1. Mesothelin as a New Cancer Biomarker for the Diagnosis and Prognosis of Ovarian Carcinomas
To the best of
the reseaour
chers' knowledge, there have been no immunohistochemical studies to date reporting a correlation between prognosis and the expression pattern of M
esothelin (MSLN) in high-grade serous ovarian carcinoma (HSOC)SLN in HSOC. In addition,
the researchers we did not find any studies that correlated the co-expression of MSLN and CA125 with prognosis in HSOC. However, in an immunohistochemical analysis of a cohort of 40 serous endometrial carcinoma cases, Kakimoto et al. observed that all 18 cases with the co-expression of these molecules had a worse prognosis compared to those without co-expression
[1][46]. In
the our
esearchers' opinion, additional studies are necessary to elucidate whether the different patterns of MSLN immunoreactivity and co-expression with CA125 also have the same prognostic significance in HSOC in order to provide useful data to inform treatment procedures after surgical therapy.
Moreover, for a subset of occult HSOC, which has not arisen from the ovarian epithelium but from a lesion of the distal end of the fallopian tube, called serous tubal intraepithelial carcinoma (STIC), prophylactic salpingo-oophorectomy (PSO) is currently recommended to reduce the cancer risk and make an early diagnosis
[2][3][4][47,48,49]. Clinically, it is very important to identify this subset of HSOC because complete surgery alone could cure affected patients, and even therapy using PARP inhibitors seems to be effective in cases at a high stage of development
[5][50].
STIC appears to be a precursor lesion for pelvic (tubal, ovarian, or primary peritoneal) high-grade serous carcinoma (HGSC) and is a non-invasive subtype of HGSC, usually located at the distal fimbriated end of the fallopian tube, often related to BRCA1 or BRCA2 mutations and associated with breast cancer
[3][4][5][6][7][48,49,50,51,52]. Upon pathological analysis, this lesion is extremely small and can be detected using a sectioning and extensively examining the fimbriated end (SEE-FIM) of the fallopian tube protocol and immunohistochemical analysis with specific antibodies, such as p53 and MIB-1
[8][53]. In the literature,
thwe
researchers did not find any studies that evaluated the expression levels of MSLN in STIC and high-grade serous ovarian carcinoma (HSOC) arising from this lesion. Intuitively, one might think that since the tubal epithelium is columnar, unlike that of the mesothelium, the STIC might not express mesothelin, and consequently HSOCs that arise from STIC might also be negative for MSLN in immunohistochemical and molecular analyses.
However,
thwe
researchers need to keep in mind that there is a broad range of tumour types, such as gastric, colorectal, oesophageal carcinomas, and synovial sarcoma, which although not arising from the mesothelium, can express MSLN
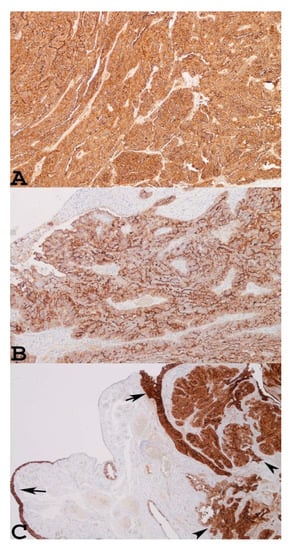
[9][33]. In addition, as shown in
Figure 1C, which refers to a case of STIC associated with small serous invasive carcinoma of the fimbria, both lesions showed marked positivity for MSLN upon immunohistochemical examination. Therefore, in
the our
esearchers' opinion, further studies with multiple cases of STIC, primary serous tubal carcinoma, and high-grade serous ovarian cancer associated with STIC or BRCA mutations should be investigated to clarify the role of MSLN in these malignancies and its impact on prognosis.
Figure 1. Two individual examples of advanced serous ovarian carcinoma showing diffuse mesothelin immunoreactivity: (A) score 4+, ×100; (B) score 3+, ×100. A personal example of STIC with a small nest of invasive serous carcinoma in a woman with BRCA-1 mutation and a previous history of breast cancer, showing strong immunoreactivity for MSLN in both lesions (C). Arrows indicate STIC, arrowheads indicate invasive serous carcinoma ×40.
2. Mesothelin as a Therapeutic Target
Currently, ovarian cancer treatment consists of surgical tumour debulking complemented with taxane- and platinum-based chemotherapy
[10][73], and occasionally supplemented with Avastin (bevacizumab, an antivascular endothelial growth factor therapy)
[11][74]. In advanced or recurrent disease, or in patients with a BRCA mutation, maintenance therapy with a poly adenosine diphosphate (ADP-ribose) polymerase (PARP) inhibitor is an effective treatment option
[12][75]. Thus, this subset of ovarian carcinoma is chemo-sensitive but a non-curable and indolent disease.
