Technological innovation has enabled the development of machine learning (ML) tools that aim to improve the practice of radiologists. In the last decade, ML applications to neuro-oncology have expanded significantly, with the pre-operative prediction of glioma grade using medical imaging as a specific area of interest.
- clinical implementation. Keywords: artificial intelligence
- glioma
- machine learning
- deep learning
1. Introduction
1.1. Artificial Intelligence, Machine Learning, and Radiomics
1.2. Machine Learning Applications in Neuro-Oncology
As the most common primary brain tumors, gliomas constitute a major focus of ML applications to neuro-oncology [7][8][7,8]. Prominent domains of glioma ML research include the image-based classification of tumor grade and prediction of molecular and genetic characteristics. Genetic information is not only instrumental to tumor diagnosis in the 2021 World Health Organization classification, but also significantly affects survival and underpins sensitivity to therapeutic interventions [9][10][9,10]. ML-based models for predicting tumor genotype can therefore guide earlier diagnosis, estimation of prognosis, and treatment-related decision-making [11][12][11,12]. Other significant areas of glioma ML research relevant to neuroradiologists include automated tumor segmentation on MRI, detection and prediction of tumor progression, differentiation of pseudo-progression from true progression, glioma survival prediction and treatment response, distinction of gliomas from other tumors and non-neoplastic lesions, heterogeneity assessment based on imaging features, and clinical incorporation of volumetrics [13][14][15][13,14,15]. Furthermore, ML tools may optimize neuroradiology workflow by expediting the time to read studies from image review to report generation [16]. As an image interpretation support tool, ML importantly may improve diagnostic performance [17][18][17,18].2. Algorithms for Glioma Grade Classification
The most common high-performing ML classifiers for glioma grading in the literature are SVM and CNN [13]. SVM is a classical ML algorithm that represents objects as points in an n-dimensional space, with features serving as coordinates. SVMs use a hyperplane, or an n-1 dimensional subspace, to divide the space into disconnected areas [19][40]. These distinct areas represent the different classes that the model can classify. Unlike CNNs, SVMs require hand-engineered features, such as from radiomics, to serve as inputs. This requirement may be advantageous for veteran diagnostic imagers, whose knowledge of brain tumor appearance may enhance feature design and selection. Hand-engineered features also can undergo feature reduction to mitigate the risks of overfitting, and prior works demonstrate better performance for glioma grading models using a smaller number of quantitative features [20][41]. However, hand-engineered features are limited since they cannot be adjusted during model training, and it is uncertain if they are optimal features for classification. Moreover, hand-engineered features may not generalize well beyond the training set and should be tested extensively prior to usage [21][22][42,43]. CNNs are a form of deep learning based on image convolution. Images are the direct inputs to the neural network, rather than the manually engineered features of classical ML. Numerous interconnected layers each compute feature representations and pass them on to subsequent layers [22][23][43,44]. Near the network output, features are flattened into a vector that performs the classification task. CNNs appeared for glioma grading in 2018 and have risen quickly in prevalence while exhibiting excellent predictive accuracies [24][25][26][27][45,46,47,48]. To a greater extent than classical ML, they are suited for working with large amounts of data, and their architecture can be modified to optimize efficiency and performance [25][46]. Disadvantages include the opaque “black box” nature of deep learning and associated difficulty with interpreting model parameters, along with problems that variably apply to classical ML as well (e.g., high amount of time and data required for training, hardware costs, and necessary user expertise) [28][29][49,50].3. Challenges in Image-Based ML Glioma Grading
3.1. Data Sources
Since 2011, a significant number of ML glioma grade prediction studies have used open-source multi-center datasets to develop their models. BraTS [30][52] and TCIA [31][53] are two prominent public datasets that contain multi-modal MRI images of high- and low-grade gliomas and patient demographics. BraTS was first made available in 2012, with the 2021 dataset containing 8000 multi-institutional, multi-parametric MR images of gliomas [30][52]. TCIA first went online in 2011 and contains MR images of gliomas collected across 28 institutions [31][53]. These datasets were developed with the aim of providing a unified multi-center resource for glioma research. A variety of predictive models have been trained and tested on these large datasets since their 2011 release [32][54]. Despite their value as public datasets for model development, several limitations should be considered. Images are collected across multiple institutions with variable protocols and image quality. Co-registration and imaging pre-processing integrate these images into a single system.3.2. External Validation
4.2. External Validation
