Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Sirius Huang and Version 1 by Akila Anandarajah.
Mobile mammography is a tool that has been used to reach underserved women in a diverse number of settings, including urban, rural, and mountain regions. The mobile mammography van, affiliated with Siteman Cancer Center Breast Health Center, acts as part of outreach efforts to increase breast screening rates in medically underserved communities including the St. Louis area (urban) as well as the rural Bootheel region of Missouri. The van reached a particularly vulnerable population that was mostly poor, uninsured, and with limited educational backgrounds regardless of their zip code of service.
- breast cancer
- community-based participatory research
- health disparities
- mobile mammography
1. Introduction
Breast cancer continues to be the most commonly diagnosed cancer in the United States, and it is the second leading cause of death among women in the United States. A proven method to reduce breast cancer mortality is mammography, with a 15–30% reduction in breast cancer specific mortality, depending on the age of the patient [2][1]. This reduction in mortality is based on mammography’s ability to detect clinically asymptomatic breast cancers at an early stage, leading to early diagnosis and initiation of treatment. Despite the proven effectiveness of mammography, the most recent data from National Health Interview Survey reports demonstrated that only 70.7% of women between the ages of 45–64 had completed a mammogram within two years, which was significantly below the Healthy People 2030 goal of 77.1% [3,4][2][3]. Factors associated with not having undergone a mammogram included lower educational attainment, lower income, and not having insurance.
2. Mobile Mammography Van
Part of the challenge in achieving breast health equity is bringing mammography closer to the women who need it. Missouri officially has 114 counties and one independent city (St. Louis), of which only 14 counties are designated as urban, while the other 101 are considered rural. Overall, the rate of mammography screening within the last two years for women over the age of 40 in Missouri is 71%, compared to a national average of 72% [23][4]. However, previous data has shown that within St. Louis City, the screening rate is 69.5% [10][5]. Additionally, studies have demonstrated that rates of breast cancer screening among rural women tend to be lower than those for urban women [24][6]. As a result, any efforts to increase mammographic screening rates in Missouri will face the challenge of confronting barriers encountered by women residing in both urban and rural populations. The mobile unit, affiliated with Siteman Cancer Center Breast Health Center, attempted to do just this by visiting sites in the St. Louis area (urban) as well as the rural Bootheel region of Missouri and addressing the Breast Cancer Community Partnership priorities.
Mobile mammography is a tool that has been used to reach underserved women in a diverse number of settings, including urban, rural, and mountain regions [25,26][7][8]. Community-academic partnerships between providers and community-based and faith-based organizations are an evidence-based approach for using mobile mammography to increase screening rates among racial and ethnic minorities, uninsured, medically underserved and women of low socioeconomic status [25][7]. Partnerships are effective in linking patients with mammography service as self-referral for mobile mammography may not optimally benefit or reach medically underserved women most in need of breast cancer screening [27][9]. Furthermore, results from a randomized controlled trial showed that women who were offered on-site mobile mammography in addition to health education were significantly more likely than those in the education-only group to undergo mammography sooner (within three months) [28][10].
The Breast Health Center is housed within the Siteman Cancer Center and provides on-site service as well as off-site care through the use of a single mobile mammography van. Each day, this van goes to one location and serves women for the entire day. The van endeavors to visit three types of site locations in equal proportions throughout the month on a regular schedule. The site location categories are (1) community sites (grocery stores, YMCAs, and libraries), (2) corporate sites, and (3) outreach sites (FQHCs, well established health fairs, churches, etc.). Identification of community and outreach sites are determined based on data that identified “hot spots,” areas within St. Louis and surrounding counties that had particularly high rates of late-stage breast cancer at diagnosis. The van’s site schedule is continually evaluated to determine its effectiveness in breast cancer screening. The clinical service and PECaD and its analysts collaborate in evaluation efforts to optimally serve the community. In addition, community engagement has enhanced and informed the mammography van approach. For example, after disparities in late-stage breast cancer diagnosis and mortality were identified in the north county [29][11], following BCaP recommendations, north county mammography van visits were subsequently increased. Valeda’s Hope, which was created by a CRFT alumnus, and The Breakfast Club are two local community organizations that have worked to increase the number of women making use of the van in the region. Many strategies, including providing community education and scheduling opportunities ahead of the van’s visit, developing marketing materials that specifically invited uninsured women to be screened, and using breast health navigators to connect uninsured women with various breast cancer screening/treatment grant programs, have been employed to ensure the success of the van.
