in relation to some factors such as the effect of age, diet and others on its composition and stability. S
Several studies suggest the importance of preserving the micro-ecosystem of commensal, symbiotic and pathogenic microbes of the respiratory system, and, more recently, its relationship with the intestinal microbiome.
However, recent studies investigate how it leads to the maintenance of human health, also in relation to some factors such as the effect of age, diet and others, making its composition and stability better understood.
- human microbiome
- respiratory microbiome
- clinical microbiology
- immune modulation
- dysbiosis
- respiratory diseases
- translational research
- SARS-CoV-2
1. Content
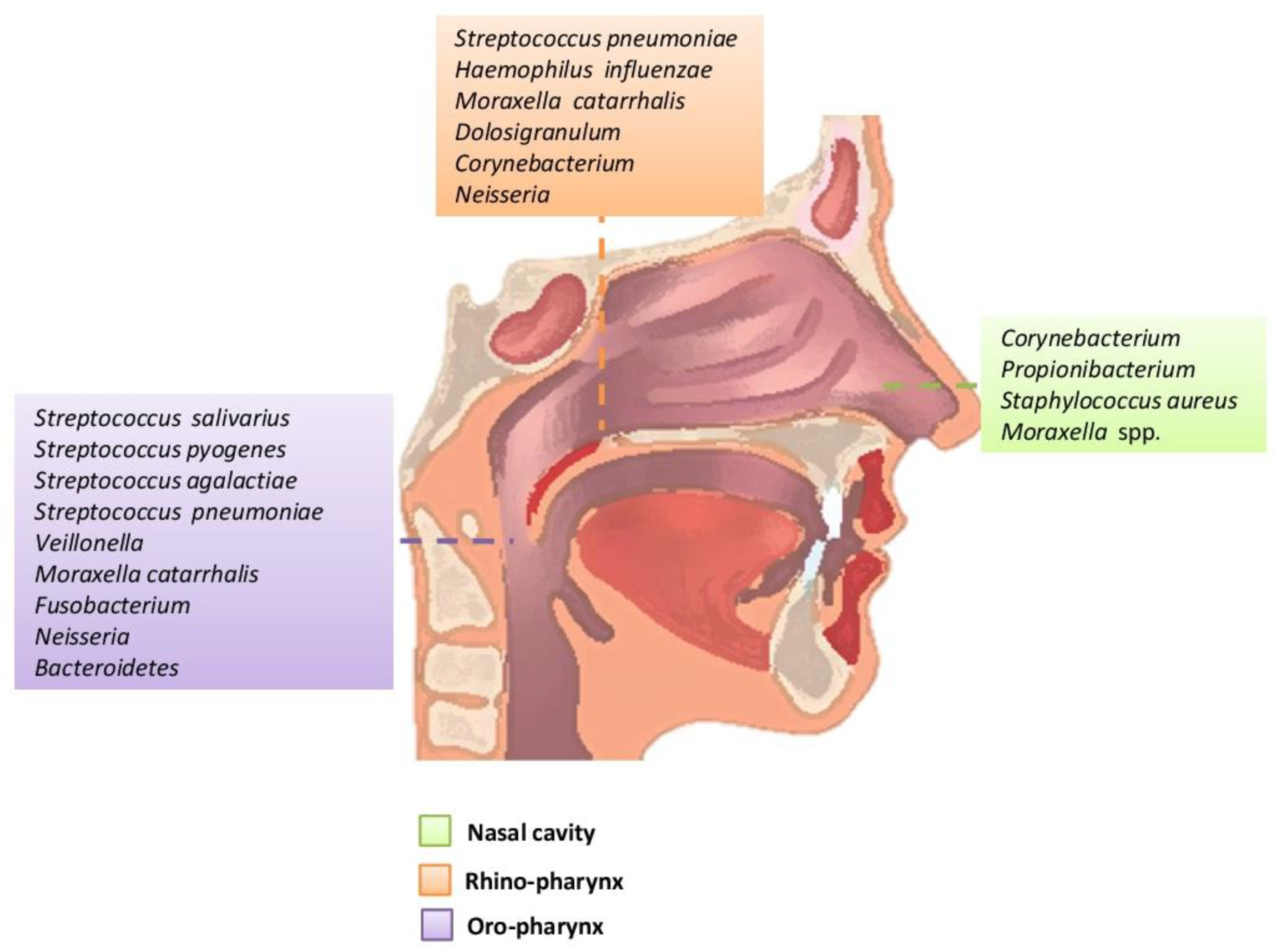
Figure 1. Main bacteria genera and microbiome species of an adult in the upper respiratory tract.
