Ultra-processed foods (UPFs) are products that have undergone a series of industrial processes, including physical, biological, or chemical processes, coupled with the use of additives such as colorings, emulsifiers, and preservatives. UPF consumption has grown dramatically over the last few decades worldwide. This growth is accompanied by the increasing prevalence of non-communicable diseases (NCDs) such as cardiovascular diseases, hypertension, and type 2 diabetes. UPFs represent three main health concerns: (i) they are generally high in non-nutritive compounds such as sugars, sodium, and trans fat and low in nutritional compounds such as proteins and fibers, (ii) they contain different types of additives that may cause severe health issues, and (iii) they are presented in packages made of synthetic materials that may also cause undesirable health side-effects.
- ultra-processed food
- type 2 diabetes
- gestational diabetes
1. Introduction
2. An Overview of Ultra-Processed Foods
Nowadays, almost all available food products are processed; the processing techniques are not the issue. Multiple conventional and other relatively novel processes such as drying, non-alcoholic fermentation, freezing, pasteurization, and vacuum-packing are beneficial for either human health or preserving foods. The issue is with the term “ultra-processed”, which reflects the series of industrial processes that have been undergone [910]. Multiple food classification systems have been designed to characterize foods according to processing criteria. In 2010, Monteiro and colleagues [1011] established a system known as “NOVA”. Since then, it has become the most widely used system in the research field [2][56][1112]. NOVA classifies foods based on the degree and purpose of industrialized processing into four categories (Figure 1): (i) unprocessed/minimally processed foods, (ii) processed culinary ingredients, (iii) processed foods, and (iv) ultra-processed foods [1213]. The latter, ultra-processed foods (UPFs), are products that have been manufactured by different types of industrial processes, including physical, biological, or chemical processes, such as hydrogenation, extrusion, and pre-frying, coupled with the use of “cosmetic additives” such as colorings, flavorings, sweeteners, and emulsifiers [45][56][67]. Cosmetic additives are low-cost ingredients that have rarely or never been used in kitchens. The presence of at least one cosmetic additive in any product’s ingredients list, which by law must be included in food labels, identifies it as ultra-processed [1213]. These additives are applied in the food industry to provide long-shelf-life products that are more convenient, hyper-palatable, and affordable to consumers with the least economic costs and maximum profit [3][56].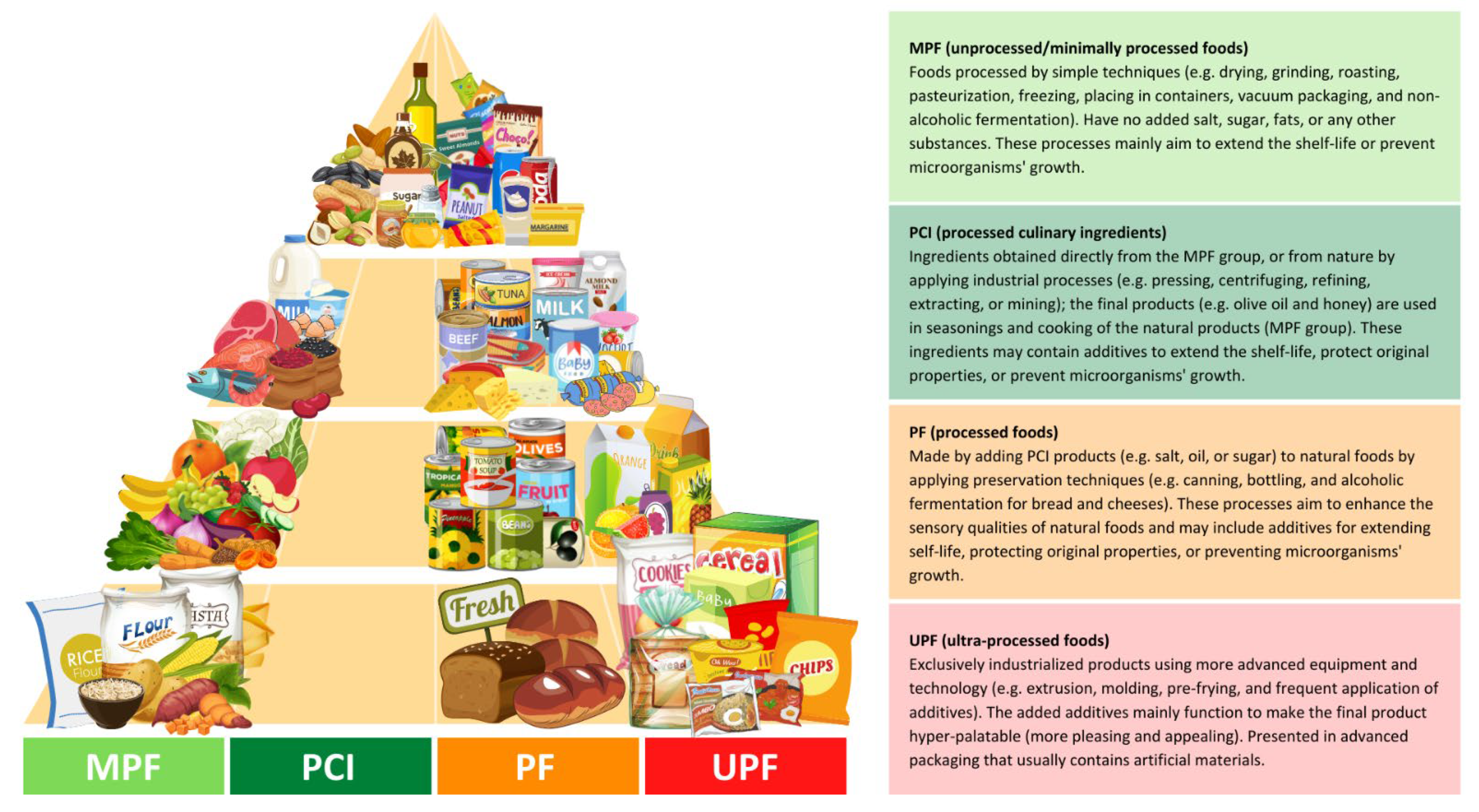
3. Ultra-Processed Foods and Health Outcomes
Concerns surrounding UPFs have attracted researchers’ interest all over the world; several studies in different populations and settings have found an association between elevated intake of UPFs and all-cause mortality and many other different specific health outcomes such as cardiovascular disease, hypertension, overall cancer, depression, metabolic syndrome, overweight and obesity, and gestational obesity [45]. The risk of all-cause mortality has been reported to increase by 62% with the high UPF consumption; with each additional serving of UPF products, the risk increased by 18% [1617]. An increased