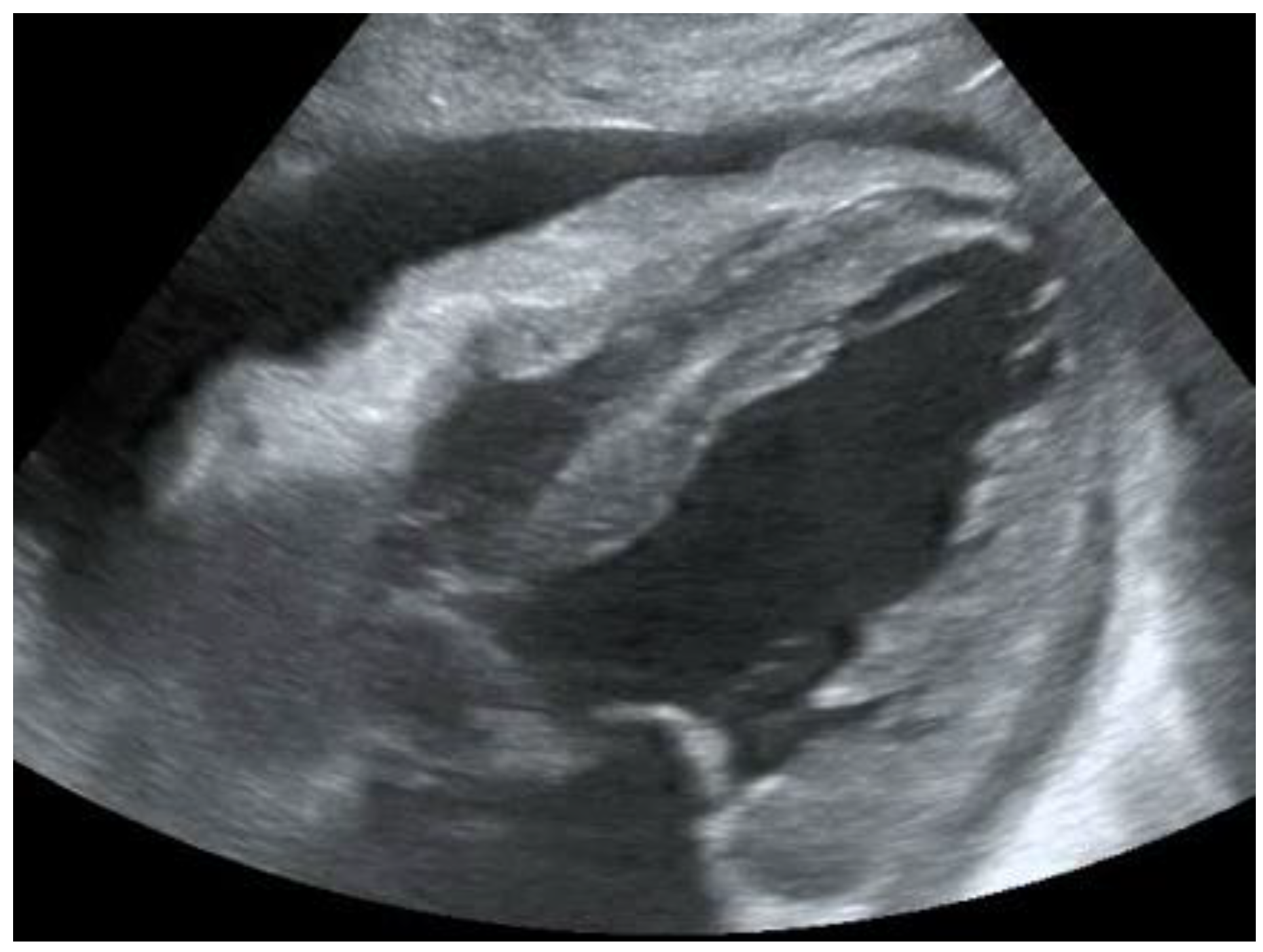
Figure 1. POCUS echocardiography: subcostal projection with pericardial effusion.
POCUS echocardiography: subcostal projection with pericardial effusion.
Figure 2. Subcostal longitudinal view: normal IVC.
Subcostal longitudinal view: normal IVC.
Table 1.