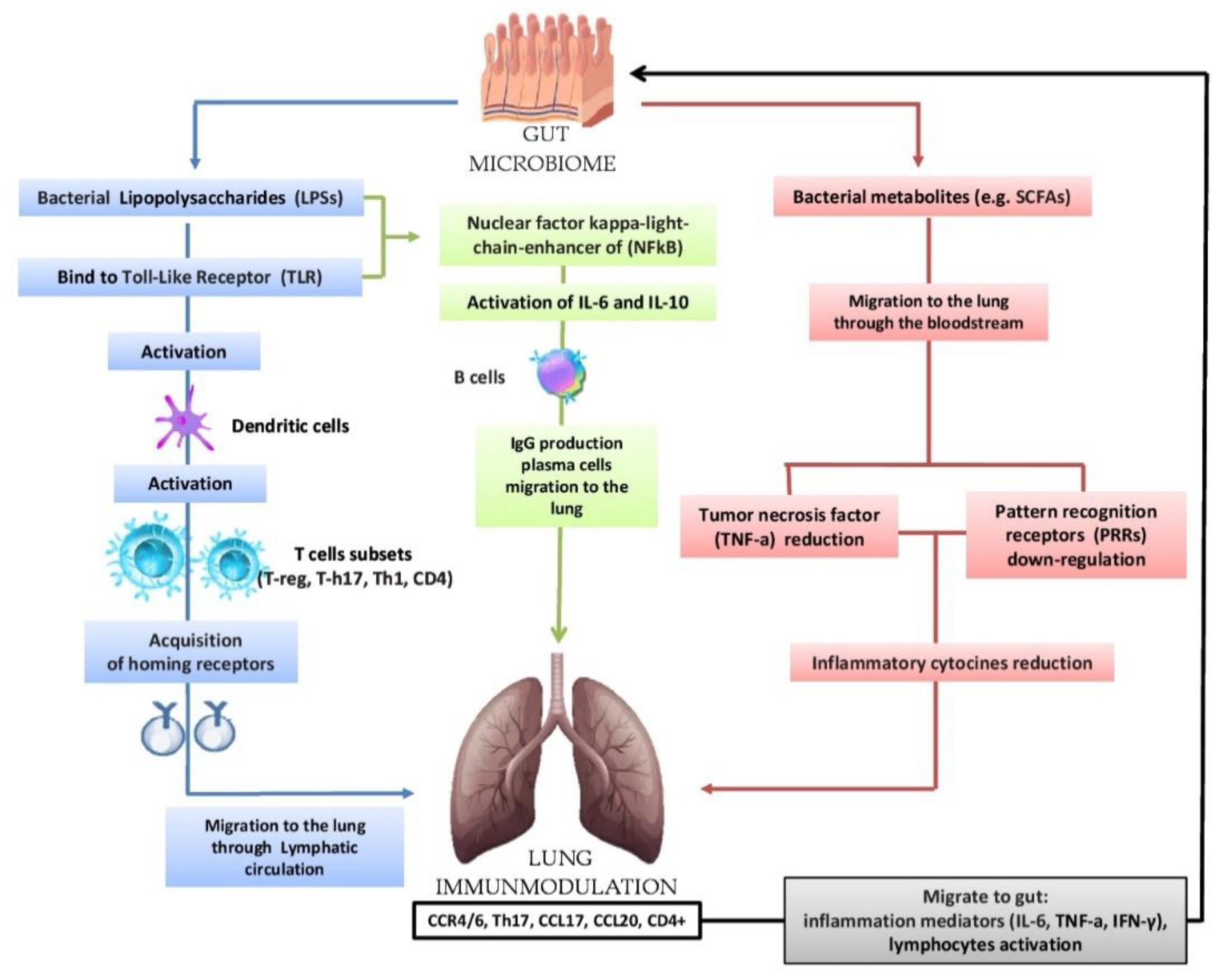
Figure 2. Bidirectional hypothesis that the intestinal microbiota can modulate the immunological activity of the lung: lipopolysaccharides (LPSs) are able to bind to the Toll-Like Receptor (TLR) present on the intestinal mucosa causing the activation of dendritic cells that favor the activation of various T cells (T-reg, T-h17, Th-1, CD4); subsequently, there is the acquisition of horning receptors (CCR6, CCR9, CCR4, a4b7) and migration to the lung through the circulatory lymphatic flow (CCR4/6Treg, CCR4/6Th17, CCR4/6Th1, CCR4/6CD4 +). It also activates (IL-18, INF-y, TNF-a, TGF-b, IL-4, IL-1), which will pass into the circulation (INF-y, TNF-a, IL-6). The nuclear factor kappa-light chain enhancer of (NFkB) activates IL-6, IL-10 and the production of IgA and IgG