Cancer is among the leading causes of death worldwide. In recent years, many cancer-associated biomarkers have been identified that are used for cancer diagnosis, prognosis, screening, and early detection, as well as for predicting and monitoring carcinogenesis and therapeutic effectiveness. Phosphatidylserine (PS) is a negatively charged phospholipid which is predominantly located in the inner leaflet of the cell membrane. In many cancer cells, PS externalizes to the outer cell membrane, a process regulated by calcium-dependent flippases and scramblases. Saposin C coupled with dioleoylphosphatidylserine (SapC-DOPS) nanovesicle (BXQ-350) and bavituximab, (Tarvacin, human–mouse chimeric monoclonal antibodies) are cell surface PS-targeting drugs being tested in clinical trial for treating a variety of cancers. Additionally, a number of other PS-selective agents have been used to trigger cytotoxicity in tumor-associated endothelial cells or cancer cells in pre-clinical studies.
- cancer biomarkers
- phosphatidylserine
- saposin C
- dioleoylphosphatidylserine
- SapC-DOPS
- electric field
- cancer imaging
- enhanced cancer therapy
1. Introduction: Biomarkers in Cancer Imaging and Therapy
2. PS: Cellular Distribution and Roles
While only 3–10% of all cellular lipids [19][24], PS is found in both prokaryotic and eukaryotic cells and plays crucial roles in a variety of cellular activities including presynaptic neurotransmitter release, post-synaptic receptor activity, mitochondrial membrane integrity and stimulation of protein kinase C in memory generation [20][21][22][25,26,27]. Normal cells exhibit most of their PS on the cytosolic side of the cell membrane (Figure 1). PS transfer between inner and outer cell membranes is regulated by a group of ATPases, and amino phospholipid translocases (flippases) [23][28]. Exposure of PS is classically known as a marker of apoptotic cells, where PS acts as a “eat me” signal for PS receptors on immune cells and leads to clearance of the cells by macrophages [24][29]. PS also plays a role in immune modulation. It is known that PS exposure on cancer cells also leads to immunosuppression in the tumor microenvironment, where it increases the activity of natural killer and dendritic cells and shifts the polarization of tumor-associated macrophages (TAMs) into anti-inflammatory (M2) macrophages [25][26][30,31].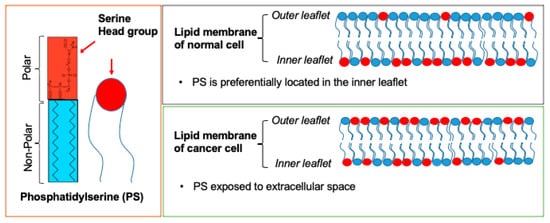
3. PS as a Cancer Biomarker
3.1. Heterogeneity in Surface PS Exposure on Membranes May Indicate a Susceptibility of Cancer Cells to Cancer Treatments at Different Stages
In contrast to the normal cells, cancer cells are unable to preserve PS asymmetry, leading to the surface exposure of PS on cell membranes [18][27][18,32] (Figure 1). The extent of PS exposure on the outer cell membrane differs significantly between different types of cancer cells. Interestingly, this variability is seen even within the same cancer type. For instance, while one subset of cells in a cell line demonstrates limited surface PS exposure, another subset of cells from the same cell line exposes high PS on cell membranes [18]. Cancer cells with low surface PS appear to be more sensitive to irradiation and chemotherapies such as gemcitabine (Gemzar)/nab-paclitaxel (Abraxane) [28][29][33,34]. On the other hand, cancer cells with higher surface PS are more sensitive to PS-targeting anticancer treatments, including saposin C embedded in a dioleoylphosphatidylserine nanovesicle (SapC-DOPS) [28][29][30][33,34,35]. PS is also a driver of cancer metastasis and immune escape [24][29]. Moreover, there is a positive correlation between surface PS exposure of tumors and their malignancy [31][36]. Therefore, the level of surface PS exposure on cancer cells may be important for diagnostic differentiation between different stages of the cancer and/or the susceptibility of the cancer to various treatments. Monitoring cell surface PS is a compelling approach to quantitatively assess tumor growth and progression because the standard cancer treatments, including chemotherapy and radiotherapy, can increase surface PS on endothelial and stromal cells in the tumor. Successful PS-targeted cancer cell imaging has been demonstrated by using different carriers [32][33][37,38]. Antibodies that specifically target PS, such as bavituximab and PGN635 (fully human PS-specific monoclonal antibody) and PS-binding annexins have been used in pre-clinical studies as imaging agents, as summarized in Table 1.| PS-Targeting Imaging | ||||