Relation between inferior vena cava diameter, inspiratory collapse and right atrium pressure.
| IVC Diameter | Inspiratory Collapse | Right Atrium Pressure |
|---|---|---|
| <2.1 cm | >50% | 3 mm Hg (range 0–5 mm Hg) |
| >2.1 cm | <50% | 15 mm Hg (range 10–20 mm Hg) |
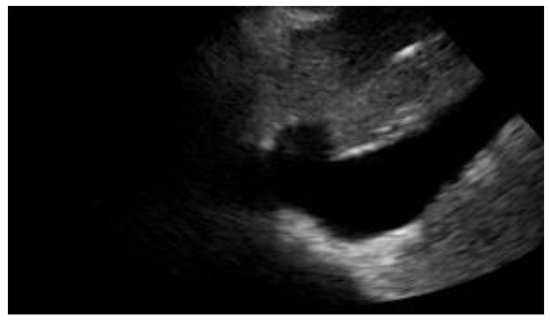
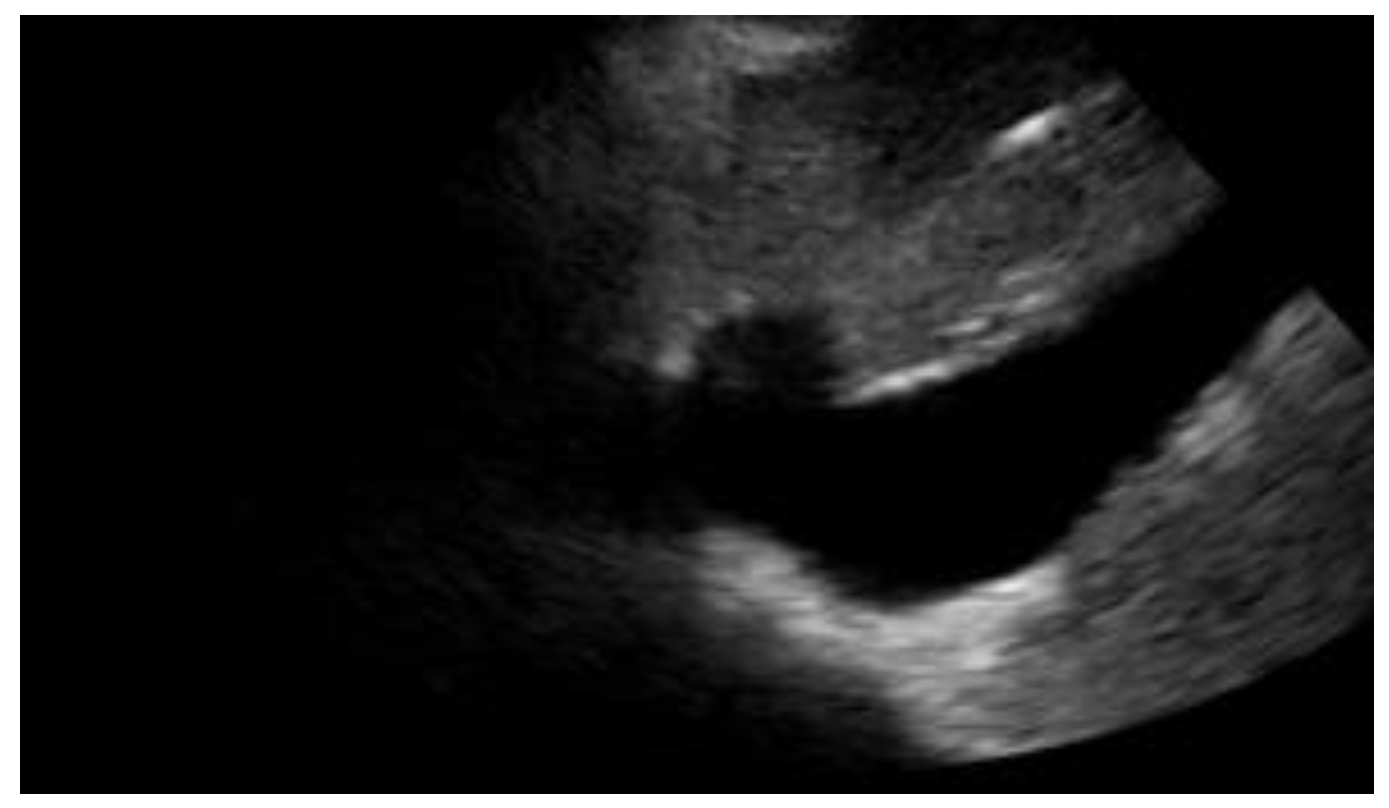
Figure 3. Subcostal longitudinal view: plethoric IVC. This finding suggests a state of fluid overload.
