Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 3 by Dean Liu and Version 2 by mohammadreza pourkarim.
New technologies are supported by the global implementation of the internet. These improvements have deeply affected various disciplines of sciences and consequently changed services such as daily business, particularly health sectors. Innovative digital marketing strategies utilize the channels of social media and retrieved user data to analyze and improve relevant services. These multidisciplinary innovations can assist specialists, physicians and researchers in diagnostic, prophylaxis and treatment issues in the health sector.
- digital marketing
- viral hepatitis
- elimination
- WHO
- influencers
- MANAGEMENT
- campaign
1. Social Media’s Impact on Health Care System
The future of health sectors is deeply linked to the application of advanced technologies. New technologies can lead to a massive change in healthcare practice and its related business sectors in a variety of ways. Companies involved in the food and pharmaceutical industry as well as hospital and producers of laboratory equipment take advantage from new technologies to deliver their products and services to the customers and end users. Furthermore, digital innovations can assist specialists, physicians and researchers in diagnostic, prophylaxis and treatment issues [14,15][1][2]. Compared to recent decades, health decision makers are more accurate and trustful in defining new strategies. Different national and international health organizations use these social media platforms to communicate, design and disseminate their health strategies [16][3]. The World Health Organization (WHO) has already used social media platforms, such as Twitter and other social networks, to communicate and report on health care information [17][4]. This organization calls for social media to be more active in broadcasting health messages to the public, under normal circumstances and during a health crisis [18][5]. Based on data collected from different regions, the WHO anticipates a shortage of human resources in the health care of nearly 12.9 million worldwide by 2035. To counter the shortage of personnel, the WHO is ambitious to apply new technologies for attracting and allocating people with different specialties in healthcare [19,20][6][7]. Additionally, the management of patients has substantially improved, and personalized contact between patients and the healthcare staff is straightforward and more convincing [21][8]. There is an ongoing evolution in communication platforms, and those that have implement these advanced digital technologies in their health system have significantly benefited by attracting larger audiences and consumer groups (Figure 1) [22][9].
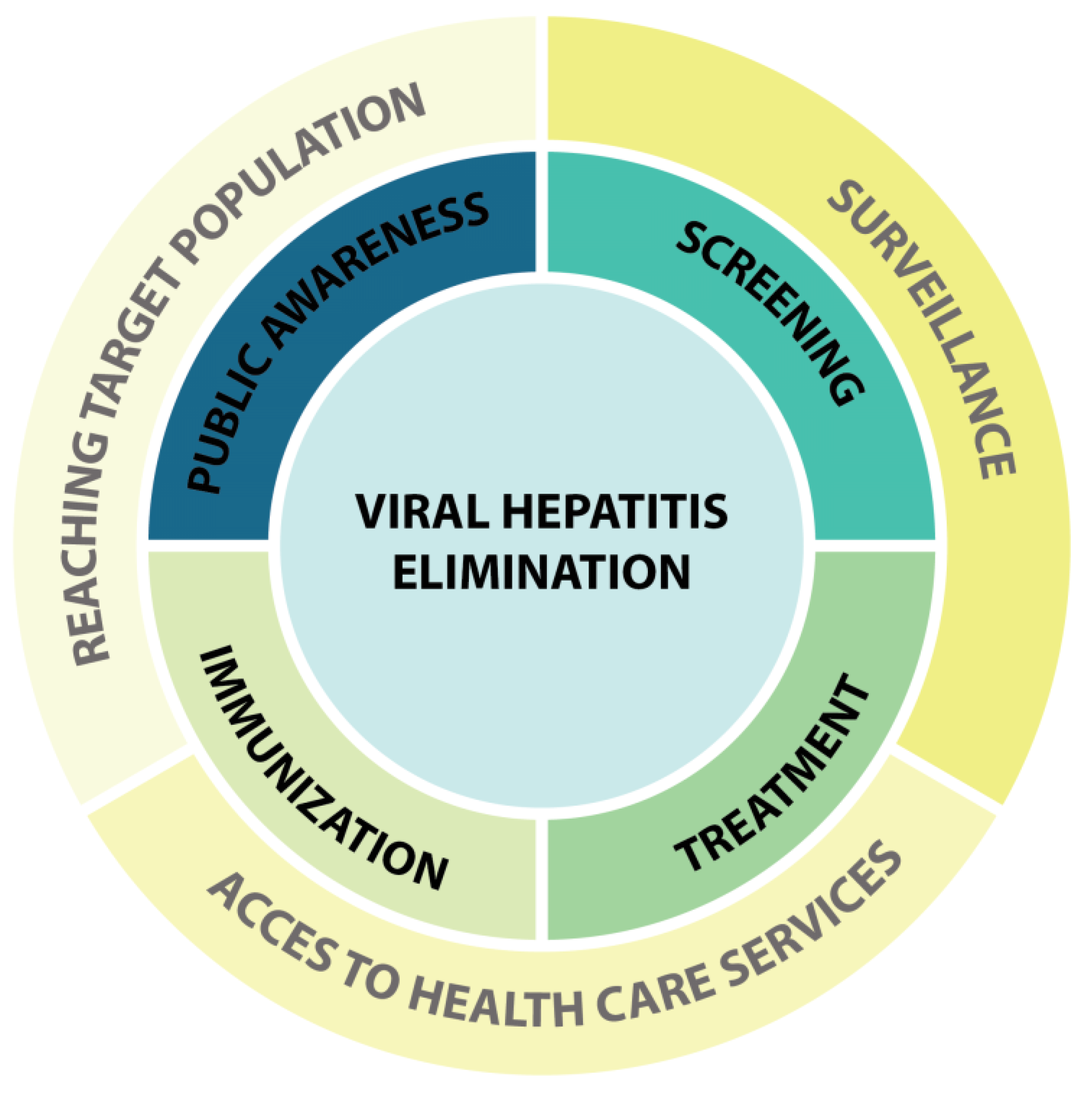
Figure 1. Application of digital marketing in program of viral hepatitis elimination. Center of diagram shows the goal of program. This goal is achieved by measurements such as increases in public awareness, screening, treatment and immunization against viral hepatitis (middle zoon). Medical apps, social media influencers and campaigns support and facilitate those medical services through surveillance, reaching target population and access to healthcare services (outer zoon).