plasma cell b cells and the migration of IgG to the lung. In the lung, we have the increase in CCL17, CCL20 and the presence of CCR4/6, CD4 +, CCR4/6 and Th17. The migration of bacterial metabolites (e.g., short-chain fatty acids (SCFAs) to the lung through the bloodstream results in the down-regulation of pattern recognition receptors (PRR) with a consequent reduction in the production of inflammatory cytokines (IL-1, IL-12, IL-18), tumor necrosis factor alpha (TNF-α), interferon gamma (IFNγ) and granulocyte–macrophage colony stimulating factor (GM-CSF). In turn, the lungs send inflammation mediators and lymphocytes to the gut in case of disease.
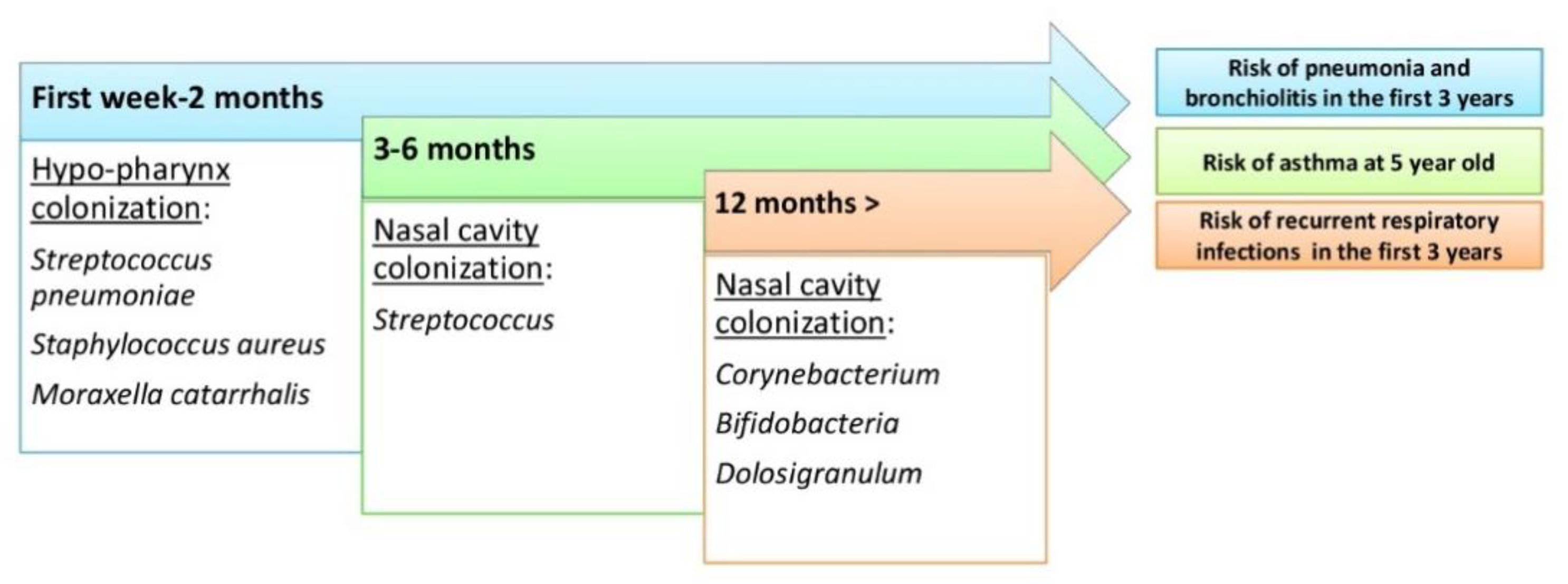
Figure 3. The evolution of the upper respiratory tract microbiome during human life and risk of respiratory tract diseases.