Subcostal longitudinal view: plethoric IVC. This finding suggests a state of fluid overload.
Table 2.
POCUS application in cardiac clinical pictures.
| Uses of Cardiac POCUS in the Emergency Department | |
|---|---|
| Disease | Assessment |
| Pulmonary embolism | Ejection fraction |
| Heart failure | Inferior vena cava filling |
| Aortic pathologies | |
| Pericardial effusion and cardiac tamponade | |
3. Chest Pain and Its Respiratory Causes
Chest pain often is associated with dyspnea or shortness of breath (SOB), which is in itself one of the most common causes of emergency room access. The origin of these symptoms is often sought in heart and lung diseases [21][25]. Patients presenting with these symptoms are routinely subjected to a chest X-ray examination, although in recent years reswearchers have witnessed the rapid growth and spread of thoracic POCUS, in which the physician himself, no longer the radiologist, performs the diagnostic examination. One of the advantages includes knowing first-hand the clinical picture and, consequently, the symptoms reported by the patient. For this reason, it is easier to orientate towards the correct differential diagnosis [22][26]. It has been known for some time now that the application of this method also presents many advantages for the patient when it is applied for the researchtudy of the thorax, including a lower exposure to ionizing radiation, a greater speed of execution, and a reduction in cost [23][27]. One of the most well-established aspects of this approach is that integrating ultrasound into the normal diagnostic tests for patients who come to the emergency room for dyspnoea and chest pain improves diagnostic accuracy [24][28].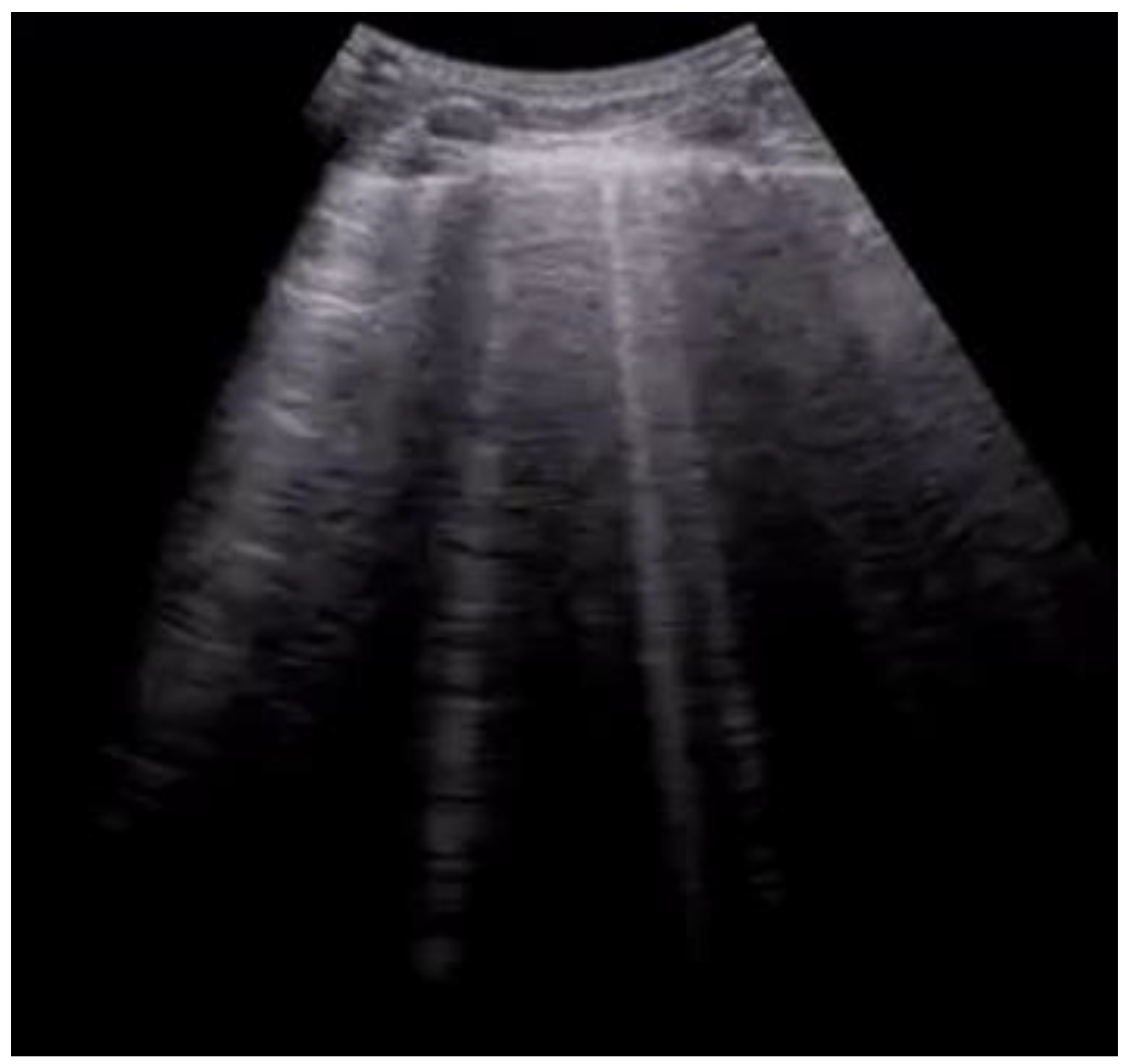
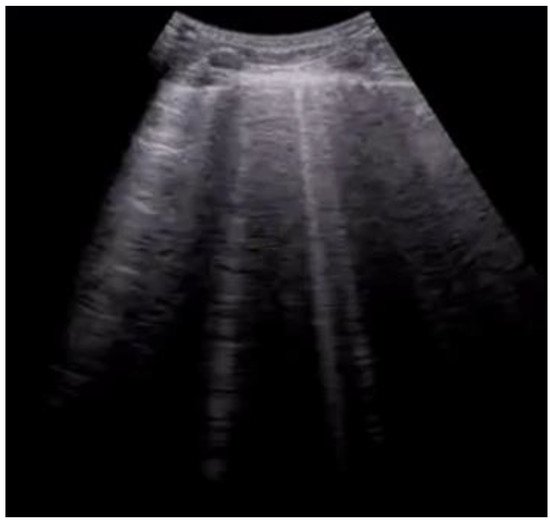
Figure 4. Longitudinal scan with evidence of B-lines: vertical artifacts perpendicular to the pleural line are indicative of inflammation or interstitial edema.
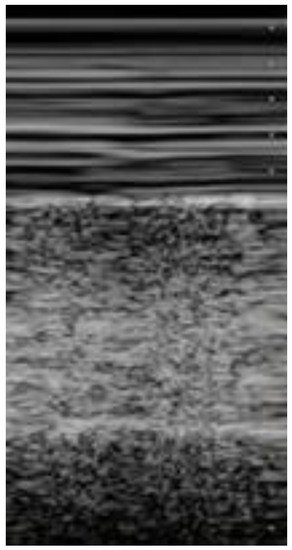
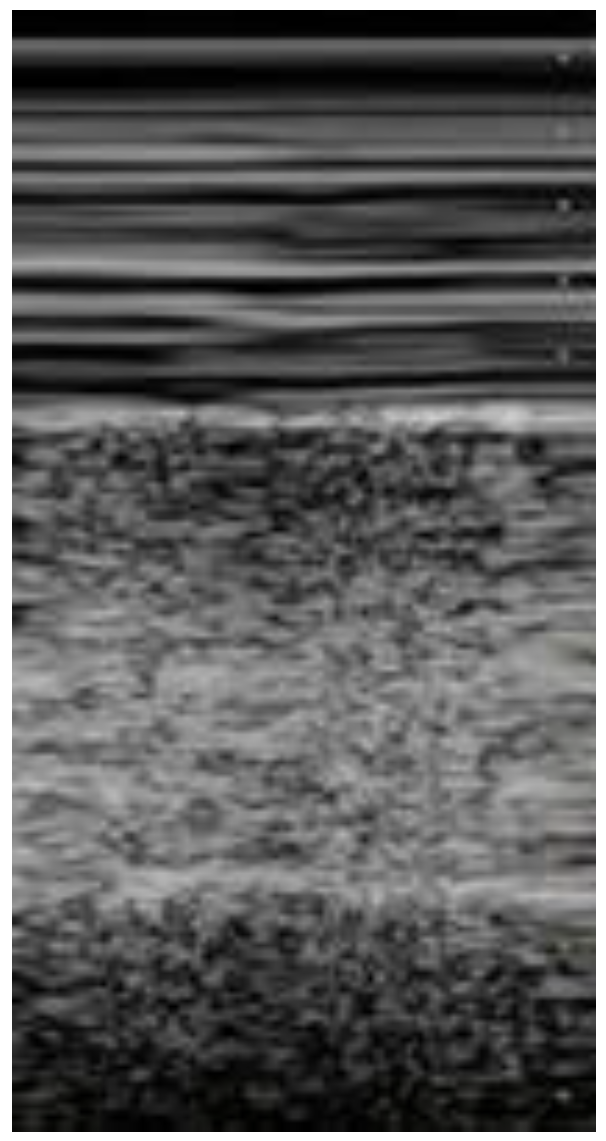
Figure 5. Lung ultrasonography, signs in motion mode (M-mode): seashore sign, indicative of the physiological sliding of the pleural line.