risk of cardiovascular disease by 11% [2526] and overall cancer by 10% [2627] has been reported with each 10% increase in UPF intake. The results remained significant even after further adjustment of several nutritional quality markers. Among adult individuals followed up for a median of 10.3 years, higher UPF consumption was reported to increase the risk of developing depression by 31% [2728]. The risk of developing metabolic syndrome has significantly increased by 28%, with high UPF consumption contributing to an average of ≥71% of TEI [1516]. Results showed a statistically significant association between high UPF consumption, elevated waist circumference, and reduced high-density lipoprotein (HDL) cholesterol levels. An increase in the risk of obesity by 31% was reported, with an average UPF consumption contributing to 73% of TEI [2829]. A recent systematic review reported that high UPF consumption correlates linearly with elevated body mass index (BMI) [78]. Several studies had reported similar significant results [1617][1718][2930]; elevated BMI levels were observed among individuals consuming a high level of UPF. Obesity, as well established for decades, is a major leading cause of the development of T2D [3031]. Indeed, higher BMI levels above 29 kg/m2 were linked to the development of T2D by 10 times more than normal levels [3031]. Higher UPF consumption can also increase fasting blood glucose, insulin, and the homeostatic model assessment for insulin resistance (Homa-IR).4. Ultra-Processed Foods and Risk of Diabetes
Regardless of the strong evidence between high consumption of UPF and obesity that has been mentioned in the above section, multiple investigational studies have assessed the association between UPF and the incidence of diabetes, especially T2D, and a few other studies investigated the association with gestational diabetes (Table 1).|
Study Design/Follow-Up/ |
UPF Intake Assessment |
Main Results |
References |
|---|---|---|---|
|
Participant Characteristics |
|||
|
Cross-sectional/- n = 13,608 adults (age ≥ 19 years) Diabetic (7%) (50% women) |
24 h recalls/NOVA/ proportion of TEI |
↑ DM risk by 37% (with high vs. low intake, 73% vs. 24% of TEI) An absolute 10% increase in UPF intake increases the risk by 6% (p < 0.05) |
(2021, Canada) |
|
Prospective cohort/6 years n = 104,707 adults (age ≥ 18 years) Non-diabetic (79.2% women) |
24 h recalls/NOVA/ proportion of weight |
An absolute 10% increase in UPF intake was associated with 15% higher risk of T2D (p = 0.001) |
(2020, France) |
|
Prospective cohort/5.4 years n = 21,730 adults (age 40–69 years) Non-diabetic (52.9% women) |
24 h recalls/NOVA/ proportion of weight |
↑ T2D risk by 44% (with high vs. low intake, 41.9% vs. 7.7% of diet proportion) (p < 0.028) |
(2020, UK) |
|
Prospective cohort/12 years n = 20,060 adults (age ≥ 18 years) Non-diabetic (61.5% women) |
FFQ/NOVA/ proportion of weight |
↑ T2D risk by 53% (with high vs. low intake, >323.3 vs. <214.6 g/day of diet proportion) (p = 0.024) |
(2021, Spain) |
|
Prospective cohort/41 months n = 70,421 adults (age 35–70 years) Non-diabetic at baseline (58.6% women) |
FFQ/NOVA/ proportion of weight |
↑ T2D risk by 80% (with high vs. low intake, 48.7% vs. 23.7% of diet proportion) An absolute 10% increase in UPF intake increases the risk by 25% (p < 0.001) |
(2020, The Netherlands) |
|
Cross-sectional/- n = 785 pregnant women (age ≥ 20 years) Non-diabetic at baseline |
24 h recalls/*/ proportion of TEI |