Publications have reported predictive models for glioma grading throughout the last 20 years with the majority relying on internal validation techniques, of which cross-validation is the most popular. While internal validation is a well-established method for measuring how well a model will perform on new cases from the initial dataset, additional evaluation on a separate dataset (i.e., external validation) is critical to demonstrate model generalizability. External validation mitigates site bias (differences amongst centers in protocols, techniques, scanner variability, level of experience, etc.) and sampling/selection bias (performance only applicable to the specific training set population/demographics) [33][55]. Not controlling for these two major biases undermines model generalizability, yet few publications externally validate their models [13]. Therefore, normalizing external validation is a crucial step in developing glioma grade prediction models that are suitable for clinical implementation.3.3. Glioma Grade Classification Systems
4.3. Glioma Grade Classification Systems
The classification of glioma subtypes into high- and low-grade gliomas is continuously evolving. In 2016, an integrated histological–molecular classification replaced the previous purely histopathological classification [34][56]. In 2021, the Consortium to Inform Molecular and Practical Approaches to CNS Tumor Taxonomy (cIMPACT NOW) once more accentuated the diagnostic value of molecular markers, such as the isocitrate dehydrogenase mutation, for glioma classification [35][57]. As a result of the evolving glioma classification system, definitions for high- and low-grade gliomas vary across ML glioma grade prediction studies and publication years. This reduces the comparability of models themselves and grade-labeled datasets used for model development. Current and future ML methods must keep abreast of the rapid progress in tissue based integrated diagnostics in order to contribute to and make an impact on the clinical care of glioma patients (Figure 12).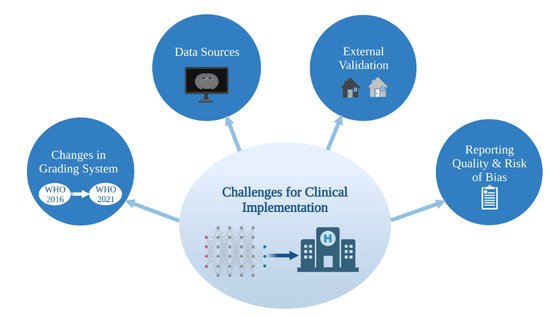
3.4. Reporting Quality and Risk of Bias
4.4. Reporting Quality and Risk of Bias
34.4.1. Overview of Current Guidelines and Tools for Assessment
Clear and thorough reporting enables more complete understanding by the reader and unambiguous assessment of study generalizability, quality, and reproducibility, encouraging future researchers to replicate and use models in clinical contexts. Several instruments have been designed to improve the reporting quality (defined here as the transparency and thoroughness with which authors share key details of their study to enable proper interpretation and evaluation) of studies developing models. The Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis (TRIPOD) Statement was created in 2015 as a set of recommendations for studies developing, validating, or updating diagnostic or prognostic models [36][58]. The TRIPOD Statement is a checklist of 22 items considered essential for transparent reporting of a prediction model study. In 2017, with a concurrent rise in radiomics-based model studies, the radiomics quality score (RQS) emerged [37][59]. RQS is an adaptation of the TRIPOD approach geared toward a radiomics-specific context. The tool has been used throughout the literature for evaluating the methodological quality of radiomics studies, including applications to medical imaging [38][60]. Radiomics-based approaches for interpreting medical images have evolved to encompass the AI techniques of classical ML and, most recently, deep learning models. Most recently, in recognition of the growing need for an evaluation tool specific to AI applications in medical imaging, the Checklist for AI in Medical Imaging (CLAIM) was published in 2020 [39][61]. The 42 elements of CLAIM aim to be a best practice guide for authors presenting their research on applications of AI in medical imaging, ranging from classification and image reconstruction to text analysis and workflow optimization. Other tools—the Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2) tool [40][62] and Prediction model Risk Of Bias ASsessment Tool (PROBAST) [41][63]—importantly evaluate the risk of bias in studies based on what is reported about their models. Bias relates to systematic limitations or flaws in study design, methods, execution, or analysis that distort estimates of model performance [40][62]. High risk of bias discourages adaptation of the reported model outside of its original research context, and, at a systemic level, undermines model reproducibility and translation into clinical practice.
34.4.2. Reporting Quality and Risk of Bias in Image-Based Glioma Grade Prediction
34.4.3. Future of Reporting Guidelines and Risk of Bias Tools for ML Studies
Efforts by authors to refine how they report their studies depend upon existing reporting guidelines. In their systematic review, Yao et al. identified substantial limitations to neuroradiology deep learning reporting standardization and reproducibility [43][65]. They recommended that future researchers propose a reporting framework specific to deep learning studies. This call for an AI-targeted framework parallels contemporary movements to produce AI extensions of established reporting guidelines.45. Future Directions
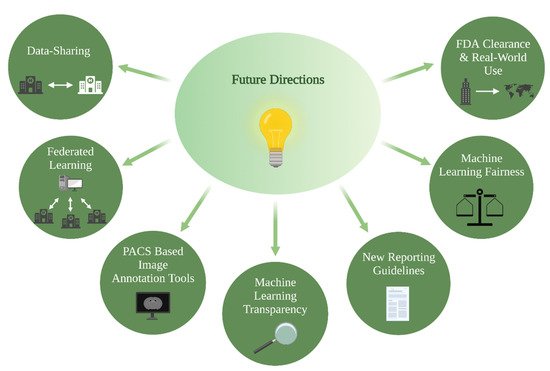
ML models present an attractive solution towards overcoming current barriers and accelerating the transition to patient-tailored treatments and precision medicine. Novel algorithms combine information derived from multimodal imaging to molecular markers and clinical information, with the aim of bringing personalized predictions on a patient level into routine clinical care. Relatedly, multi-omic approaches that integrate a variety of advanced techniques such as proteomics, transcriptomics, epigenomics, etc., are increasingly gaining importance in understanding cancer biology and will play a key role in the facilitation of precision medicine [44][45][70,71]. The growing presence of ML models in research settings is indisputable, yet several strategies should be considered to facilitate clinical implementation: PACS-based image annotation tools, data-sharing and federated learning, ML fairness, ML transparency, and FDA clearance and real-world use (Figure 23).