An outreach registry of patients served by the Breast Health Center (BHC) was created for program evaluation and planning purposes. Patients included in the database were uninsured or underinsured women that received screening care with funding from a Show Me Healthy Women grant, a program under the National Breast and Cervical Cancer Early Detection Program that provides free breast and cervical cancer screenings for women in Missouri with incomes at or below 200% of the federal poverty level who are aged 35–64 or older if they do not have Medicare Part B and have no insurance coverage for program services, or the Susan G. Komen Foundation grant. The registry data includes data from medical records and responses to a brief questionnaire completed at each visit. We examined data for the first screening visit of women that were seen on the mobile mammography van between April 2006 and December 2011. Data was examined by point of care (urban/rural) to assess the efficacy of mobile mammography as an outreach strategy in each of these environments.
Data analysis was conducted using SAS 9.3 (SAS Institute Inc., Cary, NC, USA); statistical significance was assessed at a p-value <0.05. Univariate analyses were used to examine categorical demographic characteristics such as age, income, race/ethnicity, education, employment status, marital status, insurance status, and living environment proxy (urban/suburban—St. Louis City/County, rural—Bootheel/other MO) using frequencies and percentages. Age was also examined continuously and summarized by the mean and standard deviation (Table 1). Bivariate associations were examined using chi-square tests to compare demographics between urban/suburban and rural living environment proxy. ArcGIS was used to map the number of women who received their first screening mammogram on the mobile unit and the number of times the unit visited each zip code between 2006 and 2011.
Table 1.
Demographic characteristics of sample.
| Total n = 8292 | n | % |
|---|
There were a total of 14,208 imaging records from 10,218 individual females in the BHC database from April 2006 to December 2011. During this period, 9789 women were enrolled in the registry for their first screening visit and 85% (n = 8289) received their care on the mobile mammography van. Thirty-four percent who presented were non-Hispanic White, 55% were non-Hispanic Black, 3% were Hispanic, and 9% were categorized as other race/ethnicity. The majority of women were in the 46–55 age group (mean = 52 years, SD = 8.9). Most (87%) had an annual income less than $20,000, had 12 years of education (45.1%) or less (31.1%), were unemployed (68%), uninsured (70%), and not married (72%). It was the first screening for 77% of women (Table 2).
Table 2.
Bivariate association between demographics and urban versus rural comparison.
| STL City/County —Urban/Suburban |
Bootheel/Other MO —Rural |
Chi-Square p-Value |
||||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | |||||
| Age (mean, SD) | ||||||||
| Age | (52.21, 8.86) | |||||||
| 6903 | 1273 | 38.37 df 4 | p < 0.001 |
21–39 | 82 | 1.0 | ||
| 21–39 | 56 | 0.8 | 25 | 2.0 | 40–45 | 2056 | 24.8 | |
| 40–45 | 1688 | 24.5 | 339 | 26.6 | 46–55 | 3517 | 42.4 | |
| 56–65 | ||||||||
| 46–55 | 29272016 | 24.3 | ||||||
| 42.4 | 543 | 42.6 | 66+ | |||||
| 56–65 | 1676 | 24.3621 | 7.5 | |||||
| Annual Income 3-levels | 472 | 124 | 9.86 df 2 p = 0.007 |
|||||
| <$10,000 | 232 | 49.2 | 46 | |||||
| 6903 | ||||||||
| 84.4 | ||||||||
| 313 | ||||||||
| Bootheel/other MO—Rural | ||||||||
| 1273 | ||||||||
| 15.6 | ||||||||
| 24.6 | ||||||||
| 66+ | 556 | 8.0 | 53Annual Income 3-levels (n = 604) | |||||
| <$10,000 | 283 | 46.9 | ||||||
| 37.1 | $10,000–$20,000 | 240 | 39.7 | |||||
| $20,000+ | 81 | 13.4 | ||||||
| Race/Ethnicity (n = 8290) | ||||||||
| Non-Hispanic White | 2785 | 33.6 | ||||||
| Non-Hispanic Black | 4529 | 54.6 | ||||||
| Hispanic | 267 | 3.2 | ||||||
| Other | ||||||||
| $10,000–$20,000 | 186 | 39.4 | 52 | 41.9 | ||||
| $20,000+ | 54 | 11.4 | 26 | 21.0 | ||||
| Highest Grade | 512 | 124 | 3.69 df 2 p = 0.158 |
|||||
| 0–11 | 161 | 31.4 | 38 | 30.7 | 709 | 8.6 | ||
| Single visit | 6367 | |||||||
| 12 | 223 | 43.6 | 64 | 51.6 | ||||
| 13–16 | 128 | 76.8 | ||||||
| Multiple visits | 1925 | 23.2 | ||||||
1 Grades 0–11 represent a less than high school education, 12 represents graduating high school, and 13–16 represents attending some college or having a college degree.