↑ gestational obesity risk by 3 times (with high vs. low intake, 47% vs. 18% of TEI) (p < 0.05) No association with GDM (p > 0.05) |
(2019, Brazil) |
|
Prospective cohort/7.2 years n = 3730 pregnant women (age 18–49 years) Non-diabetic |
FFQ/NOVA/ proportion of weight |
↑ GDM risk by 10% (with high vs. low intake, >4.5 vs. <3.3 serving/day)(p = 0.818) women aged ≥30 years had a doubled risk (p = 0.041) |
(2021, Spain) |
|
Cohort/- n = 42 pregnant women (age ≥ 20 years) pre-gestational diabetics |
FFQ/NOVA/ proportion of TEI |
Each 1 kcal from UPF in the 3rd trimester (mean intake, 15.2% of TEI): ↑ 1-h PPG level by 0.143 (p = 0.011) ↑ HbA1c by 0.007% (p = 0.025) ↑ gestational weight by 0.11 kg (p = 0.006) |
(2021, Brazil) |
Abbreviations: UPF: Ultra-processed foods; FFQ: Food frequently questionnaires; TEI: Total energy intake; DM: Diabetes mellitus; T2D: Type 2 diabetes; GDM: Gestational diabetes mellitus; PPG: Postprandial glucose; HbA1c: glycosylated hemoglobin; (↑): Increased. *Classified based on the 2014 Guia Alimentar para a População Brasileira; see Louzada et al. [3839] for the detailed method.
References
- Marino, M.; Puppo, F.; Del Bo’, C.; Vinelli, V.; Riso, P.; Porrini, M.; Martini, D. A systematic review of worldwide consumption of ultra-processed foods: Findings and criticisms. Nutrients 2021, 13, 2778.
- Baker, P.; Machado, P.; Santos, T.; Sievert, K.; Backholer, K.; Hadjikakou, M.; Russell, C.; Huse, O.; Bell, C.; Scrinis, G. Ultra-processed foods and the nutrition transition: Global, regional and national trends, food systems transformations and political economy drivers. Obes. Rev. 2020, 21, e13126.
- Popkin, B.M.; Ng, S.W. The nutrition transition to a stage of high obesity and noncommunicable disease prevalence dominated by ultra-processed foods is not inevitable. Obes. Rev. 2022, 23, e13366.
- Chen, X.; Zhang, Z.; Yang, H.; Qiu, P.; Wang, H.; Wang, F.; Zhao, Q.; Fang, J.; Nie, J. Consumption of ultra-processed foods and health outcomes: A systematic review of epidemiological studies. Nutr. J. 2020, 19, 86. Aguiree, F.; Brown, A.; Cho, N.H.; Dahlquist, G.; Dodd, S.; Dunning, T.; Hirst, M.; Hwang, C.; Magliano, D.; Patterson, C.; et al. IDF Diabetes Atlas; International Diabetes Federation: Basel, Switzerland, 2021; Volume 102, pp. 147–148.
- Matos, R.A.; Adams, M.; Sabaté, J. Review: The Consumption of Ultra-Processed Foods and Non-communicable Diseases in Latin America. Front. Nutr. 2021, 8, 622714. Chen, X.; Zhang, Z.; Yang, H.; Qiu, P.; Wang, H.; Wang, F.; Zhao, Q.; Fang, J.; Nie, J. Consumption of ultra-processed foods and health outcomes: A systematic review of epidemiological studies. Nutr. J. 2020, 19, 86.
- Schulze, K.; Adams, J.; White, M. Associations Between Sales of Ultra-Processed Food Products and Prevalence of Adiposity and Diabetes Mellitus: A Panel Analysis of 76 Countries Between 2001–2016. SSRN Elect. J. 2019. Matos, R.A.; Adams, M.; Sabaté, J. Review: The Consumption of Ultra-Processed Foods and Non-communicable Diseases in Latin America. Front. Nutr. 2021, 8, 622714.
- De Araújo, T.P.; de Moraes, M.M.; Magalhães, V.; Afonso, C.; Santos, C.; Rodrigues, S.S.P. Ultra-Processed Food Availability and Noncommunicable Diseases: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 7382. Schulze, K.; Adams, J.; White, M. Associations Between Sales of Ultra-Processed Food Products and Prevalence of Adiposity and Diabetes Mellitus: A Panel Analysis of 76 Countries Between 2001–2016. SSRN Elect. J. 2019.