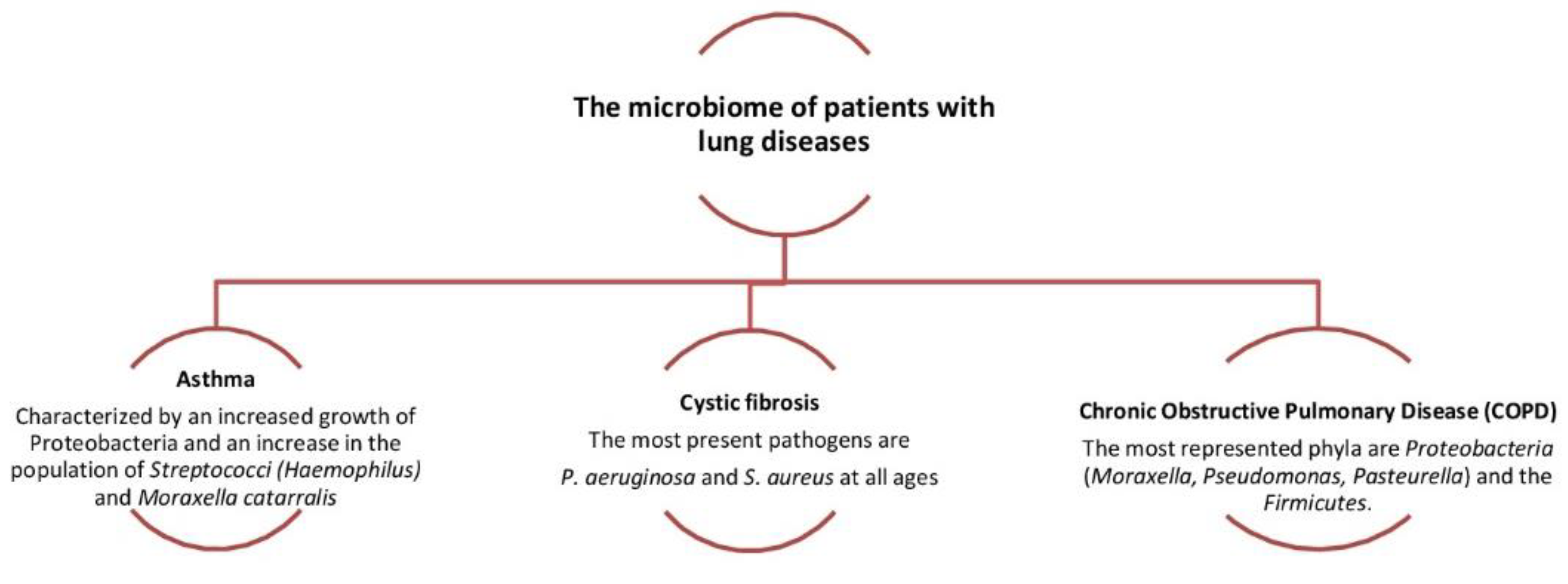
Figure 4. Dysbiosis related to some lung diseases. The relative abundance in Proteobacteria is associated with the increased severity of chronic obstructive pulmonary disease (COPD).