| 4.2 | ||||||||
| 25.0 | ||||||||
| 22 | ||||||||
| 17.7 | ||||||||
| Race 4-categories | ||||||||
| 6901 | ||||||||
| 1273 | 1479.03 df 3 | p | < 0.001 | |||||
| Highest Grade Completed 1 (n = 639) | ||||||||
| Non-Hispanic White | 1720 | 24.9 | 993 | 78.0 | 0–11 | 199 | 31.1 | |
| Non-Hispanic Black | 4376 | 63.4 | 122 | 9.6 | 12 | 288 | 45.1 | |
| Hispanic | 220 | 3.2 | 40 | 3.1 | 13–16 | 152 | 23.8 | |
| Other | 585 | 8.5 | 118 | 9.3 | Currently Unemployed | 5667 | 68.3 | |
| Currently Unemployed | 4701 | 68.1 | 899 | 70.6 | 3.16 df 1 p = 0.075 |
Not Married (n = 7694) | 5558 | 72.2 |
| Married | 1572 | 24.2 | 512 | 47.1 | 245.60 df 1 p < 0.001 |
No Insurance coverage (n = 8279) | 5769 | 69.7 |
| No Insurance coverage | 4644 | 67.3 | 1044 | 82.9 | 122.45 df 1 p < 0.001 |
Urban proxy (n = 8176) | ||
| Single visit | 5190 | 75.2 | 1077 | 84.6 | 53.27 df 1 p < 0.001 |
St. Louis City/County—Urban/Suburban | ||
| Multiple visits | 1713 | 24.8 | 196 | 15.4 |
The GIS maps show a wide outreach area for a single mobile unit. The highest numbers of women served were seen in the zip codes closer to the Siteman Cancer Center and in the rural Bootheel region of Missouri. However, the reach of mobile mammography was seen in women who reside in zip codes closer to Springfield, MO (approximately 200 miles from St. Louis) and across the state border in Illinois zip codes (Figure 1). Furthermore, it is interesting to note the large number of women served in the Bootheel region, despite the few number of mobile unit visits to that region.
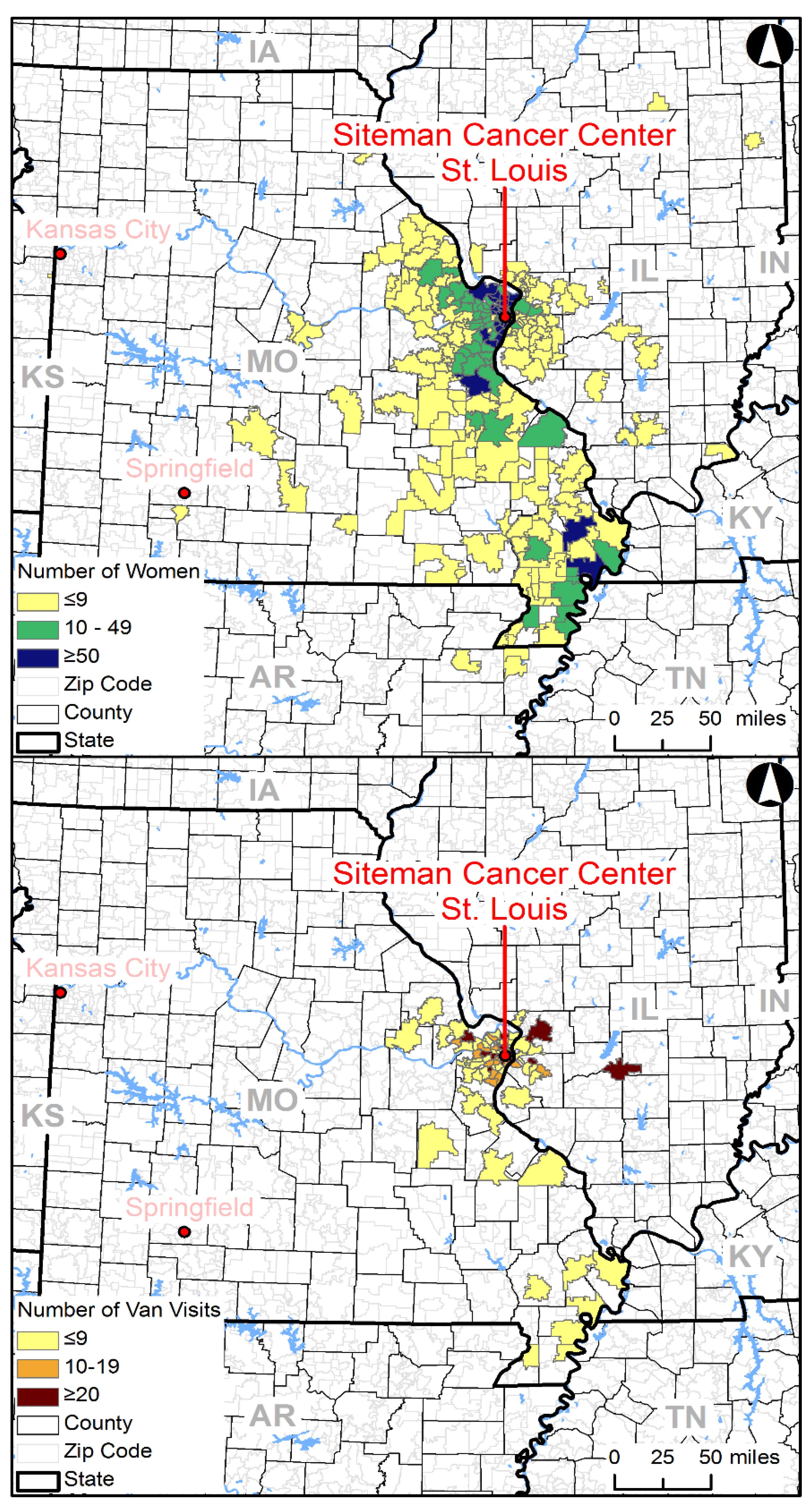
Figure 1.
Number of women served (top) and van visits (bottom) by zip code.