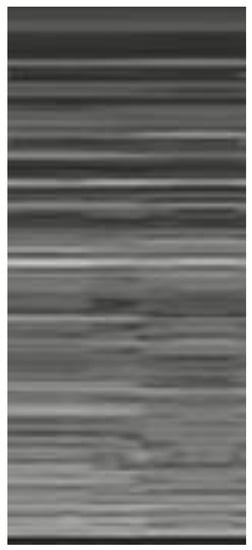
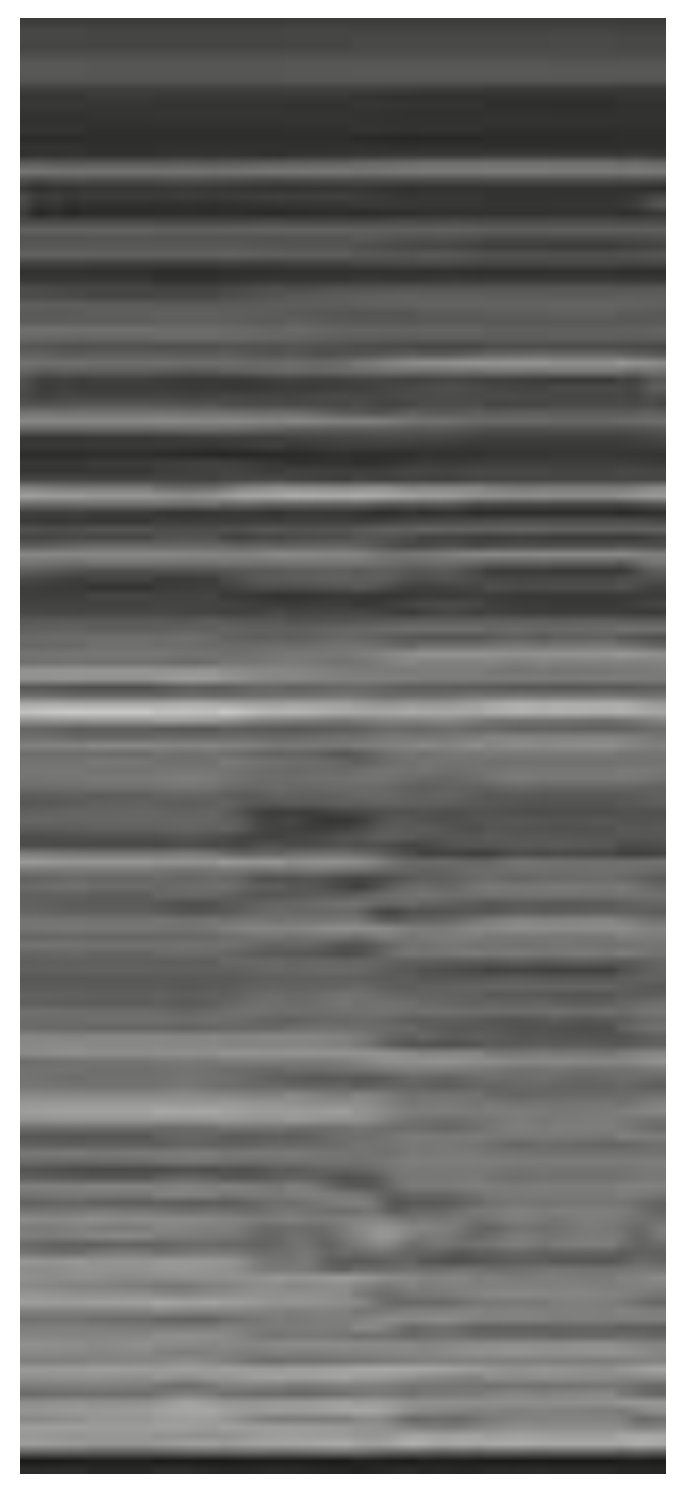
Figure 6. Lung ultrasonography, signs in motion mode (M-mode): barcode sign (sign of the stratosphere), no evidence of pleural sliding, a sign suggestive of pneumothorax.