In parallel with health service providers, digital technologies are frequently used by ordinary people who search and look for answers on questions about their health on the internet [23,24][10][11]. Surprisingly, monitoring health-seeking queries on the web in different geographical regions and seasons can provide big data, which can be used to analyze real world health associated developments. For instance, it has been shown that the frequency of certain key words in the web correlate with the number of patients with influenza-like illnesses who refer to physicians in some geographical regions [25][12]. This sort of digital-based data analysis can support innovative surveillance systems that can assist epidemiologists in the identification of seasonal influenza epidemics [26][13]. The same approach has been used in the surveillance of Dengue virus [27][14]. Furthermore, in some tropical countries such as India, Indonesia, Singapore, Bolivia and Brazil, web search query data corresponded with the resurgence of Dengue virus [28][15]. Beyond pathogen surveillance, data on web behavior can be utilized as a health indicator of web users and to determine their access to healthcare facilities, including screening tests, vaccine, physicians and therapies (Figure 1) [24][11]. Additionally, the utility of web-based data can be beneficial for the assessment of other health issues such as contraception [29[16][17],30], diabetes [31[18][19],32], obesity [33][20] or cardiovascular diseases [34][21]. However, in the case of communicable diseases, the application of digital technology has extraordinary relevance.
The relevance of digital innovations is highlighted when wresearchers are confronted with human pathogens that cause significant morbidity/mortality, especially during the early days of epidemics. In moments when there is lack of information and few effective therapies (e.g., vaccines and medication), a unified and appropriate response is very critical. Accordingly, it has been demonstrated that access to digitally generated data on platforms of social media can empower an immediate response or/and control the spread of viral diseases such as HIV and Ebola [24,35][11][22]. For instance, during the Ebola epidemics in Africa, a global massive web search was observed. Interestingly, a significant positive correlation was reported between social media behavior (e.g., number of tweets) and an increasing prevalence of HIV, which exemplifies the massive potential of social media’s impact on health status information of users (Figure 1) [36,37][23][24]. The analysis of such geographical location specific data retrieved from web searches helps the health authorities implement appropriate and timely actions. Via social media networking, public health researchers or clinicians have access to a wide/global audience (Figure 1) [38,39][25][26]. This allows the rapid communication of health-related information and might contribute to the improvement of the society’s health status. Several studies have shown that users follow up the advice of messages posted on social media by health advisers [6,40,41,42][27][28][29][30]. Therefore, communicating the implementation of interventions alongside messages to support healthy behavior could have tremendous value and interests. For example, research projects that offered home HIV testing through social media platforms, known as app-based intervention, has been well accepted. [41,43][29][31].
Antimicrobial resistance is another serious health concern that is highlighted in human digital communication. By 2050, 10 million deaths due to antimicrobial resistance are estimated per year, which highlights an eminent threat to human health [44][32]. Recent investigations have demonstrated that misunderstandings and wrong public perceptions underlie antibiotic overconsumption [45,46,47][33][34][35]. Furthermore, self-medication, off-label use (e.g., for curing viral infections) and suboptimal dosing of antibiotics are examples of misconception that occur in both developing and developed countries [48,49][36][37]. Several strategies, such as different assessments or educational programs, have been implemented to increase knowledge concerning antibiotic use and infectious diseases [47][35]. Among a variety of tools, social networking platforms such as Facebook pages, Twitter and YouTube have been efficiently used change public perception (Figure 1) [39,50,51][26][38][39]. The dissemination of an educational program called “antimicrobial stewardship” (ASP) on Facebook and Twitter for students of medicine is a worthy example of the application of social media technologies [50,52][38][40]. Further, to increase students’ awareness, online games about antibiotics have been launched in the UK and USA, which had a positive impact [53][41]. However, the use digital marketing in health system is not always a success story, as has been demonstrated in the case of measles. Despite the availability of an effective vaccine, measles is still a worldwide public health concern, with several measles outbreaks, even in developed countries, in recent years [54][42]. Health policy makers have used social media to promote vaccination programs; however, antivaccine movements have applied similar tools to spread disinformation [55][43]. More so, the activity of the antivaccination (anti-vax) movement on social media seems much higher and more successful compared to the pro-vaccines movement, which contributes to the increased vaccine hesitancy. [56,57][44][45]. A survey showed that activities of the anti-vax movement on Twitter positively correlated with the incidence of measles outbreaks and a drop in vaccine coverage [58][46]. Antivaccine discourses on social media majorly highlight potential vaccine side effects and deaths. Additionally, they try to link the deaths to conspiracy theories and attempt to minimize the effectiveness of vaccines. However, none of them use scientific arguments to support their claims [58][46]. Contrasting the anti-vax movement, communication that reverberate on social media has been able to transmit well-informed information about measles infection sequela and has assisted parents in making the correct decision for vaccination [59][47]. Vaccination against influenza and HPV are experiencing the same scenarios on social media in which misinformation is propagated by antivaccine movements [60,61,62][48][49][50].
Besides monodirectional communication and the dispatch of health messages, social media platforms enable the interactions between stakeholders, such as healthy individuals and patients, patients and specialists and ordinary people who are interested in a healthy lifestyle [63][51]. Nowadays, patients can communicate through social media with health specialists rather than planning visits and speaking in person [64][52]. This can decrease the number of hospital visits [64][52]. In addition to social networking sites, different applications and algorithms offered by authorities of digital markets can be used as blueprints for this bidirectional interaction [65][53]. The term Mobile Health (mHealth) implies the use of different applications (apps) on mobile phones or tablets, which assist in monitoring the personal health of users [66][54]. In such platforms, advice on daily physical or mental behavior, such as diets, activities and treatments, are suggested to the users. Eventually, the daily functioning of the user is monitored, and personalized reports are delivered [67,68,69,70,71][55][56][57][58][59].
2. Current Pandemic and Digital Revolution
From the first days of the SARS-CoV-2 pandemic, which started in December 2019 in China, digital marketing tools (e.g., social media) demonstrated their potential use in times of crisis [72,73][60][61]. Not surprisingly, the first diagnostic report of a suspected pneumonia case with unknown etiology was posted on WeChat by Dr. Li Wenliang, who later died from the same illness. Although the use of social media to disseminate information was adopted in previous epidemics such as Ebola outbreaks [74][62], Zika virus [75][63], Influenza [76][64], Dengue [77][65] and MERS-CoV [78][66], the wide application of digital technology in the SARS-CoV-2 pandemic was beyond previous experiences. The World Health Organization (WHO) noted that “the coronavirus disease 2019 (COVID-19) is the first pandemic in history in which technology and social media are being used on a massive scale.” [79][67]. Accordingly, by applying social media, health information spread quickly and was instantly shared with the public to inform people about the epidemic, prophylactic measures and treatments [80,81,82][68][69][70]. Furthermore, through different channels of social media, bidirectional communication was implemented during phases of lockdown for people with health-related questions and/or to increase their own awareness [82,83][70][71]. This demand was partially linked to the current COVID-19 pandemic, and other needs were related to other illnesses in which patients needed remote care, relevant advice, and medical services (Figure 1) [84,85][72][73].