|---|---|---|---|---|
| Type of Imaging Modality | PS-Targeting Antibody + Imaging Compound | Results | Cancer Type(s) | Refs. |
| Optical Imaging | Annexin V-Cy | A 2- to 3-fold stronger near-infrared fluorescent signal was observed in tumors of mice once treated with pro-apoptotic drug, cyclophosphamide. | Gliosarcoma | [34][39] |
| Optical Imaging | PGN635+ 800CW | Successfully imaged the tumor 4 h post-IV injection of PGN635-800 CW. Highest signal observed at 24 h. |
Glioblastoma | [35][40] |
| Positron Emission Tomography (PET) | PGN635 + 89Zr | High accumulation 89Zr-PGN635 in treated tumors undergoing apoptosis. Tumor-to-blood ratios of up to 13. |
Human colorectal cancer Breast cancer |
[32][37] |
| PET | 74As-labeled bavituximab | Tumor–liver ratio was 22 for bavituximab compared with 1.5 for an isotype matched control chimeric antibody 72 h after injection. | Prostate cancer | [36][41] |
| Magnetic resonance imaging (MRI) (9.4T) | PGN635 + Superparamagnetic iron oxide nanoparticles (SPIO) | T2-weighted MRI detected a drastic reduction in signal intensity and T2 values of tumors at 24 h. | Breast cancer | [33][38] |
3.2. SapC-DOPS Nanovesicles Can Target Cancer Surface PS
Different cancer cell lines can also be monitored using a system that includes PS and SapC, which is an endogenous sphingolipid activator protein that plays an important role in lysosomal enzyme activation and sphingosine and ceramide generation from sphingolipid degradation [42][43][44][45][46][47][48][47,48,49,50,51,52,53]. SapC has strong binding affinity for PS at an acidic pH [44][45][46][47][49][50][49,50,51,52,54,55]. It is known that tumors express abundant PS on the cell surface and have a lower extracellular pH (pH~6) than normal tissues (pH~7) due to lactate secretion from anaerobic glycolysis [51][56]. Therefore, the SapC-PS interaction provides a valuable, highly selective system for targeted tumor imaging and therapy. Previous studies have shown that nanovesicles comprised of SapC and DOPS, SapC-DOPS can selectively target tumor cells [19][29][42][52][53][54][55][56][57][24,34,47,57,58,59,60,61,62]. ReseaOurchers' group has also shown that contrast agent-loaded SapC-DOPS nanocarriers can be used to monitor and trace different cancer cell lines [56][58][61,63]. Successful imaging of cancer cells with the PS-targeting SapC-DOPS nanocarrier system has been reported using optical, magnetic resonance imaging (MRI), as well as single-photon emission computed tomography (SPECT) [19][59][60][24,64,65], as described below. Figure 2 shows a schematic representation of SapC-based imaging modalities.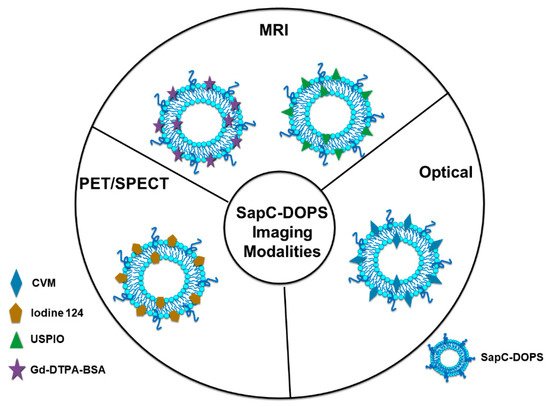
3.2.1. Optical Cancer Imaging Using PS-Targeting SapC-DOPS Nanovesicles
Optical imaging has been widely used in pre-clinical cancer research [61][62][66,67]. In particular, it is utilized to conduct research on cancer markers, drug pharmacodynamics and to examine the effects of drugs in small animals [63][68]. The allure strength of optical imaging is that it is economical, easy to manage, and provides real-time results. CellVue Maroon (CVM) is a far-red fluorophore and Chu et al. [64][69] demonstrated that CVM- tagged SapC-DOPS nanovesicles can be utilized for detecting brain tumors and arthritic joints in mice. A rotational bed was used to obtain the multi-angle rotational optical image. The results confirmed that optical imaging intensity depends on the optical imaging angle, which varies with cancer type in different animal models. For example, the values for the optical imaging angle in orthotopic and mut49 tumor-bearing mouse models were determined to be 10° and 20°, respectively. In the same study, Chu et al. showed that SapC-DOPS nanovesicle-based optical imaging not only provided information about the disease or the cancer site, it also enabled assessment of disease state and/or cancer progression [64][69]. Similar results have been reported by Kaimal et al. in their mouse xenograft