However, radical treatment regimens and multiple chemotherapeutic treatments do not reduce the recurrence of the disease nor the death rate of the patients. Given that MSLN is overexpressed in many solid tumours and has antigenic properties, this molecule could be considered an antigenic target for immunotherapeutic strategies in the treatment of ovarian carcinomas
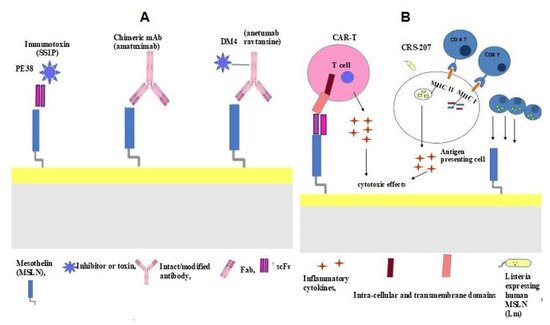
[13][76]. The main immunotherapeutic strategies that use different therapeutic agents include the anti-mesothelin immunotoxin SS1P, MORAb-009 (chimeric anti-mesothelin mAb), and the anti-mesothelin antibody–drug conjugate BAY-94 9343. Chimeric antigen receptor T cell (CAR T) therapy and vaccines have also been evaluated. The main immunotherapeutic strategies for ovarian cancer are summarised in
Figure 23A.
Table 12 lists the clinical trials of immunotherapeutic strategies for the treatment of ovarian carcinoma.
Figure 23. Schematic and simplified representation of the main therapeutic strategies that use mesothelin as a target. (A) PE translocated in cytosol and killed cells, catalysing protein synthesis and initiating programmed cell death. DM4 binding to tubulin disrupts the microtubule polymerisation, causing cell cycle arrest, apoptosis, and the killing of the dividing cells. (B) Attached to MSLN, CAR T cells become activated and stimulate the host immune system with the production of inflammatory cytokines. In CR-207, Listeria monocytogenes (Lm) and its antigens into the cytosol can be loaded onto major histocompatibility complex (MHC) I and MCH II, causing the activation of potent CD4 helper lymphocytes and CD8 cytotoxic lymphocytes, or activating pro-inflammatory genes, which can amplify the cytotoxic effect caused by inflammatory cytokines.
Table 12. Summary of clinical trials using MSLN target therapies for ovarian carcinoma.
| Clinical Trials gov Identifier |
Agent |
Phase |
Status |
Disease Setting |
Recruiting Centers |
| NCT00066651 |
SS1P |
I |
Completed |
Advanced Cervical, ovarian Fallopian tube, pacreatic, peritoneal, lung, head and neck cancer |
Unites States |
| NCT01521325 |
MORAb-009 (Chimeric Anti-Mesothelin mAb)
amatuximab |
I |
Completed |
Ovarian carcinoma, Mesothelioma, Pancreatic Cancer, Non Small Cell Lung |
United States |
| NCT01413451 |
MORAb-009 (Chimeric Anti-Mesothelin mAb)
amatuximab |
Early Phase I |
Terminated without efficacy in patienets with Ovarian Carcinoma |
Ovarian carcinoma Mesothelioma, Pancreatic Cancer, Non Small Cell Lung cancer expressing mesothelin |
United States |
| NCT01439152 |
BAY-94 9343
(Anti-MesothelinAntibody Drug Conjugate)
Anetumab ravtansine |
I |
Completed |
Invasive epithelial ovarian, primary serous peritoneal fallopian tube cancer |
United States |
| NCT02751918 |
BAY-94 9343
(Anti-MesothelinAntibody Drug Conjugate)
Anetumab ravtansine + pegyleted liposomal doxorubicin |
Ib |
Completed |
Invasive or metastatic, predominantly epithelial platinum-resistant ovarian, fallopian tube, or primary serous peritoneal cancer |
United States
Belgium
Moldova
Spain |
| NCT03814447 |
CAR-T-meso |
Early Phase I |
Recruitment |
Refractory-Relapsed Ovarian Cancer |
China |
| NCT03608618 |
CAR-T-meso+ intraperitoneal MCY-M11 |
Early Phase I |
Recruitment |
Advanced Ovarian cancer and mesthelioma |
United States |
| NCT00585845 |
CRS-207 |
I |
Terminated |
Ovarian Carcinoma, Mesothelioma, Non small-cell Lung carcinoma, Pancratic carcinoma, who have failed or who are not candidates for standard treatments |
United States |
| NCT02575807 |
CRS-207 + alfaPD-1 + IDO1 inhibitor (Epacadostat) |
I /II |
Terminated low enrollment and lack of cinical activity |
Platinum-resistant ovarian, fallopian or seous peritoneal cancer |
United States |
SS1P comprises an anti-MSLN immunotoxin obtained from immunised mice and fused to a truncated form of Pseudomonas exotoxin A (PE38) (
3A). SS1P binding to MSLN forms a complex that is internalised by endocytosis and PE, translocated in the cytosol, and kills the cells that catalyse protein synthesis, thereby initiating programmed cell death [77] ( 3A). In vitro studies have demonstrated the cytotoxic effect of SS1P on the neoplastic cells of patients affected by ovarian carcinomas [77]. In a phase I clinical trial ( identifier: NCT00066651), patients with ovarian carcinomas presented with stable disease.