Access to trustable information is very important, and the spread of fake news has been a major threat for the credibility of social media during the COVID-19 pandemic [86][74]. In the first months of 2020, plenty of disinformation was shared social media that included conspiracy theories, in which bioweapons, the involvement of Bill Gates and the implementation the 5G network were introduced as the main causes or catalyzers of COVID-19 spread [87,88][75][76]. In contrast, following the approval of SARS-CoV-2 vaccines, social media was a crucial platform for the roll-out of vaccines. However, similar to previous vaccination campaigns, individuals used social media channels to spread conspiracy theories and antivaccination disinformation to disturb the immunization program and avoid vaccinations [89,90,91][77][78][79]. Unfortunately, the view rate of vaccine-opposing posts related to SARS-CoV-2 was much higher than the views of pro-vaccine messages [92,93,94,95][80][81][82][83]. Besides vaccine inequity, vaccine hesitancy, which counters public health messages, is now considered a real hurdle for vaccination against SARS-CoV-2 [96,97][84][85].
The current pandemic has been a trigger for users to innovate digital marketing. These initiatives are taken by users to intensify and amplify their activities. Often, people utilize more than one platform of social media. It allows them to disseminate information from one platform to another. This type of activity, which is called cross-platform use [79[67][86],98], is often applied by the antivaccine movement to support tweets with links to YouTube. This nimble strategy tries to boost the dispersal of vaccine-opposing videos by re-tweeting antivaccine contents [99][87]. Unfortunately, this strategy has not been thoroughly used by health authorities so far.
“EpiTweetr” is another innovative tool that was developed by the European Center for Diseases Control (ECDC). This tool allows epidemiologist to track possible emerging threats through searches on different platforms particularly Twitter. This tool automatically monitors, collects and processes data on Twitter and informs experts when the posted material on Twitter is not ordinary. For instance, when an increasing number of Tweets include keywords, such as the name of a pathogen, EpiTweetr automatically informs the end-user. The generated information is the result of massive data collection that has been filtered and validated by the tool. In detail, the signaling of a threat at the early stages is detected in Twitter by EpiTwittr; however, the validation of these data is necessary. Therefore, these signals are checked and approved by public health institutes and international organizations. However, to not miss potential risks, the received signals are rechecked in other platforms of social media as well.
Although EpiTweetr is a free package tool that can be used for any potential threat, the current pandemic helped the ECDC to improve this tool in terms of data collection, processing and visualization for end users. [100][88].
The current pandemic has highlighted the importance of mobile health apps and digital technologies on human health [101,102,103][89][90][91]. To combat the pandemic, huge numbers of mobile applications are available in different countries to share health information and/or trace contacts [104,105][92][93]. These applications can track the health situation of the users and prevent the dispersal of SARS-CoV-2 [106][94]. Eventually, these tools successfully reduced the global costs/health burden COVID-19 [107][95]. Apps such as mHealth have frequently been used during vaccination processes against COVID-19 and are currently used in campaigns for vaccination against HPV and influenza [108,109,110][96][97][98]. Undoubtedly, without digital marketing health tools, the roll-out of mass vaccinations would be more challenging. These tools have been used to contact eligible persons for vaccinations. Furthermore, individuals are regularly invited or reminded by phone message or app notifications to make an appointment and to ensure the completion of the full vaccination program (e.g., the administration of booster vaccines). In addition to the dispersal of vaccines, apps can be used to monitor post-vaccination side effects. After finalizing the vaccination program, a digital immunity certificate or vaccination passport can be issued, which is always presentable by vaccinees [111][99]. This final key service of digital health is online issued evidence, which allows vaccinees to travel and access public places without restrictions. Recent evaluations showed that the digital vaccine passport had a positive impact on re-opening economies [112][100]. Importantly, the usage of mobile applications during the COVID-19 pandemic was confronted with some restrictions that originated from cultural, demographic and political issues in some country [107,113,114][95][101][102]. For instance, using mHealth for contact tracing and the registration of vaccine passports is highly controversial in some regions [115][103].
The COVID-19 pandemic has not only accelerated the digitalization of the health sector but also added new concepts by the introduction of digital vaccination passports, a series of nexuses such as the “Diplomacy for digital health,” “Digital health for diplomacy,” and “Digital health in diplomacy”. These developments have become more widespread on a global scale [114,116,117,118,119][102][104][105][106][107]. Undoubtedly, the COVID-19 pandemic was an important scene for the development and implementation of digital marketing tools, including social media and mobile apps, for health-related issues at a global level. These tools assisted health policymakers to implement a series of efficient responses to pandemic and will certainly be applied in pandemic preparedness programs.
3. Engagement of Influencers in Public Health Issues
For market managers, the power of influencers is worthy [120][108]. Individuals with a large number of followers on social media can efficiently increase the selling rates of a products [121][109]. It has been shown that people like to follow individuals that have created their own follower community and are directly accessible and responsive to the audience. This contrasts with traditional celebrities that have a mass audience and are not tangible for ordinary people. Influencers, or micro-influencers, are trusted by the audience, and compared to known celebrities, their recommendations and advocations are often accepted by their followers [122,123][110][111]. Accordingly, influencers have an impact on decisions makers and can turn/drive the decisions of followers towards some specific products or opinions. There is an increasing body of evidence that social media influencers have a positive impact on public health issues [124,125][112][113] such as reducing smoking [126,127][114][115] and vaccination against HPV or influenza [95,128,129][83][116][117]. The use of influencers in public health is an intervention that can transmit tailored messages and inspire social media users to change their behaviors [95][83]. Furthermore, influencers can collaborate with public health policy makers and support them in the use of social media. Additionally, influencers’ population-targeted engagement has a positive impact on the health improvement of high-risk populations, e.g., immigrants [130,131,132,133,134][118][119][120][121][122].
It seems that all mentioned worthy experiences and knowledge from different disciplines in digital marketing have created a paved path for supporting health programs such as the elimination of widespread pathogens.
References
- Glazyrin, Y.E.; Veprintsev, D.V.; Ler, I.A.; Rossovskaya, M.L.; Varygina, S.A.; Glizer, S.L.; Zamay, T.N.; Petrova, M.M.; Minic, Z.; Berezovski, M.V. Proteomics-Based Machine Learning Approach as an Alternative to Conventional Biomarkers for Differential Diagnosis of Chronic Kidney Diseases. Int. J. Mol. Sci. 2020, 21, 4802.