models of pancreatic adenocarcinoma, neuroblastoma and a murine rhabdomyosarcoma model [59][64]. However, while optical imaging is highly sensitive, it has significant limitations. For example, optical imaging techniques have limited utility in human patients due to challenges associated with signal detection of fluorescence probes in deep tissues. Another limitation is autofluorescence that is generated in animal/human tissue and in ingested food. Studies are ongoing to circumvent these limitations; thus, Blanco et al. (see Section 3.2.3) demonstrated that phenol-substituted membrane-intercalating lipophilic dyes and conjugated iodinated lipophilic dyes can be incorporated into SapC-DOPS, allowing dual imaging of glioblastoma (optical and PET imaging) [56][61].3.2.2. Magnetic Resonance Imaging (MRI) Using PS-Targeting SapC-DOPS Nanovesicles
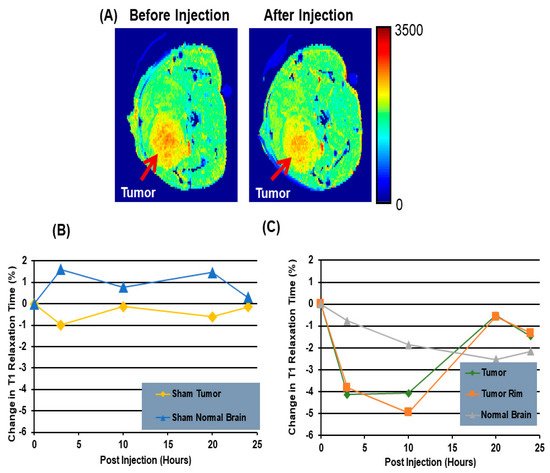
MRI is a broadly used method for tumor detection. Even though its sensitivity is low, MRI has exceptional soft tissue contrast and excellent spatial resolution [65][70]. MRI was used to selectively image neuroblastoma by utilizing iron oxide particles encapsulated inside SapC-DOPS nanocarriers [59][64]. By tagging these vesicles with ultrasmall superparamagnetic iron oxide contrast agent (USPIO) particles, Kaimal and his-coworkers monitored both in vitro and in vivo delivery and uptake of the SapC-DOPS-IO vesicles. According to the in vitro results, there is a significant increase on the R2 and R2* relaxation rates (14.64 s−1, 26.74 s−1) once the cells are exposed to SapC-DOPS-IO for 24 h as compared to the control cells (7.84 s−1, 11.04 s−1). According to an in vivo study conducted in mice, T2*-weighted imaging at 7T shows that the signal intensity in tumors drops immediately after injection of SapC-DOPS-IO, followed by a gradual further decrease before rebounding slightly 24 h later. The drop in signal intensity is observed throughout the tumor. Inductively coupled plasma atomic emission spectroscopy (ICP-AES) analysis shows that the concentration of iron in the tumor of a mouse injected with SapC-DOPS-IO is approximately 5-fold higher than the concentration of iron in the tumor of a free IO-treated mouse [59][64]. Winter et al. used paramagnetic gadolinium chelates, gadolinium-DTPA-bis(stearylamide) (Gd-DTPA-BSA)-loaded SapC-DOPS vesicles as a targeted contrast agent for imaging glioblastoma multiform tumors [58][63]. At 7T, Gd-DTPA-BSA/SapC-DOPS vesicles and Gd-DTPA display a similar relaxivity of 3.32 and 2.80 (s·mM)−1, respectively. According to the in vivo experiments using injection of Gd-DTPA-BSA/SapC-DOPS vesicles, the R1 values before the injection of the tumor, contralateral normal brain, and sham-injected brain were 0.4676 ± 0.010 s−1, 0.5596 ± 0.003 s−1 and 0.5216 ± 0.034 s−1, respectively. Following the injection, the average change in the tumor R1 value was 9.0 ± 2.3% (p < 0.05) at 10 h post-injection, whereas the normal brain and the sham-injected brain showed no significant change, 1.2 ± 1.5% and 1.4 ± 1.9% (p > 0.05). The tumor R1 was increased (7.9 ± 1.5%, p < 0.05) compared to that for the normal and sham brains at 20 h post-injection, and it became statistically indistinguishable from the controls at 24 h post-injection (4.7 ± 2.0%, p > 0.05). Figure 3A shows the T1 maps of tumor cells before treatment and after 10 h injection of Gd-DTPA-BSA/SapC-DOPS vesicles. The results indicate that there is a clear reduction in the T1 relaxation time 10 h after treatment with Gd-DTPA-BSA/SapC-DOPS vesicles as compared with the T1 value before the injection. Figure 3B shows the percent change in T1 relaxation of sham tumor and sham normal brain treated with only SapC DOPS. At 4, 10, and 20 h, the increase in T1 relaxation time is higher in the sham normal brain, as compared with that in the sham tumor. By 24 h post-injection, the T1-weighted signal is similar in both tissues. Figure 3C shows the percent change in T1 relaxation after injection of Gd-DTPA-BSA/SapC-DOPS vesicle. At 4 and 10 h post-injection, the T1 relaxation time change is higher in the tumor (−4.12%, −4.05%) and the tumor rim (−3.81%, −4.94%), as compared with the T1 relaxation time change for the normal brain (−0.76%, −1.84%).