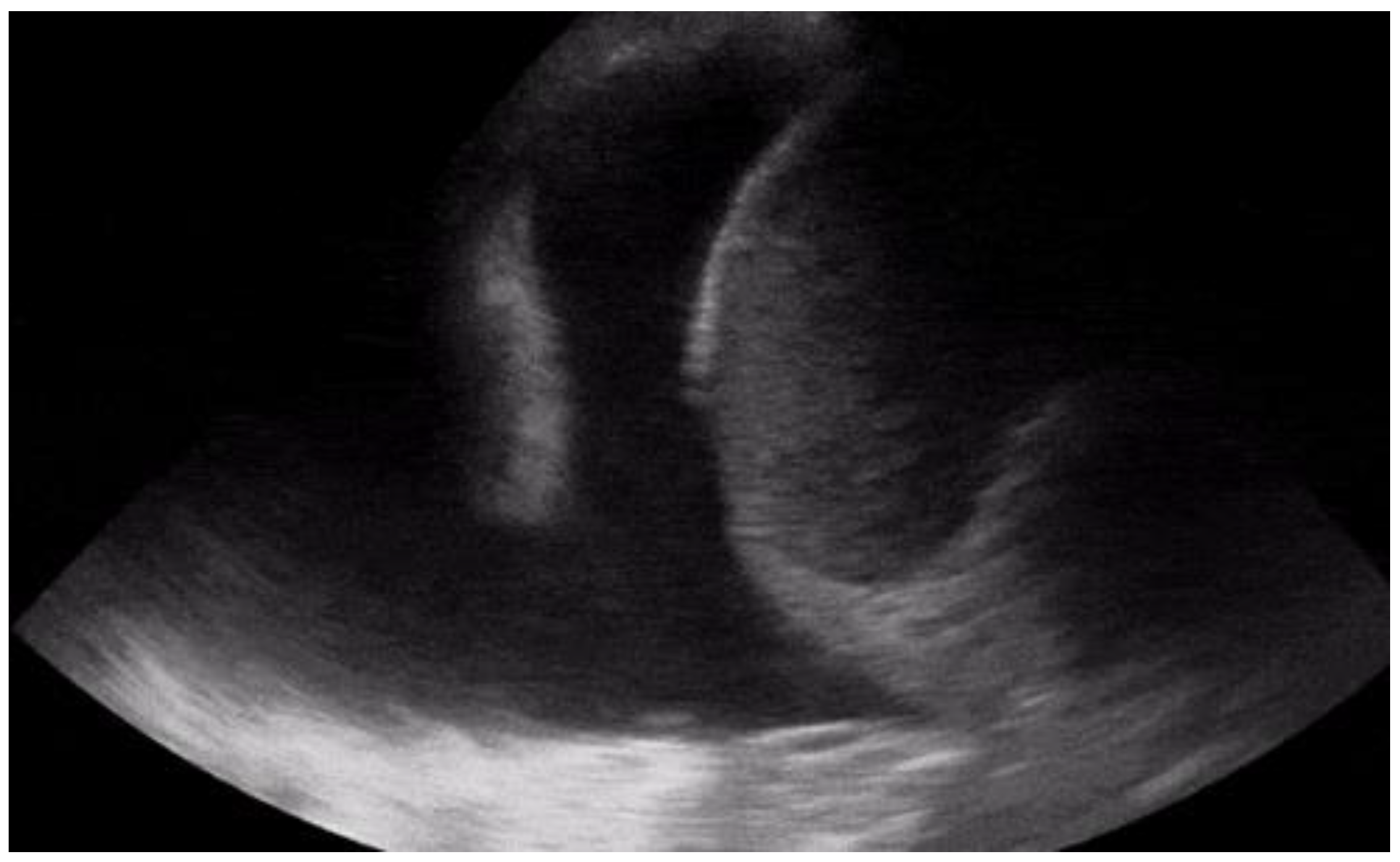

Figure 7. Longitudinal scan with presence of massive pleural effusion above the diaphragmatic line in pleural cavity, with atelectasis of adjacent lung parenchyma.