- Martini, D.; Godos, J.; Bonaccio, M.; Vitaglione, P.; Grosso, G. Ultra-Processed Foods and Nutritional Dietary Profile: A Meta-Analysis of Nationally Representative Samples. Nutrients 2021, 13, 3390. De Araújo, T.P.; de Moraes, M.M.; Magalhães, V.; Afonso, C.; Santos, C.; Rodrigues, S.S.P. Ultra-Processed Food Availability and Noncommunicable Diseases: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 7382.
- Monteiro, C.A.; Cannon, G.; Lawrence, M.; Louzada, M.L.C.; Machado, P.P. Ultra-Processed Foods, Diet Quality, and Health Using the NOVA Classification System; Food and Agriculture Organization of the United Nations: Rome, Italy, 2019; pp. 6–9. Martini, D.; Godos, J.; Bonaccio, M.; Vitaglione, P.; Grosso, G. Ultra-Processed Foods and Nutritional Dietary Profile: A Meta-Analysis of Nationally Representative Samples. Nutrients 2021, 13, 3390.
- Monteiro, C.A.; Levy, R.B.; Claro, R.M.; de Castro, I.R.R.; Cannon, G. A new classification of foods based on the extent and purpose of their processing. Cad. Saude Publica 2010, 26, 2039–2049. Monteiro, C.A.; Cannon, G.; Lawrence, M.; Louzada, M.L.C.; Machado, P.P. Ultra-Processed Foods, Diet Quality, and Health Using the NOVA Classification System; Food and Agriculture Organization of the United Nations: Rome, Italy, 2019; pp. 6–9.
- Dicken, S.J.; Batterham, R.L. The Role of Diet Quality in Mediating the Association between Ultra-Processed Food Intake, Obesity and Health-Related Outcomes: A Review of Prospective Cohort Studies. Nutrients 2021, 14, 23. Monteiro, C.A.; Levy, R.B.; Claro, R.M.; de Castro, I.R.R.; Cannon, G. A new classification of foods based on the extent and purpose of their processing. Cad. Saude Publica 2010, 26, 2039–2049.
- Monteiro, C.A.; Cannon, G.; Levy, R.B.; Moubarac, J.C.; Louzada, M.L.C.; Rauber, F.; Khandpur, N.; Cediel, G.; Neri, D.; Martinez-Steele, E.; et al. Ultra-processed foods: What they are and how to identify them. Public Health Nutr. 2019, 22, 936–941. Dicken, S.J.; Batterham, R.L. The Role of Diet Quality in Mediating the Association between Ultra-Processed Food Intake, Obesity and Health-Related Outcomes: A Review of Prospective Cohort Studies. Nutrients 2021, 14, 23.
- Machado, P.P.; Steele, E.M.; Levy, R.B.; Sui, Z.; Rangan, A.; Woods, J.; Gill, T.; Scrinis, G.; Monteiro, C.A. Ultra-processed foods and recommended intake levels of nutrients linked to non-communicable diseases in Australia: Evidence from a nationally representative cross-sectional study. BMJ 2019, 9, 29544. Monteiro, C.A.; Cannon, G.; Levy, R.B.; Moubarac, J.C.; Louzada, M.L.C.; Rauber, F.; Khandpur, N.; Cediel, G.; Neri, D.; Martinez-Steele, E.; et al. Ultra-processed foods: What they are and how to identify them. Public Health Nutr. 2019, 22, 936–941.
- Rauber, F.; da Costa Louzada, M.L.; Steele, E.; Millett, C.; Monteiro, C.A.; Levy, R.B. Ultra-Processed Food Consumption and Chronic Non-Communicable Diseases-Related Dietary Nutrient Profile in the UK (2008–2014). Nutrients 2018, 10, 587. Machado, P.P.; Steele, E.M.; Levy, R.B.; Sui, Z.; Rangan, A.; Woods, J.; Gill, T.; Scrinis, G.; Monteiro, C.A. Ultra-processed foods and recommended intake levels of nutrients linked to non-communicable diseases in Australia: Evidence from a nationally representative cross-sectional study. BMJ 2019, 9, 29544.
- Steele, E.M.; Juul, F.; Neri, D.; Rauber, F.; Monteiro, C.A. Dietary share of ultra-processed foods and metabolic syndrome in the US adult population. Prev. Med. 2019, 125, 40–48. Rauber, F.; da Costa Louzada, M.L.; Steele, E.; Millett, C.; Monteiro, C.A.; Levy, R.B. Ultra-Processed Food Consumption and Chronic Non-Communicable Diseases-Related Dietary Nutrient Profile in the UK (2008–2014). Nutrients 2018, 10, 587.
