Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Cameron David Ryall and Version 2 by Nora Tang.
Application of modern delivery techniques to natural bioactive products improves their permeability, bioavailability, and therapeutic efficacy. Many natural products have desirable biological properties applicable to wound healing but are limited by their inability to cross the stratum corneum to access the wound. Over the past two decades, modern systems such as microneedles, lipid-based vesicles, hydrogels, composite dressings, and responsive formulations have been applied to natural products such as curcumin or aloe vera to improve their delivery and efficacy.
- wound healing
- natural products
- advanced delivery
- traditional medicine
- alternative medicine
1. TIME and TWA: Deciding on a Treatment
A key focus in today’s conventional treatment of wounds is managing the risk of a wound becoming chronic [1][18]. A wound should only require treatment if its natural healing is stalled or interrupted. The ‘TIME’ or ‘TWA’ processes are used to assess the wound and determine a treatment. No single treatment is applied to all wounds; hence, assessing wounds and making evidence-based decisions is emphasised [1][2][18,19]. Both TIME and TWA are acronyms. For TIME, T stands for ‘tissue non-viable or deficient’, I for ‘infection or inflammation’, M for ‘moisture balance’, and E for ‘edge of wound—non-advancing or undermined’ [1][3][18,20]. TWA stands for ‘Triangle of Wound Assessment’ [4][5][21,22]. TWA elaborates on TIME with a three-point ‘triangle’: wound bed, wound edge, and peri-wound skin [5][22]. TWA and TIME analysis provide a systematic way to analyse a wound and direct clinicians to the proper treatment.
2. Wound-Healing Dressings
The most common and historically present product for a wound is its dressing. The primary function of a dressing is to protect against foreign microbes and protect the skin from exudate [4][6][21,23]. It is often desirable for a dressing to be absorbent, particularly when a wound has too much exudate interfering with the patient’s daily life or creating too friendly an environment for bacteria to colonise [3][20]. Absorbents can be fibrous, fabric, or a combination of the two: these forms are among the most accessible wound dressings around the world [2][19]. Modern technologies have added to this category with hydrofibres and impregnated gauzes, which are more bioactive than their fibre/fabric counterparts [6][23]. Such direct dressings can have the disadvantage of being painful when removed, hence the use of non-adherent dressings. Non-adherent dressings are often preferred for the contact layer dressing as they do not attach to the wound’s tissue. Non-adherence allows the protection of granulation tissue and the epithelium at the expense of requiring a secondary dressing to secure the wound [2][5][19,22].
Water-based formations such as hydrogels and hydrocolloids are applied to wounds requiring a moist environment to heal. Hydrogels use hydrophilic polymers to attract water and create a three-dimensional network in the form of a gel. Hydrogels can be used to rehydrate a wound bed, rehydrate necrotic tissue, absorb excess exudate, or reduce pain [2][6][7][19,23,24]. Hydrogels can be loaded with bioactive compounds to deliver it directly to the wound area in a relatively painless manner. An available hydrogel is Curasol™ which is applied to an absorbent layer such as cotton or gauze and then taped, netted, or bandaged onto the wound. Hydrogel dressings often market themselves based on their pain relief and rehydrating abilities—one problem with these products is the complicated application that requires a healthcare professional [8][25]. Hydrogels are commonly applied to traditional medicine and are often fabricated using polymers derived from nature [9][10][11][26,27,28]. The polymers applied to hydrogels are becoming increasingly advanced; Yan et al. formulated a thermosensitive hydrogel that released a phage to combat bacterial infections. This hydrogel could be infected as a liquid but would form into a hydrogel dressing once exposed to the temperature of an inflamed wound bed [12][29]. Hydrocolloid dressings such as alginates have the advantage of requiring no secondary dressing. Hydrocolloid dressings are gel-forming agents that absorb and retain fluid to create a wound-moistening gel [7][13][24,30]. Hydrocolloids, like hydrogels, can be loaded with antiseptics or wound-healing drugs to make them bioactive. Hydrocolloid dressings derived from sodium alginate taken from brown seaweed are commonly used for wounds with excess exudate because of their absorptive properties. Other hydrocolloids such as Duoderm™ can be used for shallow acute wounds with little exudate present [7][14][24,31]. Hydrocolloids and hydrogels reduce pain sensation by keeping nerve endings moist and providing a provisional ECM to facilitate autolysis [7][13][24,30].