The side effects of the treatment are dose-related and include capillary leak syndrome and pleuritis due to SS1P binding to normal mesothelial cells, as well as inflammation. The association with prednisone reduces the risk of toxicity, allowing for increased dosages
[15][78]. Moreover, in line with cases of mesothelioma, SS1P could be used in combination with chemotherapy to obtain a major response
[15][78]. However, as observed in treatments for mesotheliomas, it must be kept in mind that the efficacy of SS1P is limited by anti-drug antibody formation. Thus, SS1P is being administered in association with pentostatin and cyclophosphamide, which are lymphocyte-depleting drugs that allow patients to receive multiple cycles of treatments
[16][79].
2.2. MORAb-009 (Chimeric Anti-Mesothelin mAb)
MORAb-009 (chimeric anti-mesothelin mAb), also named amatuximab, is composed of the heavy- and light-chain variable regions of a mouse anti-mesothelin single-chain Fv grafted onto a human IgG1 and k constant region (
Figure 23A) (
Table 12). MORAb-009 has a high affinity for mesothelin, and a preclinical evaluation demonstrated that it could inhibit the adhesion between cell lines expressing mesothelin and MUC16 (CA125), as well as causing cell-mediated cytotoxicity in mesothelin-bearing tumour cells
[17][80]. In clinical trials, it was observed that patients treated with MORAb-009 showed a marked increase in CA125 serum levels, suggesting that it could block the binding between mesothelin and CA125. It was also demonstrated that MORAb-009 could inhibit cellular adhesion during metastasis in the case of both ovarian carcinomas and mesotheliomas
[18][81]. Studies in vivo on animal models demonstrated that these effects were markedly increased in combination with chemotherapy agents, such as gemcitabine and Taxol
[19][82], or in a phase II clinical trial with other chemotherapeutic substances for cases of mesotheliomas (
ClinicalTrials.gov identifier: NCT00738582)
[20][83].
The reduction in the MPF level in serum after treatment demonstrated a correlation with good prognosis
[20][83]. However, the combination with chemotherapy agents caused adverse events, such as hypersensitivity reactions, neutropenia, and atrial fibrillation
[20][83].
Although most studies (
ClinicalTrials.gov identifiers: NCT01521325, NCT01413451) on ovarian carcinomas have focused on the efficacy of monotherapy with MORAb-009, these data suggest that a combination with different chemotherapeutic agents could provide satisfactory results, with prolonged overall survival.
2.3. Anti-Mesothelin Antibody–Drug Conjugate (BAY-94 9343)
BAY-94 9343, known as anetumab ravtansine, is an anti-mesothelin antibody–drug conjugate (ADC) consisting of a fully human immunoglobulin G1 anti-mesothelin monoclonal antibody conjugated to the maytansine derivative tubulin inhibitor DM4 through a reducible disulphide linker (
Figure 23A)
[21][84]. BAY-94 9343 has antiproliferative activity because after binding to mesothelin on tumour cells it is internalised and the disulphide linker is cleaved, releasing DM4. Subsequently, DM4 binding to tubulin disrupts microtubule polymerisation, causing cell cycle arrest and apoptosis and consequently killing the dividing cells
[22][23][85,86] (
Figure 23A). Preclinical studies have shown that anetumab ravtansine is highly cytotoxic in MSLN-expressing mesotheliomas, as well as in pancreatic, non-small-cell lung, and ovarian cancer cell lines
[20][83].
In an in vivo study, anetumab ravtansine was shown to have antitumour activity in mesotheliomas as well as in pancreatic and ovarian xenograft models
[21][84]. A study by Quanz et al. demonstrated that in ovarian cancer cell lines and patient-derived xenografts, the combination of anetumab ravtansine with pegylated liposomal doxorubicin (PLD) or with carboplatin, copanlisib, or bevacizumab showed an additive antiproliferative activity both in vitro and in vivo compared to either agent used as a monotherapy
[24][87].