- Rico-Campà, A.; Martínez-González, M.A.; Alvarez-Alvarez, I.; De Deus Mendonça, R.; De La Fuente-Arrillaga, C.; Gómez-Donoso, C.; Bes-Rastrollo, M. Association between consumption of ultra-processed foods and all cause mortality: SUN prospective cohort study. BMJ 2019, 365, l1949. Steele, E.M.; Juul, F.; Neri, D.; Rauber, F.; Monteiro, C.A. Dietary share of ultra-processed foods and metabolic syndrome in the US adult population. Prev. Med. 2019, 125, 40–48.
- Schnabel, L.; Kesse-Guyot, E.; Allès, B.; Touvier, M.; Srour, B.; Hercberg, S.; Buscail, C.; Julia, C. Association Between Ultraprocessed Food Consumption and Risk of Mortality Among Middle-aged Adults in France. JAMA Intern. Med. 2019, 179, 490–498. Rico-Campà, A.; Martínez-González, M.A.; Alvarez-Alvarez, I.; De Deus Mendonça, R.; De La Fuente-Arrillaga, C.; Gómez-Donoso, C.; Bes-Rastrollo, M. Association between consumption of ultra-processed foods and all cause mortality: SUN prospective cohort study. BMJ 2019, 365, l1949.
- Kazmi, Z.; Fatima, I.; Perveen, S.; Malik, S.S. Monosodium glutamate: Review on clinical reports. Int. J. Food Prop. 2017, 20, 1807–1815. Schnabel, L.; Kesse-Guyot, E.; Allès, B.; Touvier, M.; Srour, B.; Hercberg, S.; Buscail, C.; Julia, C. Association Between Ultraprocessed Food Consumption and Risk of Mortality Among Middle-aged Adults in France. JAMA Intern. Med. 2019, 179, 490–498.
- Singh, K.; Ahluwalia, P. Effect of monosodium glutamate on lipid peroxidation and certain antioxidant enzymes in cardiac tissue of alcoholic adult male mice. J. Cardiovasc. Dis. Res. 2012, 3, 12–18. Kazmi, Z.; Fatima, I.; Perveen, S.; Malik, S.S. Monosodium glutamate: Review on clinical reports. Int. J. Food Prop. 2017, 20, 1807–1815.
- Shukry, M.; El-Shehawi, A.M.; El-Kholy, W.M.; Elsisy, R.A.; Hamoda, H.S.; Tohamy, H.G.; Abumandour, M.M.; Farrag, F.A. Ameliorative Effect of Graviola (Annona muricata) on Mono Sodium Glutamate-Induced Hepatic Injury in Rats: Antioxidant, Apoptotic, Anti-inflammatory, Lipogenesis Markers, and Histopathological Studies. Animals 2020, 10, 1996. Singh, K.; Ahluwalia, P. Effect of monosodium glutamate on lipid peroxidation and certain antioxidant enzymes in cardiac tissue of alcoholic adult male mice. J. Cardiovasc. Dis. Res. 2012, 3, 12–18.
- Ogbuagu, E.O.; Airaodion, A.I.; Okoroukwu, V.N. Hyperglycemic and hypocholesterolemic effect of monosodium glutamate in Wistar rats. Int. J. Res. Rept. Hematol. 2019, 2, 1–7. Shukry, M.; El-Shehawi, A.M.; El-Kholy, W.M.; Elsisy, R.A.; Hamoda, H.S.; Tohamy, H.G.; Abumandour, M.M.; Farrag, F.A. Ameliorative Effect of Graviola (Annona muricata) on Mono Sodium Glutamate-Induced Hepatic Injury in Rats: Antioxidant, Apoptotic, Anti-inflammatory, Lipogenesis Markers, and Histopathological Studies. Animals 2020, 10, 1996.
- Bhattacharyya, S.; O-Sullivan, I.; Katyal, S.; Unterman, T.; Tobacman, J.K. Exposure to the common food additive carrageenan leads to glucose intolerance, insulin resistance and inhibition of insulin signalling in HepG2 cells and C57BL/6J mice. Diabetologia 2012, 55, 194–203. Ogbuagu, E.O.; Airaodion, A.I.; Okoroukwu, V.N. Hyperglycemic and hypocholesterolemic effect of monosodium glutamate in Wistar rats. Int. J. Res. Rept. Hematol. 2019, 2, 1–7.
- Pepino, M.Y.; Tiemann, C.D.; Patterson, B.W.; Wice, B.M.; Klein, S. Sucralose affects glycemic and hormonal responses to an oral glucose load. Diabetes Care 2013, 36, 2530–2535. Bhattacharyya, S.; O-Sullivan, I.; Katyal, S.; Unterman, T.; Tobacman, J.K. Exposure to the common food additive carrageenan leads to glucose intolerance, insulin resistance and inhibition of insulin signalling in HepG2 cells and C57BL/6J mice. Diabetologia 2012, 55, 194–203.