- Fang, C.; An, J.; Bruno, A.; Cai, X.; Fan, J.; Fujimoto, J.; Golfieri, R.; Hao, X.; Jiang, H.; Jiao, L.R. Consensus recommendations of three-dimensional visualization for diagnosis and management of liver diseases. Hepatol. Int. 2020, 14, 437–453.
- Utunen, H.; Attias, M.; George, R.; Ndiaye, N.; Piroux, C.; Farzi, M.R.; Sy, A.; Gamhewage, G. Global Access to OpenWHO’s Online Learning Resources for COVID-19. Stud. Health Technol. Inform. 2020, 272, 304–305.
- Moorhead, S.A.; Hazlett, D.E.; Harrison, L.; Carroll, J.K.; Irwin, A.; Hoving, C. A new dimension of health care: Systematic review of the uses, benefits, and limitations of social media for health communication. J. Med. Internet Res. 2013, 15, e85.
- Tang, L.; Bie, B.; Park, S.-E.; Zhi, D. Social media and outbreaks of emerging infectious diseases: A systematic review of literature. Am. J. Infect. Control. 2018, 46, 962–972.
- Truth, A.U. No health without a workforce. In World Health Organisation (WHO) Report; WHO: Geneva, Switzerland, 2013; pp. 1–104.
- Dhingra, D.; Dabas, A. Global Strategy on Digital Health. Indian Pediatrics 2020, 57, 356–358.
- Improta, G.; De Luca, V.; Illario, M.; Triassi, M. Digital innovation in healthcare: A device with a method for monitoring, managing and preventing the risk of chronic polypathological patients. Transl. Med. UniSa 2020, 21, 61.
- Simpson, S.; Reid, C. Telepsychology in A ustralia: 2020 vision. Aust. J. Rural. Health 2014, 22, 306–309.
- Fox, S. Online Health Search 2006. Pew Internet and American Life Project. 29 October 2006. Available online: http://www.pewinternet.org/pdfs/PIP_Online_Health_2006.pdf (accessed on 29 October 2006).
- Nielsen, R.C.; Luengo-Oroz, M.; Mello, M.B.; Paz, J.; Pantin, C.; Erkkola, T. Social media monitoring of discrimination and HIV testing in Brazil, 2014–2015. AIDS Behav. 2017, 21, 114–120.
- Polgreen, P.M.; Chen, Y.; Pennock, D.M.; Nelson, F.D.; Weinstein, R.A. Using internet searches for influenza surveillance. Clin. Infect. Dis. 2008, 47, 1443–1448.
- Ginsberg, J.; Mohebbi, M.H.; Patel, R.S.; Brammer, L.; Smolinski, M.S.; Brilliant, L. Detecting influenza epidemics using search engine query data. Nature 2009, 457, 1012–1014.
- Chan, E.H.; Sahai, V.; Conrad, C.; Brownstein, J.S. Using web search query data to monitor dengue epidemics: A new model for neglected tropical disease surveillance. PLoS Negl. Trop. Dis. 2011, 5, e1206.
- Chan, E.; Sahai, V.; Conrad, C.; Brownstein, J. Web search query data to monitor dengue epidemics: A new model for dengue surveillance. In Proceedings of the International Society for Disease Surveillance 10th Annual Conference 2011 Building the Future of Public Health Surveillance, Atlanta, GA, USA; 2011.
- Smith, C.; Sokhey, L.; Tijamo, C.F.E.; McLaren, M.; Free, C.; Watkins, J.; Amra, O.; Masuda, C.; Oreglia, E. Development of an intervention to support reproductive health of garment factory workers in Cambodia: A qualitative study. BMJ Open 2021, 11, e049254.
- Yousef, H.; Al-Sheyab, N.; Al Nsour, M.; Khader, Y.; Al Kattan, M.; Bardus, M.; Alyahya, M.; Taha, H.; Amiri, M. Perceptions Toward the Use of Digital Technology for Enhancing Family Planning Services: Focus Group Discussion with Beneficiaries and Key Informative Interview with Midwives. J. Med. Internet Res. 2021, 23, e25947.
- Hempler, N.F.; Joensen, L.E.; Willaing, I. Relationship between social network, social support and health behaviour in people with type 1 and type 2 diabetes: Cross-sectional studies. BMC Public Health 2016, 16, 198.
- Ashrafi, S.; Taylor, D.; Tang, T.S. Moving beyond ‘don’t ask, don’t tell’: Mental health needs of adults with type 1 diabetes in rural and remote regions of British Columbia. Diabet. Med. 2021, 38, e14534.
- Li, C.; Ademiluyi, A.; Ge, Y.; Park, A. Using Social Media to Understand Web-Based Social Factors Concerning Obesity: Systematic Review. JMIR Public Health Surveill. 2022, 8, e25552.
- Yan, Q.; Jensen, K.J.; Thomas, R.; Field, A.R.; Jiang, Z.; Goei, C.; Davies, M.G. Digital Footprint of Academic Vascular Surgeons in the Southern United States on Physician Rating Websites: Cross-sectional Evaluation Study. JMIR Cardio 2021, 5, e22975.
- Fung, I.C.-H.; Tse, Z.T.H.; Cheung, C.-N.; Miu, A.S.; Fu, K.-W. Ebola and the social media. Lancet 2014, 384, 2207.
- Young, S.D.; Rivers, C.; Lewis, B. Methods of using real-time social media technologies for detection and remote monitoring of HIV outcomes. Prev. Med. 2014, 63, 112–115.
- Stoové, M.A.; Pedrana, A.E. Making the most of a brave new world: Opportunities and considerations for using Twitter as a public health monitoring tool. Prev. Med. 2014, 63, 109–111.
- van der Worp, H.; Brandenbarg, D.; Boek, P.A.; Braams, J.H.; Brink, L.J.; Keupers, J.; Blanker, M.H. Identifying women’s preferences for treatment of urinary tract infection: A discrete choice experiment. BMJ Open 2021, 11, e049916.
- Muflih, S.M.; Al-Azzam, S.; Karasneh, R.A.; Conway, B.R.; Aldeyab, M.A. Public Health Literacy, Knowledge, and Awareness Regarding Antibiotic Use and Antimicrobial Resistance during the COVID-19 Pandemic: A Cross-Sectional Study. Antibiotics 2021, 10, 1107.