Semipermeable dressings such as foams and films can protect wounds from the external environment while allowing essential molecules to enter. Foams fabricated from polyurethane or silicone can protect against bacteria and moisten the wound bed while avoiding tissue damage when removed [15][32]. Foams are also used to encapsulate drugs and have been applied with natural products such as asiaticoside from Centella asiatica [16][33]. Recent advances in foams for wound care combine other technologies to create responsive/smart dressings. A multi-layer dressing made from an anti-microbial foam and an electrospun cellulose surface mesh was formulated by He et al. which changes colour in response to infection-caused pH changes [17][34]. Films are like foams by being semipermeable but are more often applied to epithelizing wounds with little exudate. Oxygen and carbon dioxide can pass through films but, similarly to foams, bacteria or pathogens are kept away. Koetse et al. and Babikian et al. have innovated different films for wound care which can record electrical signals in a wound [18][19][35,36]. Both devices aimed to capture a wide range of physiological parameters using impedance, current, and other parameters.
Another dressing that aids wound healing is bioadhesives. These adhere to the site of a wound to moisten, absorb exudate, and protect from external pathogens [20][37]. These can be injected as hydrogels which then adhere to the surface of a wound or be delivered as a patch placed similarly to a plaster [21][38]. Figure 12 shows how a bioadhesive can cover a wound bed. Bioadhesives must be biocompatible and biodegradable; thus, they are often derived from nature. One bioadhesive formulated by Ke et al. used two natural products in tannic acid and silk fibroin to help develop the ECM and protect against bacterial infection [22][39]. Table 1 summarizes the many kinds of wound dressing. Many of these dressings are being made using natural compounds because of their biocompatibility and biodegradability; thus, it is a promising field for natural products in wound care [23][40].
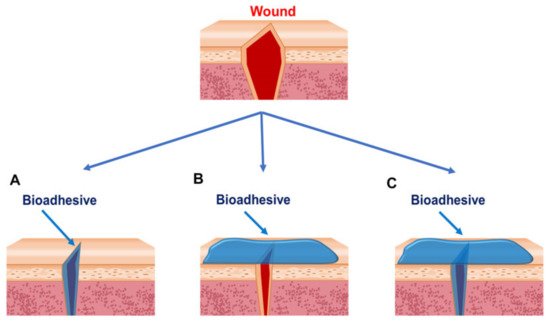
Figure 12. Strategies for bioadhesives used to close wounds. (A) Bioadhesives are applied between wound edges. (B) Bioadhesives are applied outside of the wounds. (C) Bioadhesives are applied between and outside the wounds. Reprinted with permission from Ref. [20][37].
Table 1. Characteristics of wound dressings.
Characteristics of wound dressings.
| Type of Wound Dressing | Features | Limitations | Product Name | References |
|---|---|---|---|---|
| Film dressings | Elastic, durable, comfortable, and conform well to body contours Waterproof and transparent Create a moist healing environment Bacterial and viral barrier Semi-permeable to water vapour and gas |
Adhesive films might disrupt newly formed epithelium during dressing change Limited use for highly exuding wounds Might develop leakage channels |
Tegaderm™ (3M™, UK Plc.) Opsite Films® (Smith and Nephew) Mepitel®Film (Mölnlycke Health Care Limited) |
[15][17][24][32,34,41] |
| Foam dressings | Highly absorbent Easily removable Create a moist healing environment Bacterial and viral barrier Semi-permeable to water vapour and gas |
Form an opaque layer, making wound monitoring difficult Limited use for dry wounds Poor stability |
Flexsan Biopatch Biatain Cultinova Lyofoam Allevyn Unilene Tielle CuraSpon Kendall Hydrasorb |
[16][25][33,42] |
| Hydrogel dressings | Create a moist healing environment Pain relief Self-applied or injectable Facilitate autolytic debridement Easily removed |
Require a secondary dressing Lack of mechanical strength Inconsistent hydration properties Poor bacterial barrier |
Suprasorb® AquaDerm™ Neoheal® Simpurity™ DermaGauze™ Restore |
[26][27][28][43,44,45] |
| Bioadhesive dressings | Create a moist healing environment Self-injectable Adhesive |
Unremovable Interference with other medical devices Might develop leakage channels |
Ligate™ | [20][37] |