The mobile mammography van improved access to breast cancer screening among a largely vulnerable uninsured population at risk for poor health due to being medically underserved, reaching women in both urban and rural areas in Missouri. Additionally, it successfully engaged economically disadvantaged women in medically underserved areas including women without health insurance who had never had a mammogram, and those with a family history of breast cancer.
While a larger percentage of the rural sample reported an income of greater than $20,000 (21.0%) as compared to the urban sample (11.4%), the vast majority of women in both groups were poor with incomes less than $20,000 (urban: 88.6% vs. rural: 79%). This is not an unexpected finding. However, it highlights an opportunity for both the education and recruitment of this particular population, as many of these women may be eligible for programs specifically for breast cancer screening based on income alone. For example, Show Me Healthy Women covers low-income women who are uninsured or underinsured. In addition, Medicaid in Missouri covers low-income individuals and families.
The majority of women in both groups had a high school education or less (urban: 75% vs. rural: 82.3%). This is actually a notable finding, because it means that the van is reaching a population of women that has traditionally been extremely underserved. Rates of mammographic screening in women aged 50–74 with less than a high school education was 69.4% and was 73.2% among those who have graduated from high school, both of which are beneath the national average [30][12]. Furthermore, prior research has also demonstrated that a decreased general understanding of breast cancer, and not just screening alone, contributes to lower mammography rates [31][13]. While the data demonstrates that this mobile mammography van is reaching a particularly vulnerable population, one must be mindful that this success is not from merely the presence of the van, but also likely from the significant community education that occurred as well.