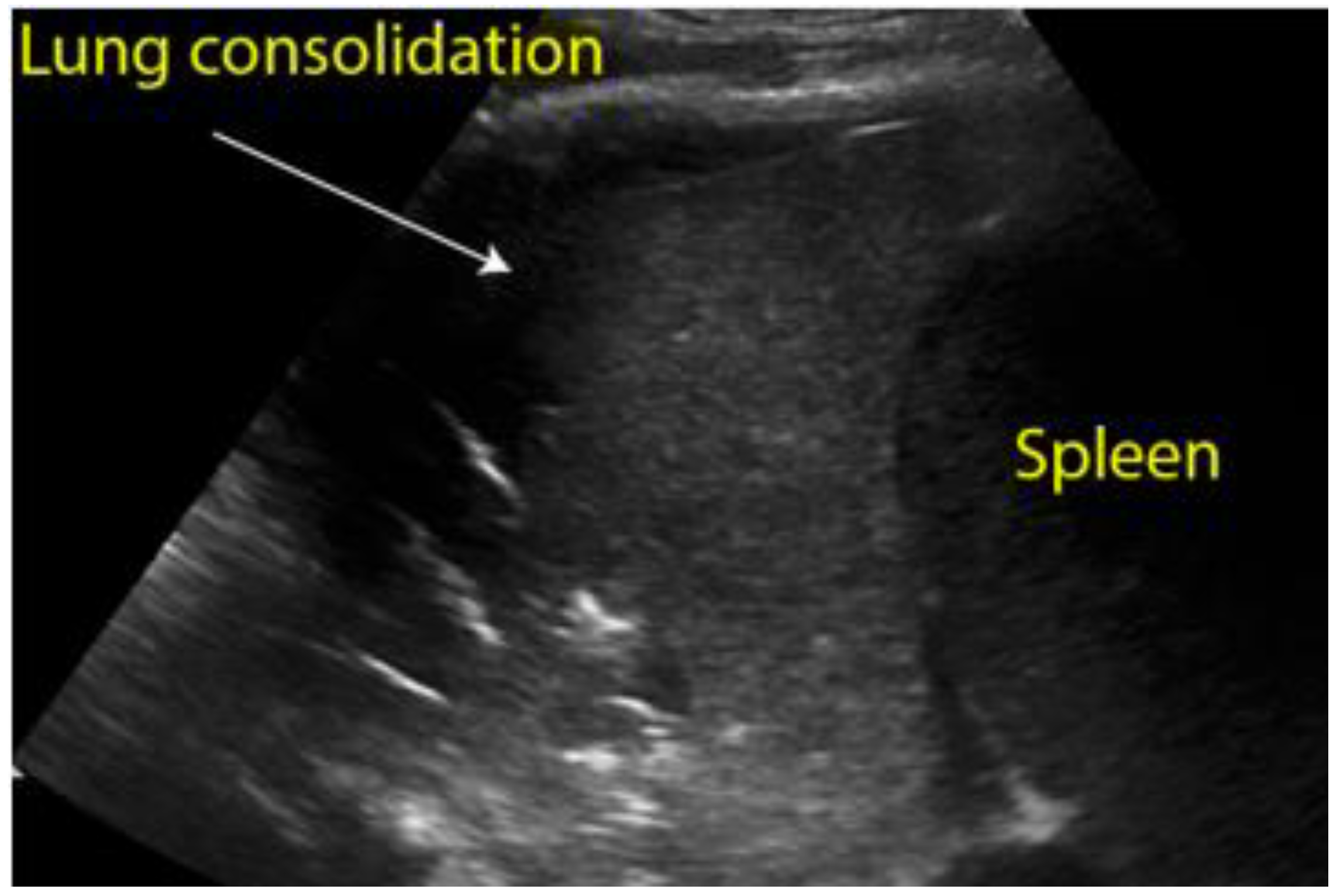
Figure 8. Longitudinal scan of left hypochondrium with presence of lung consolidation suggestive of pneumonia.