- Holloway, I.W.; Dunlap, S.; Del Pino, H.E.; Hermanstyne, K.; Pulsipher, C.; Landovitz, R.J. Online social networking, sexual risk and protective behaviors: Considerations for clinicians and researchers. Curr. Addict. Rep. 2014, 1, 220–228.
- Stevens, R.; Gilliard-Matthews, S.; Dunaev, J.; Todhunter-Reid, A.; Brawner, B.; Stewart, J. Social media use and sexual risk reduction behavior among minority youth: Seeking safe sex information. Nurs. Res. 2017, 66, 368.
- Phillips, G.; Magnus, M.; Kuo, I.; Rawls, A.; Peterson, J.; Jia, Y.; Opoku, J.; Greenberg, A.E. Use of geosocial networking (GSN) mobile phone applications to find men for sex by men who have sex with men (MSM) in Washington, DC. AIDS Behav. 2014, 18, 1630–1637.
- Rendina, H.J.; Jimenez, R.H.; Grov, C.; Ventuneac, A.; Parsons, J.T. Patterns of lifetime and recent HIV testing among men who have sex with men in New York City who use Grindr. AIDS Behav. 2014, 18, 41–49.
- Holloway, I.W.; Rice, E.; Gibbs, J.; Winetrobe, H.; Dunlap, S.; Rhoades, H. Acceptability of smartphone application-based HIV prevention among young men who have sex with men. AIDS Behav. 2014, 18, 285–296.
- Acharya, K.P.; Subedi, D. Use of Social Media as a Tool to Reduce Antibiotic Usage: A Neglected Approach to Combat Antimicrobial Resistance in Low and Middle Income Countries. Front. Public Health 2020, 8, 671.
- Mazińska, B.; Strużycka, I.; Hryniewicz, W. Surveys of public knowledge and attitudes with regard to antibiotics in Poland: Did the European Antibiotic Awareness Day campaigns change attitudes? PLoS ONE 2017, 12, e0172146.
- Lam, T.; Lam, K.; Ho, P.; Yung, W. Knowledge, attitude, and behaviour toward antibiotics among Hong Kong people: Local-born versus immigrants. Hong Kong Med. J. 2015, 21, S41–S47.
- Or, P.-L.; Ching, T.-Y. The effectiveness of raising Hong Kong parents’ awareness of antimicrobial resistance through an education program with peer support on social media: A randomized, controlled pilot study. BMC Public Health 2022, 22, 315.
- Alumran, A.; Hou, X.-Y.; Hurst, C. Assessing the overuse of antibiotics in children in Saudi Arabia: Validation of the parental perception on antibiotics scale (PAPA scale). Health Qual. Life Outcomes 2013, 11, 39.
- Hutinel, M.; Larsson, D.J.; Flach, C.-F. Antibiotic resistance genes of emerging concern in municipal and hospital wastewater from a major Swedish city. Sci. Total Environ. 2022, 812, 151433.
- Ellis, J.; Vassilev, I.; Kennedy, A.; Moore, M.; Rogers, A. Help seeking for antibiotics; is the influence of a personal social network relevant? BMC Fam. Pract. 2019, 20, 63.
- Djerf-Pierre, M.; Lindgren, M. Making sense of “superbugs” on YouTube: A storytelling approach. Public Underst. Sci. 2021, 30, 535–551.
- Pisano, J.; Pettit, N.; Bartlett, A.; Bhagat, P.; Han, Z.; Liao, C.; Landon, E. Social media as a tool for antimicrobial stewardship. Am. J. Infect. Control. 2016, 44, 1231–1236.
- Hale, A.R.; Young, V.L.; Grand, A.; McNulty, C.A.M. Can gaming increase antibiotic awareness in children? A mixed-methods approach. JMIR Serious Games 2017, 5, e6420.
- Patel, M.K.; Dumolard, L.; Nedelec, Y.; Sodha, S.V.; Steulet, C.; Gacic-Dobo, M.; Kretsinger, K.; McFarland, J.; Rota, P.A.; Goodson, J.L. Progress toward regional measles elimination—worldwide, 2000–2018. Morb. Mortal. Wkly. Rep. 2019, 68, 1105.
- Wawrzuta, D.; Jaworski, M.; Gotlib, J.; Panczyk, M. Characteristics of antivaccine messages on social media: Systematic review. J. Med. Internet Res. 2021, 23, e24564.
- Schmidt, A.L.; Zollo, F.; Scala, A.; Betsch, C.; Quattrociocchi, W. Polarization of the vaccination debate on Facebook. Vaccine 2018, 36, 3606–3612.
- Bozzola, E.; Spina, G.; Tozzi, A.E.; Villani, A. Global measles epidemic risk: Current perspectives on the growing need for implementing digital communication strategies. Risk Manag. Healthc. Policy 2020, 13, 2819.
- Gunaratne, K.; Coomes, E.A.; Haghbayan, H. Temporal trends in anti-vaccine discourse on Twitter. Vaccine 2019, 37, 4867–4871.
- Broniatowski, D.A.; Hilyard, K.M.; Dredze, M. Effective vaccine communication during the disneyland measles outbreak. Vaccine 2016, 34, 3225–3228.
- Kang, G.J.; Culp, R.K.; Abbas, K.M. Facilitators and barriers of parental attitudes and beliefs toward school-located influenza vaccination in the United States: Systematic review. Vaccine 2017, 35, 1987–1995.
- Bodson, J.; Wilson, A.; Warner, E.L.; Kepka, D. Religion and HPV vaccine-related awareness, knowledge, and receipt among insured women aged 18-26 in Utah. PLoS ONE 2017, 12, e0183725.
- Massey, P.M.; Kearney, M.D.; Hauer, M.K.; Selvan, P.; Koku, E.; Leader, A.E. Dimensions of misinformation about the HPV vaccine on Instagram: Content and network analysis of social media characteristics. J. Med. Internet Res. 2020, 22, e21451.
- Zhong, B.; Liu, Q. Medical Insights from Posts About Irritable Bowel Syndrome by Adolescent Patients and Their Parents: Topic Modeling and Social Network Analysis. J. Med. Internet Res. 2021, 23, e26867.
- Lammert, C.; Comerford, M.; Love, J.; Bailey, J.R. Investigation gone viral: Application of the social mediasphere in research. Gastroenterology 2015, 149, 839–843.
- Sheppard, M.K. mHealth Apps: Disruptive Innovation, Regulation, and Trust—A Need for Balance. Med. Law Rev. 2020, 28, 549–572.