While there are certainly a few differences between urban and rural women served by the mobile mammography unit, the mobile unit predominantly serves a portion of the female population that is usually defined as medically underserved and “hard to reach”. These women are mostly poor, uninsured, and with limited educational backgrounds regardless of their zip code of service.
Support for components of the program have fluctuated over time, including changes with Medicaid, support for navigation, capacity, and organization priorities. To sustain decreases in the cancer burden, ongoing monitoring of services and resources is needed to ensure that access is sustained. Show Me Healthy Women faces barriers for providers to implement and maintain the program and is chronically underfunded, adding challenges to sustaining hospital engagement.
References
- Nelson, H.D.; Tyne, K.; Naik, A.; Bougatsos, C.; Chan, B.K.; Humphrey, L. Screening for breast cancer: An update for the U.S. Preventive Services Task Force. Ann. Intern. Med. 2009, 151, 727–737.
- Gorina, Y.; Elgaddal, N. Patterns of Mammography, Pap Smear, and Colorectal Cancer Screening Services among Women Aged 45 and Over. Natl. Health Stat. Rep. 2021, 1–18. Available online: https://www.ncbi.nlm.nih.gov/pubmed/34181518 (accessed on 19 January 2022).
- Healthy People 2030. Increase the Proportion of Females Who Get Screened for Breast Cancer—C-05. Available online: https://health.gov/healthypeople/objectives-and-data/browse-objectives/cancer/increase-proportion-females-who-get-screened-breast-cancer-c-05 (accessed on 19 January 2022).
- Kaiser Family Foundation. Women Age 40 and Older Who Report Having Had a Mammogram within the Past Two Years by Race/Ethnicity. Available online: https://www.kff.org/womens-health-policy/state-indicator/mammogram-rate-for-women-40-years/ (accessed on 22 January 2022).
- Lian, M.; Jeffe, D.B.; Schootman, M. Racial and geographic differences in mammography screening in St. Louis City: A multilevel study. J. Urban Health 2008, 85, 677–692.
- Orwat, J.; Caputo, N.; Key, W.; De Sa, J. Comparing Rural and Urban Cervical and Breast Cancer Screening Rates in a Privately Insured Population. Soc. Work Public Health 2017, 32, 311–323.
- Kamaraju, S.; DeNomie, M.; Visotcky, A.; Banerjee, A.; Krause, K.; Tavares, E.; Rao, A.; Drew, E.; Neuner, J.; Stolley, M. Increasing Mammography Uptake Through Academic-Community Partnerships Targeting Immigrant and Refugee Communities in Milwaukee. WMJ 2018, 117, 55–61. Available online: https://www.ncbi.nlm.nih.gov/pubmed/30048573 (accessed on 19 January 2022).
- Gardner, T.; Gavaza, P.; Meade, P.; Adkins, D.M. Delivering free healthcare to rural Central Appalachia population: The case of the Health Wagon. Rural Remote Health 2012, 12, 197–203. Available online: https://www.ncbi.nlm.nih.gov/pubmed/22452285 (accessed on 19 January 2022).
- Peek, M.E.; Han, J. Mobile mammography: Assessment of self-referral in reaching medically underserved women. J. Natl. Med. Assoc. 2007, 99, 398–403. Available online: https://www.ncbi.nlm.nih.gov/pubmed/17444429 (accessed on 19 January 2022).
- Reuben, D.B.; Bassett, L.W.; Hirsch, S.H.; Jackson, C.A.; Bastani, R. A randomized clinical trial to assess the benefit of offering on-site mobile mammography in addition to health education for older women. AJR Am. J. Roentgenol. 2002, 179, 1509–1514.
- Saint Louis County Department of Public Health. Cancer Profile St. Louis County, Missouri; Saint Louis County Department of Public Health: Berkeley, MO, USA, 2019.
- National Cancer Institute. Breast Cancer Screening. Available online: https://progressreport.cancer.gov/detection/breast_cancer (accessed on 19 January 2022).
- Ahmed, N.U.; Fort, J.G.; Fair, A.M.; Semenya, K.; Haber, G. Breast cancer knowledge and barriers to mammography in a low-income managed care population. J. Cancer Educ. 2009, 24, 261–266.
More