- Pagliai, G.; Dinu, M.; Madarena, M.P.; Bonaccio, M.; Iacoviello, L.; Sofi, F. Consumption of ultra-processed foods and health status: A systematic review and meta-Analysis. Br. J. Nutr. 2021, 125, 308–318. Pepino, M.Y.; Tiemann, C.D.; Patterson, B.W.; Wice, B.M.; Klein, S. Sucralose affects glycemic and hormonal responses to an oral glucose load. Diabetes Care 2013, 36, 2530–2535.
- Srour, B.; Fezeu, L.K.; Kesse-Guyot, E.; Allès, B.; Méjean, C.; Andrianasolo, R.M.; Chazelas, E.; Deschasaux, M.; Hercberg, S.; Galan, P.; et al. Ultra-processed food intake and risk of cardiovascular disease: Prospective cohort study (NutriNet-Santé). BMJ 2019, 365, l1451. Pagliai, G.; Dinu, M.; Madarena, M.P.; Bonaccio, M.; Iacoviello, L.; Sofi, F. Consumption of ultra-processed foods and health status: A systematic review and meta-Analysis. Br. J. Nutr. 2021, 125, 308–318.
- Fiolet, T.; Srour, B.; Sellem, L.; Kesse-Guyot, E.; Allès, B.; Méjean, C.; Deschasaux, M.; Fassier, P.; Latino-Martel, P.; Beslay, M.; et al. Consumption of ultra-processed foods and cancer risk: Results from NutriNet-Santé prospective cohort. BMJ 2018, 360, k322. Srour, B.; Fezeu, L.K.; Kesse-Guyot, E.; Allès, B.; Méjean, C.; Andrianasolo, R.M.; Chazelas, E.; Deschasaux, M.; Hercberg, S.; Galan, P.; et al. Ultra-processed food intake and risk of cardiovascular disease: Prospective cohort study (NutriNet-Santé). BMJ 2019, 365, l1451.
- Gómez-Donoso, C.; Sánchez-Villegas, A.; Martínez-González, M.A.; Gea, A.; de Deus Mendonça, R.; Lahortiga-Ramos, F.; Bes-Rastrollo, M. Ultra-processed food consumption and the incidence of depression in a Mediterranean cohort: The SUN Project. Eur. J. Nutr. 2020, 59, 1093–1103. Fiolet, T.; Srour, B.; Sellem, L.; Kesse-Guyot, E.; Allès, B.; Méjean, C.; Deschasaux, M.; Fassier, P.; Latino-Martel, P.; Beslay, M.; et al. Consumption of ultra-processed foods and cancer risk: Results from NutriNet-Santé prospective cohort. BMJ 2018, 360, k322.
- Nardocci, M.; Polsky, J.Y.; Moubarac, J.-C. Consumption of ultra-processed foods is associated with obesity, diabetes and hypertension in Canadian adults. Can. J. Public Health 2021, 112, 421–429. Gómez-Donoso, C.; Sánchez-Villegas, A.; Martínez-González, M.A.; Gea, A.; de Deus Mendonça, R.; Lahortiga-Ramos, F.; Bes-Rastrollo, M. Ultra-processed food consumption and the incidence of depression in a Mediterranean cohort: The SUN Project. Eur. J. Nutr. 2020, 59, 1093–1103.
- Beslay, M.; Srour, B.; Méjean, C.; Allès, B.; Fiolet, T.; Debras, C.; Chazelas, E.; Deschasaux, M.; Wendeu-Foyet, M.G.; Hercberg, S.; et al. Ultra-processed food intake in association with BMI change and risk of overweight and obesity: A prospective analysis of the French NutriNet-Santé cohort. PLoS Med. 2020, 17, e1003256. Nardocci, M.; Polsky, J.Y.; Moubarac, J.-C. Consumption of ultra-processed foods is associated with obesity, diabetes and hypertension in Canadian adults. Can. J. Public Health 2021, 112, 421–429.
- Maggio, C.A.; Pi-Sunyer, F.X. Obesity and type 2 diabetes. Endocrinol. Metab. Clin. 2003, 32, 805–822. Beslay, M.; Srour, B.; Méjean, C.; Allès, B.; Fiolet, T.; Debras, C.; Chazelas, E.; Deschasaux, M.; Wendeu-Foyet, M.G.; Hercberg, S.; et al. Ultra-processed food intake in association with BMI change and risk of overweight and obesity: A prospective analysis of the French NutriNet-Santé cohort. PLoS Med. 2020, 17, e1003256.
- Srour, B.; Léopold, K.F.; Kesse-Guyot, E.; Allès, B.; Debras, C.; Druesne-Pecollo, N.; Chazelas, E.; Deschasaux, M.; Hercberg, S.; Galan, P.; et al. Ultraprocessed Food Consumption and Risk of Type 2 Diabetes Among Participants of the NutriNet-Santé Prospective Cohort. JAMA Intern. Med. 2020, 180, 283–291. Maggio, C.A.; Pi-Sunyer, F.X. Obesity and type 2 diabetes. Endocrinol. Metab. Clin. 2003, 32, 805–822.