- Lewis, R.A.; Lunney, M.; Chong, C.; Tonelli, M. Identifying Mobile Applications Aimed at Self-Management in People with Chronic Kidney Disease. Can. J. Kidney Health Dis. 2019, 6, 2054358119834283.
- Falkenhain, K.; Locke, S.R.; Lowe, D.A.; Lee, T.; Singer, J.; Weiss, E.J.; Little, J.P. Use of an mHealth Ketogenic Diet App Intervention and User Behaviors Associated with Weight Loss in Adults with Overweight or Obesity: Secondary Analysis of a Randomized Clinical Trial. JMIR mHealth uHealth 2022, 10, e33940.
- Turesson, C.; Liedberg, G.; Björk, M. Development of a Digital Support Application with Evidence-Based Content for Sustainable Return to Work for Persons with Chronic Pain and Their Employers: User-Centered Agile Design Approach. JMIR Hum. Factors 2022, 9, e33571.
- Rochat, J.; Ehrler, F.; Siebert, J.N.; Ricci, A.; Ruiz, V.G.; Lovis, C. Usability Testing of a Patient-Centered Mobile Health App for Supporting and Guiding the Pediatric Emergency Department Patient Journey: Mixed Methods Study. JMIR Pediatrics Parent. 2022, 5, e25540.
- Denecke, K.; Schmid, N.; Nüssli, S. Implementation of Cognitive Behavioral Therapy in e–Mental Health Apps: Literature Review. J. Med. Internet Res. 2022, 24, e27791.
- Anastasiadou, D.; Lupiañez-Villanueva, F.; Faulí, C.; Cunillera, J.A.; Serrano-Troncoso, E. Cost-effectiveness of the mobile application TCApp combined with face-to-face CBT treatment compared to face-to-face CBT treatment alone for patients with an eating disorder: Study protocol of a multi-centre randomised controlled trial. BMC Psychiatry 2018, 18, 118.
- Oladeru, O.T.; Eber, G.; McClelland, S., III. Should patients who are incarcerated on death row receive palliative cancer care? Lancet Oncol. 2020, 21, 337–338.
- Lwin, M.O.; Lu, J.; Sheldenkar, A.; Schulz, P.J.; Shin, W.; Gupta, R.; Yang, Y. Global sentiments surrounding the COVID-19 pandemic on Twitter: Analysis of Twitter trends. JMIR Public Health Surveill. 2020, 6, e19447.
- Seltzer, E.K.; Jean, N.; Kramer-Golinkoff, E.; Asch, D.A.; Merchant, R. The content of social media’s shared images about Ebola: A retrospective study. Public Health 2015, 129, 1273–1277.
- Gui, X.; Wang, Y.; Kou, Y.; Reynolds, T.L.; Chen, Y.; Mei, Q.; Zheng, K. Understanding the patterns of health information dissemination on social media during the Zika outbreak. AMIA Annu. Symp. Proc. 2017, 2017, 820–829.
- Gu, H.; Chen, B.; Zhu, H.; Jiang, T.; Wang, X.; Chen, L.; Jiang, Z.; Zheng, D.; Jiang, J. Importance of Internet surveillance in public health emergency control and prevention: Evidence from a digital epidemiologic study during avian influenza A H7N9 outbreaks. J. Med. Internet Res. 2014, 16, e2911.
- Lwin, M.O.; Jayasundar, K.; Sheldenkar, A.; Wijayamuni, R.; Wimalaratne, P.; Ernst, K.C.; Foo, S. Lessons from the implementation of Mo-Buzz, a mobile pandemic surveillance system for dengue. JMIR Public Health Surveill. 2017, 3, e7376.
- Fung, I.C.-H.; Fu, K.-W.; Ying, Y.; Schaible, B.; Hao, Y.; Chan, C.-H.; Tse, Z.T.-H. Chinese social media reaction to the MERS-CoV and avian influenza A (H7N9) outbreaks. Infect. Dis. Poverty 2013, 2, 31.
- Ginossar, T.; Cruickshank, I.J.; Zheleva, E.; Sulskis, J.; Berger-Wolf, T. Cross-platform spread: Vaccine-related content, sources, and conspiracy theories in YouTube videos shared in early Twitter COVID-19 conversations. Hum. Vaccines Immunother. 2022, 18, 1–13.
- Thijssen, M.; Devos, T.; Ejtahed, H.-S.; Amini-Bavil-Olyaee, S.; Pourfathollah, A.A.; Pourkarim, M.R. Convalescent plasma against COVID-19: A broad-spectrum therapeutic approach for emerging infectious diseases. Microorganisms 2020, 8, 1733.
- Halim, D.A.; Kurniawan, A.; Agung, F.H.; Angelina, S.; Jodhinata, C.; Winata, S.; Wijovi, F.; Agatha, C.M. Understanding of Young People About COVID-19 During Early Outbreak in Indonesia. Asia-Pac. J. Public Health 2020, 32, 363–365.
- Yousuf, H.; Corbin, J.; Sweep, G.; Hofstra, M.; Scherder, E.; Van Gorp, E.; Zwetsloot, P.P.; Zhao, J.; Van Rossum, B.; Jiang, T. Association of a public health campaign about coronavirus disease 2019 promoted by news media and a social influencer with self-reported personal hygiene and physical distancing in the Netherlands. JAMA Netw. Open 2020, 3, e2014323.
- Stechemesser, A.; Wenz, L.; Levermann, A. Corona crisis fuels racially profiled hate in social media networks. EClinicalMedicine 2020, 23, 100372.
- Yadav, S.K.; Yadav, N. Continuity of cancer care in the era of COVID-19 pandemic: Role of social media in low-and middle-income countries. World J. Clin. Cases 2021, 9, 291.
- Li, H.; Zheng, S.; Da Li, D.J.; Liu, F.; Guo, W.; Zhao, Z.; Zhou, Y.; Liu, J.; Zhao, R. The Establishment and Practice of Pharmacy Care Service Based on Internet Social Media: Telemedicine in Response to the COVID-19 Pandemic. Front. Pharmacol. 2021, 12, 707442.
- Pulido, C.M.; Ruiz-Eugenio, L.; Redondo-Sama, G.; Villarejo-Carballido, B. A New Application of Social Impact in Social Media for Overcoming Fake News in Health. Int. J. Environ. Res. Public Health 2020, 17, 2430.
- Constantinou, M.; Kagialis, A.; Karekla, M. COVID-19 scientific facts vs. Conspiracy theories: Is science failing to pass its message? Int. J. Environ. Res. Public Health 2021, 18, 6343.