Longitudinal scan of left hypochondrium with presence of lung consolidation suggestive of pneumonia.
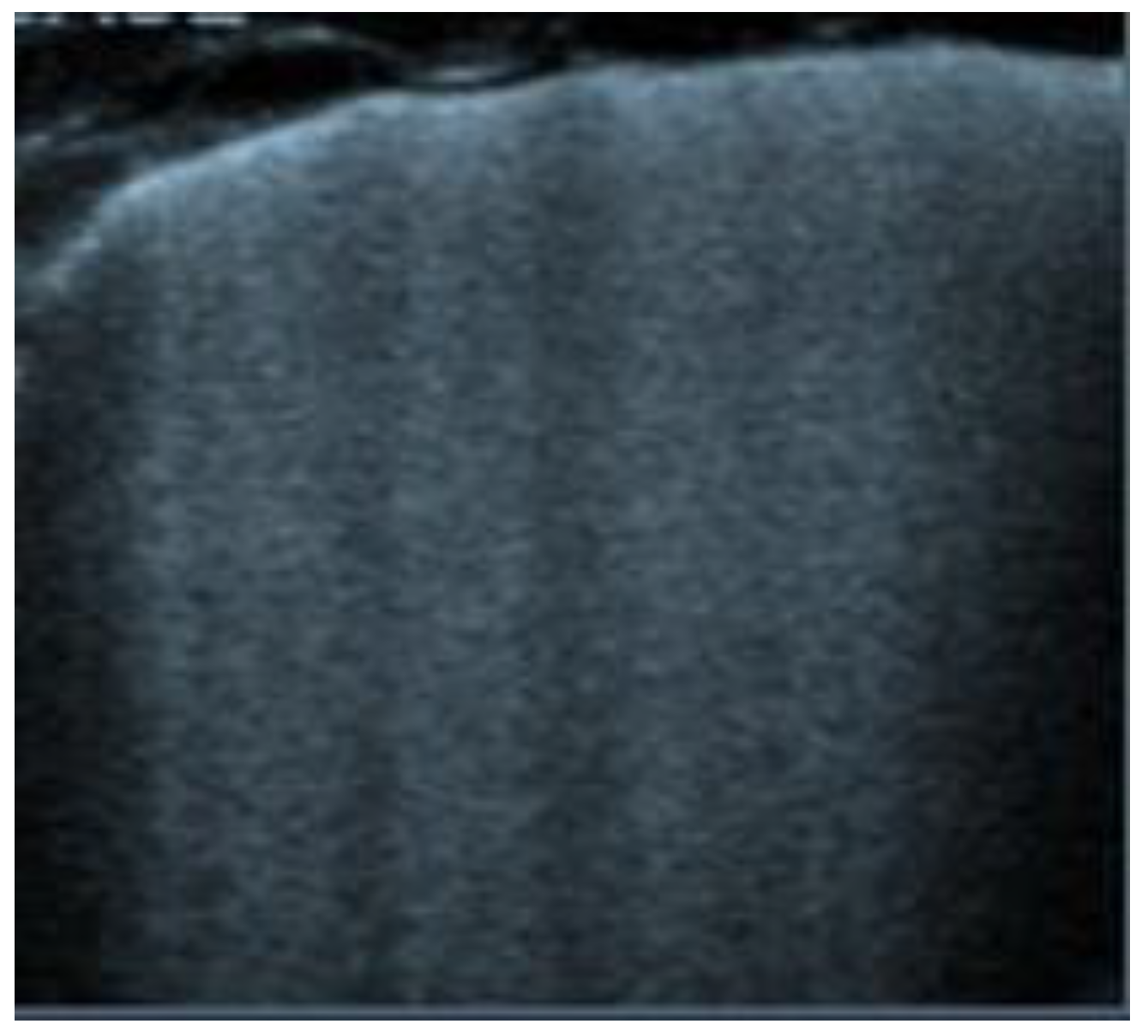
Figure 9. Transverse scan, presence of diffuse B-lines over all fields (white lung) indicative of acute pulmonary edema.
Transverse scan, presence of diffuse B-lines over all fields (white lung) indicative of acute pulmonary edema.