- Levy, R.B.; Rauber, F.; Chang, K.; da Costa Louzada, M.L.; Monteiro, C.A.; Millett, C.; Vamos, E.P. Ultra-processed food consumption and type 2 diabetes incidence: A prospective cohort study. Clin. Nutr. 2020, 40, 3608–3614. Srour, B.; Léopold, K.F.; Kesse-Guyot, E.; Allès, B.; Debras, C.; Druesne-Pecollo, N.; Chazelas, E.; Deschasaux, M.; Hercberg, S.; Galan, P.; et al. Ultraprocessed Food Consumption and Risk of Type 2 Diabetes Among Participants of the NutriNet-Santé Prospective Cohort. JAMA Intern. Med. 2020, 180, 283–291.
- Llavero-Valero, M.; Escalada-San Martín, J.; Martínez-González, M.A.; Basterra-Gortari, F.J.; de la Fuente-Arrillaga, C.; Bes-Rastrollo, M. Ultra-processed foods and type-2 diabetes risk in the SUN project: A prospective cohort study. Clin. Nutr. 2021, 40, 2817–2824. Levy, R.B.; Rauber, F.; Chang, K.; da Costa Louzada, M.L.; Monteiro, C.A.; Millett, C.; Vamos, E.P. Ultra-processed food consumption and type 2 diabetes incidence: A prospective cohort study. Clin. Nutr. 2020, 40, 3608–3614.
- Duan, M.-J.; Vinke, P.C.; Navis, G.; Corpeleijn, E.; Dekker, L.H. Ultra-processed food and incident type 2 diabetes: Studying the underlying consumption patterns to unravel the health effects of this heterogeneous food category in the prospective Lifelines cohort. BMC Med. 2022, 20, 7. Llavero-Valero, M.; Escalada-San Martín, J.; Martínez-González, M.A.; Basterra-Gortari, F.J.; de la Fuente-Arrillaga, C.; Bes-Rastrollo, M. Ultra-processed foods and type-2 diabetes risk in the SUN project: A prospective cohort study. Clin. Nutr. 2021, 40, 2817–2824.
- Sartorelli, D.S.; Crivellenti, L.C.; Zuccolotto, D.C.C.; Franco, L.J. Relationship between minimally and ultra-processed food intake during pregnancy with obesity and gestational diabetes mellitus. Cad. Saude. Publica 2019, 35, e00049318. Duan, M.-J.; Vinke, P.C.; Navis, G.; Corpeleijn, E.; Dekker, L.H. Ultra-processed food and incident type 2 diabetes: Studying the underlying consumption patterns to unravel the health effects of this heterogeneous food category in the prospective Lifelines cohort. BMC Med. 2022, 20, 7.
- Leone, A.; Martínez-González, M.Á.; Craig, W.; Fresán, U.; Gómez-Donoso, C.; Bes-Rastrollo, M. Pre-gestational consumption of ultra-processed foods and risk of gestational diabetes in a mediterranean cohort. The SUN project. Nutrients 2021, 13, 2202. Sartorelli, D.S.; Crivellenti, L.C.; Zuccolotto, D.C.C.; Franco, L.J. Relationship between minimally and ultra-processed food intake during pregnancy with obesity and gestational diabetes mellitus. Cad. Saude. Publica 2019, 35, e00049318.
- Silva, C.F.M.; Saunders, C.; Peres, W.; Folino, B.; Kamel, T.; dos Santos, M.S.; Padilha, P. Effect of ultra-processed foods consumption on glycemic control and gestational weight gain in pregnant with pregestational diabetes mellitus using carbohydrate counting. PeerJ 2021, 9, e10514. Leone, A.; Martínez-González, M.Á.; Craig, W.; Fresán, U.; Gómez-Donoso, C.; Bes-Rastrollo, M. Pre-gestational consumption of ultra-processed foods and risk of gestational diabetes in a mediterranean cohort. The SUN project. Nutrients 2021, 13, 2202.
- Da Costa Louzada, M.L.; Baraldi, L.G.; Steele, E.M.; Martins, A.P.B.; Canella, D.S.; Moubarac, J.-C.; Levy, R.B.; Cannon, G.; Afshin, A.; Imamura, F. Consumption of ultra-processed foods and obesity in Brazilian adolescents and adults. Prev. Med. 2015, 81, 9–15. Silva, C.F.M.; Saunders, C.; Peres, W.; Folino, B.; Kamel, T.; dos Santos, M.S.; Padilha, P. Effect of ultra-processed foods consumption on glycemic control and gestational weight gain in pregnant with pregestational diabetes mellitus using carbohydrate counting. PeerJ 2021, 9, e10514.