- Shahsavari, S.; Holur, P.; Wang, T.; Tangherlini, T.R.; Roychowdhury, V. Conspiracy in the time of corona: Automatic detection of emerging COVID-19 conspiracy theories in social media and the news. J. Comput. Soc. Sci. 2020, 3, 279–317.
- Siegler, A.J.; Luisi, N.; Hall, E.W.; Bradley, H.; Sanchez, T.; Lopman, B.A.; Sullivan, P.S. Trajectory of COVID-19 Vaccine Hesitancy Over Time and Association of Initial Vaccine Hesitancy with Subsequent Vaccination. JAMA Netw. Open 2021, 4, e2126882.
- Clark, S.E.; Bledsoe, M.C.; Harrison, C.J. The role of social media in promoting vaccine hesitancy. Curr. Opin. Pediatrics 2022, 34, 156–162.
- Blane, J.T.; Bellutta, D.; Carley, K.M. Social-Cyber Maneuvers During the COVID-19 Vaccine Initial Rollout: Content Analysis of Tweets. J. Med. Internet Res. 2022, 24, e34040.
- Keelan, J.; Pavri-Garcia, V.; Tomlinson, G.; Wilson, K. YouTube as a source of information on immunization: A content analysis. Jama 2007, 298, 2482–2484.
- Bonnevie, E.; Goldbarg, J.; Gallegos-Jeffrey, A.K.; Rosenberg, S.D.; Wartella, E.; Smyser, J. Content themes and influential voices within vaccine opposition on Twitter, 2019. Am. J. Public Health 2020, 110, S326–S330.
- Hoffman, B.L.; Felter, E.M.; Chu, K.-H.; Shensa, A.; Hermann, C.; Wolynn, T.; Williams, D.; Primack, B.A. It’s not all about autism: The emerging landscape of anti-vaccination sentiment on Facebook. Vaccine 2019, 37, 2216–2223.
- Bonnevie, E.; Smith, S.M.; Kummeth, C.; Goldbarg, J.; Smyser, J. Social media influencers can be used to deliver positive information about the flu vaccine: Findings from a multi-year study. Health Educ. Res. 2021, 36, 286–294.
- Kalichman, S.C.; Eaton, L.A.; Earnshaw, V.A.; Brousseau, N. Faster than warp speed: Early attention to COVD-19 by anti-vaccine groups on Facebook. J. Public Health 2022, 44, e96–e105.
- Hou, Z.; Tong, Y.; Du, F.; Lu, L.; Zhao, S.; Yu, K.; Piatek, S.J.; Larson, H.J.; Lin, L. Assessing COVID-19 vaccine hesitancy, confidence, and public engagement: A global social listening study. J. Med. Internet Res. 2021, 23, e27632.
- Jamison, A.M.; Broniatowski, D.A.; Dredze, M.; Sangraula, A.; Smith, M.C.; Quinn, S.C. Not just conspiracy theories: Vaccine opponents and proponents add to the COVID-19 ‘infodemic’on Twitter. Harv. Kennedy Sch. Misinform. Rev. 2020, 1.
- Donzelli, G.; Palomba, G.; Federigi, I.; Aquino, F.; Cioni, L.; Verani, M.; Carducci, A.; Lopalco, P. Misinformation on vaccination: A quantitative analysis of YouTube videos. Hum. Vaccines Immunother. 2018, 14, 1654–1659.
- Espinosa, L.; Wijermans, A.; Orchard, F.; Höhle, M.; Czernichow, T.; Coletti, P.; Hermans, L.; Faes, C.; Kissling, E.; Mollet, T. Epitweetr: Early warning of public health threats using Twitter data. SSRN 2021, 397, 3811673.
- Leonard, N.R.; Casarjian, B.; Fletcher, R.R.; Prata, C.; Sherpa, D.; Kelemen, A.; Rajan, S.; Salaam, R.; Cleland, C.M.; Gwadz, M.V. Theoretically-based emotion regulation strategies using a mobile app and wearable sensor among homeless adolescent mothers: Acceptability and feasibility study. JMIR Pediatrics Parent. 2018, 1, e9037.
- Ming, L.C.; Untong, N.; Aliudin, N.A.; Osili, N.; Kifli, N.; Tan, C.S.; Goh, K.W.; Ng, P.W.; Al-Worafi, Y.M.; Lee, K.S. Mobile health apps on COVID-19 launched in the early days of the pandemic: Content analysis and review. JMIR mHealth uHealth 2020, 8, e19796.
- Lattie, E.G.; Cohen, K.A.; Hersch, E.; Williams, K.D.; Kruzan, K.P.; MacIver, C.; Hermes, J.; Maddi, K.; Kwasny, M.; Mohr, D.C. Uptake and effectiveness of a self-guided mobile app platform for college student mental health. Internet Interv. 2022, 27, 100493.
- Davalbhakta, S.; Advani, S.; Kumar, S.; Agarwal, V.; Bhoyar, S.; Fedirko, E.; Misra, D.; Goel, A.; Gupta, L.; Agarwal, V. A systematic review of the smartphone applications available for coronavirus disease 2019 (COVID19) and their assessment using the mobile app rating scale (MARS). medRxiv 2020.
- Huang, Z.; Guo, H.; Lim, H.Y.-F.; Chow, A. Determinants of the acceptance and adoption of a digital contact tracing tool during the COVID-19 pandemic in Singapore. Epidemiol. Infect. 2022, 150, e54.
- Tsvyatkova, D.; Buckley, J.; Beecham, S.; Chochlov, M.; O’Keeffe, I.R.; Razzaq, A.; Rekanar, K.; Richardson, I.; Welsh, T.; Storni, C. Digital Contact Tracing Apps for COVID-19: Development of a Citizen-Centered Evaluation Framework. JMIR mHealth uHealth 2022, 10, e30691.
- Majeed, M.T.; Khan, F.N. Do information and communication technologies (ICTs) contribute to health outcomes? An empirical analysis. Qual. Quant. 2019, 53, 183–206.
- Becker, E.R.; Shegog, R.; Savas, L.S.; Frost, E.L.; Coan, S.P.; Healy, C.M.; Spinner, S.W.; Vernon, S.W. Parents’ Experience with a Mobile Health Intervention to Influence Human Papillomavirus Vaccination Decision Making: Mixed Methods Study. JMIR Pediatrics Parent. 2022, 5, e30340.