- McRae, M.P. Dietary Fiber Intake and Type 2 Diabetes Mellitus: An Umbrella Review of Meta-analyses. J. Chiropr. Med. 2018, 17, 44–53. Da Costa Louzada, M.L.; Baraldi, L.G.; Steele, E.M.; Martins, A.P.B.; Canella, D.S.; Moubarac, J.-C.; Levy, R.B.; Cannon, G.; Afshin, A.; Imamura, F. Consumption of ultra-processed foods and obesity in Brazilian adolescents and adults. Prev. Med. 2015, 81, 9–15.
- Partula, V.; Deschasaux, M.; Druesne-Pecollo, N.; Latino-Martel, P.; Desmetz, E.; Chazelas, E.; Kesse-Guyot, E.; Julia, C.; Fezeu, L.K.; Galan, P.; et al. Associations between consumption of dietary fibers and the risk of cardiovascular diseases, cancers, type 2 diabetes, and mortality in the prospective NutriNet-Santé cohort. Am. J. Clin. Nutr. 2020, 112, 195–207. McRae, M.P. Dietary Fiber Intake and Type 2 Diabetes Mellitus: An Umbrella Review of Meta-analyses. J. Chiropr. Med. 2018, 17, 44–53.
- Gbadamosi, M.A.; Tlou, B. Modifiable risk factors associated with non-communicable diseases among adult outpatients in Manzini, Swaziland: A cross-sectional study. BMC Public Health 2020, 20, 665. Partula, V.; Deschasaux, M.; Druesne-Pecollo, N.; Latino-Martel, P.; Desmetz, E.; Chazelas, E.; Kesse-Guyot, E.; Julia, C.; Fezeu, L.K.; Galan, P.; et al. Associations between consumption of dietary fibers and the risk of cardiovascular diseases, cancers, type 2 diabetes, and mortality in the prospective NutriNet-Santé cohort. Am. J. Clin. Nutr. 2020, 112, 195–207.
- Sarmento, R.A.; Antonio, J.P.; de Miranda, I.L.; Nicoletto, B.B.; de Almeida, J.C. Eating Patterns and Health Outcomes in Patients With Type 2 Diabetes. J. Endocr. Soc. 2018, 2, 42–52. Gbadamosi, M.A.; Tlou, B. Modifiable risk factors associated with non-communicable diseases among adult outpatients in Manzini, Swaziland: A cross-sectional study. BMC Public Health 2020, 20, 665.
- Garshick, M.; Mochari-Greenberger, H.; Mosca, L. Reduction in dietary trans fat intake is associated with decreased LDL particle number in a primary prevention population. Nutr. Metab. Cardiovasc. 2014, 24, 100–106. Sarmento, R.A.; Antonio, J.P.; de Miranda, I.L.; Nicoletto, B.B.; de Almeida, J.C. Eating Patterns and Health Outcomes in Patients With Type 2 Diabetes. J. Endocr. Soc. 2018, 2, 42–52.
- Kesse-Guyot, E.; Chaltiel, D.; Fezeu, L.K.; Baudry, J.; Druesne-Pecollo, N.; Galan, P.; Deschamps, V.; Touvier, M.; Julia, C.; Hercberg, S. Association between adherence to the French dietary guidelines and the risk of type 2 diabetes. Nutrition 2021, 84, 111107. Garshick, M.; Mochari-Greenberger, H.; Mosca, L. Reduction in dietary trans fat intake is associated with decreased LDL particle number in a primary prevention population. Nutr. Metab. Cardiovasc. 2014, 24, 100–106.
- Michaud, M.; Balardy, L.; Moulis, G.; Gaudin, C.; Peyrot, C.; Vellas, B.; Cesari, M.; Nourhashemi, F. Proinflammatory Cytokines, Aging, and Age-Related Diseases. J. Am. Med. Dir. Assoc. 2013, 14, 877–882. Kesse-Guyot, E.; Chaltiel, D.; Fezeu, L.K.; Baudry, J.; Druesne-Pecollo, N.; Galan, P.; Deschamps, V.; Touvier, M.; Julia, C.; Hercberg, S. Association between adherence to the French dietary guidelines and the risk of type 2 diabetes. Nutrition 2021, 84, 111107.
- Müller, L.; Benedetto, S.D.; Pawelec, G. The immune system and its dysregulation with aging. Subcell Biochem. 2019, 91, 21–43. Michaud, M.; Balardy, L.; Moulis, G.; Gaudin, C.; Peyrot, C.; Vellas, B.; Cesari, M.; Nourhashemi, F. Proinflammatory Cytokines, Aging, and Age-Related Diseases. J. Am. Med. Dir. Assoc. 2013, 14, 877–882.
- Müller, L.; Benedetto, S.D.; Pawelec, G. The immune system and its dysregulation with aging. Subcell Biochem. 2019, 91, 21–43.