- Muñoz-Ramírez, S.; Escribano-López, B.; Rodrigo-Casares, V.; Vergara-Hernández, C.; Gil-Mary, D.; Sorribes-Monrabal, I.; Garcés-Sánchez, M.; Muñoz-Del-Barrio, M.-J.; Albors-Fernández, A.-M.; Úbeda-Sansano, M.-I. Feasibility of a hybrid clinical trial for respiratory virus detection in toddlers during the influenza season. BMC Med. Res. Methodol. 2021, 21, 273.
- Antonelli, M.; Penfold, R.S.; Merino, J.; Sudre, C.H.; Molteni, E.; Berry, S.; Canas, L.S.; Graham, M.S.; Klaser, K.; Modat, M. Risk factors and disease profile of post-vaccination SARS-CoV-2 infection in UK users of the COVID Symptom Study app: A prospective, community-based, nested, case-control study. Lancet Infect. Dis. 2022, 22, 43–55.
- Fahy, N.; Williams, G.A. Use of Digital Health Tools in Europe: Before, during and after COVID-19; European Observatory on Health Systems and Policies: Copenhagen, Denmark, 2021.
- Arias-Oliva, M.; Pelegrín-Borondo, J.; Almahameed, A.A.; Andrés-Sánchez, J.d. Ethical Attitudes toward COVID-19 Passports: Evidences from Spain. Int. J. Environ. Res. Public Health 2021, 18, 13098.
- Morley, J.; Cowls, J.; Taddeo, M.; Floridi, L. Ethical Guidelines for COVID-19 Tracing Apps; Nature Publishing Group: Berlin, Germany, 2020.
- Bengio, Y.; Ippolito, D.; Janda, R.; Jarvie, M.; Prud’homme, B.; Rousseau, J.-F.; Sharma, A.; Yu, Y.W. Inherent privacy limitations of decentralized contact tracing apps. J. Am. Med. Inform. Assoc. 2020, 28, 193–195.
- Vandamme, A.-M.; Nguyen, T. Belgium--concerns about coronavirus contact-tracing apps. Nature 2020, 581, 384–385.
- Godinho, M.A.; Martins, H.; Al-Shorbaji, N.; Quintana, Y.; Liaw, S.-T. “Digital Health Diplomacy” in Global Digital Health? A call for critique and discourse. J. Am. Med. Inform. Assoc. 2021, 29, 1019–1024.
- Zeng, K.; Bernardo, S.N.; Havins, W.E. The use of digital tools to mitigate the COVID-19 pandemic: Comparative retrospective study of six countries. JMIR Public Health Surveill. 2020, 6, e24598.
- Grande, D.; Mitra, N.; Marti, X.L.; Merchant, R.; Asch, D.; Dolan, A.; Sharma, M.; Cannuscio, C. Consumer views on using digital data for COVID-19 control in the United States. JAMA Netw. Open 2021, 4, e2110918.
- Khan, M.L.; Malik, A.; Ruhi, U.; Al-Busaidi, A. Conflicting attitudes: Analyzing social media data to understand the early discourse on COVID-19 passports. Technol. Soc. 2022, 68, 101830.
- Ye, G.; Hudders, L.; De Jans, S.; De Veirman, M. The value of influencer marketing for business: A bibliometric analysis and managerial implications. J. Advert. 2021, 50, 160–178.
- Childers, C.C.; Lemon, L.L.; Hoy, M.G. #Sponsored# Ad: Agency perspective on influencer marketing campaigns. J. Curr. Issues Res. Advert. 2019, 40, 258–274.
- Glucksman, M. The rise of social media influencer marketing on lifestyle branding: A case study of Lucie Fink. Elon J. Undergrad. Res. Commun. 2017, 8, 77–87.
- Lou, C.; Yuan, S. Influencer marketing: How message value and credibility affect consumer trust of branded content on social media. J. Interact. Advert. 2019, 19, 58–73.
- Gough, A.; Hunter, R.F.; Ajao, O.; Jurek, A.; McKeown, G.; Hong, J.; Barrett, E.; Ferguson, M.; McElwee, G.; McCarthy, M. Tweet for behavior change: Using social media for the dissemination of public health messages. JMIR Public Health Surveill. 2017, 3, e6313.
- Byrne, E.; Kearney, J.; MacEvilly, C. The role of influencer marketing and social influencers in public health. Proc. Nutr. Soc. 2017, 76, E103.
- Navarro, M.A.; O’Brien, E.K.; Ganz, O.; Hoffman, L. Influencer prevalence and role on cigar brand Instagram pages. Tob. Control. 2021, 30, e33–e36.
- La Fauci, V.; Mondello, S.; Squeri, R.; Alessi, V.; Genovese, C.; Laudani, N.; Cattaruzza, M. Family, lifestyles and new and old type of smoking in young adults: Insights from an italian multiple-center study. Ann Ig 2021, 33, 131–140.
- Ortiz, R.R.; Smith, A.; Coyne-Beasley, T. A systematic literature review to examine the potential for social media to impact HPV vaccine uptake and awareness, knowledge, and attitudes about HPV and HPV vaccination. Hum. Vaccines Immunother. 2019, 15, 1465–1475.
- Chen, F.; Stevens, R. Applying lessons from behavioral economics to increase flu vaccination rates. Health Promot. Int. 2017, 32, 1067–1073.
- Priebe Rocha, L.; Soares, C.; McGregor, A.; Chen, S.; Kaplan, A.; Rose, R.R.; Galvão, H.; Siqueira, C.E.; Allen, J.D. Understanding health priorities, behaviors, and service utilization among Brazilian immigrant women: Implications for designing community-based interventions. J. Racial Ethn. Health Disparities 2022, 9, 135–145.
- Hong, Y.A.; Yee, S.; Bagchi, P.; Juon, H.-S.; Kim, S.C.; Le, D. Social media-based intervention to promote HBV screening and liver cancer prevention among Korean Americans: Results of a pilot study. Digit. Health 2022, 8, 20552076221076257.
- Massaro, M.; Tamburro, P.; La Torre, M.; Dal Mas, F.; Thomas, R.; Cobianchi, L.; Barach, P. Non-pharmaceutical interventions and the infodemic on Twitter: Lessons learned from Italy during the COVID-19 Pandemic. J. Med. Syst. 2021, 45, 50.
- Arora, S.; Bø, B.; Tjoflåt, I.; Eslen-Ziya, H. Immigrants in Norway: Resilience, challenges and vulnerabilities in times of COVID-19. J. Migr. Health 2022, 5, 100089.
- Xu, L.; Tang, F.; Chen, Y.; Dong, X. Acculturation and depressive symptoms among older Chinese immigrants in the United States: The roles of positive and negative social interactions. Aging Ment. Health 2022, 26, 1–8.
More