2.4. Chimeric Antigen Receptor T cell (CAR T) Therapy
MSLN has also been regarded as an attractive target for chimeric antigen receptor T cell (CAR T) therapy because of its abundant expression in tumour cells and its limited expression in normal cells. CAR T therapy is a type of treatment in which a patient’s T cells, obtained by apheresis, are modified in the laboratory via the insertion of a gene for a special receptor called the chimeric antigen receptor (CAR). CAR T cells can target cell surface antigens without major histocompatibility complex (MHC) restriction. Thus, CAR T cells can be used for broad HLA-diverse allogeneic recipients.
The CAR is usually complex, with an extracellular antigen recognition domain that corresponds to a single-chain variable fragment (scFv) of a specific antibody, a transmembrane domain anchored to the cell membrane of the T cell, and an intracellular domain that transmits T cell activation signals. To amplify the activation signals in CARs, MSLN can be used in two co-stimulator domains, which allows for major activation in terms of proliferation, cytotoxicity, and consequently antitumour efficacy. The considerable effectiveness of this subtype of CAR, known as “
third-generation MSLN”, has been proven in many neoplasms and in ovarian carcinoma
[25][88] (
Figure 3B). CAR T cells are grown in the laboratory and then administered to the patient by infusion. The CAR T cells are able to bind to antigens on the cancer cells and kill them. Once attached to the antigens present on the neoplastic cells, the CAR T cells become activated and stimulate the host’s immune system, which in turn attacks the MSLN-expressing cells
[26][89]. The effectiveness of CAR T therapy has been observed in mouse models of different solid neoplasms, including ovarian carcinomas and mesotheliomas, in which the chimeric receptors recognised human MSLN and the inflammatory cytokines secreted by the T cells (including IL-2, IL-6, tumour necrosis factor alpha, and interferon-y) produced cytotoxic effects in the cancer cells (
Figure 23B) (
Table 12)
[27][28][90,91]. Banville et al. provided insights into the design of logic-gated CAR T cell strategies with a greater number of antigens. The authors demonstrated that the most promising pairwise combination was CA125 and MSLN. Thus, a CAR T cell strategy against CA125 and MSLN would target most tumour cells in the majority of cases
[29][92]. However, as observed in treatments for other neoplasms, it must be kept in mind that the immunosuppressive tumour microenvironment of neoplasms plays an important role in the response to CAR T therapy in vivo. Many authors have demonstrated that a transmembrane protein named programmed death ligand 1 (PD-L1) plays an important role in regulating the T cell response. The binding of this substance to the inhibitor programmed cell death protein 1 (PD-1) or the binding of PD-1 to the immune co-inhibitory receptor lymphocyte activation gene-3 (LAG3) transmits an inhibitory signal, causing a reduction in the proliferation of antigen-specific T cells, and consequently a reduction in the infiltration of T cells into the tumour lesion
[30][31][32][93,94,95]. For ovarian carcinoma, recent in vivo preclinical studies have shown that it is possible to restore the functions of the tumour-specific checkpoint blockade in MSLN-directed CAR T cells using different substances
[31][32][33][94,95,96].
The side effects of treatment observed during CAR T therapy are related to excessive immune activation, which causes cytokine release syndrome (CRS) and neurotoxicity. These adverse effects are probably due to non-specific T cell activation. CRS is an acute systemic inflammatory disorder characterised by fever, and sometimes by the fatal dysfunction of many organs
[34][35][97,98]. Severe CRS symptoms can culminate in delirium, seizures, and encephalopathy caused by high levels of IL-6, IFN gamma, and CAR T cells in the cerebrospinal fluid
[36][99]. Compartmental CRS (C-CRS) was reported in a patient with advanced ovarian cancer treated with mesothelin-targeted CAR T cells, characterised by the elevation of IL-6 and accumulation in the pleural fluid
[35][98]. The treatment used against this serious side effect sometimes involves using an anti-IL-6R antibody, tocilizumab
[37][100]. In cases with the involvement of the nervous system and unresponsive cases to tocilizumab, corticosteroids have often been used
[36][37][38][39][99,100,101,102], or suicide genes have been introduced within T cells to reduce their number and activity (
ClinicalTrials.gov identifiers: NTC0374965).
2.5. Vaccines
Cancer vaccines are immunotherapy treatments that induce a tumour-specific immune response in the host that is capable of recognising and eliminating neoplastic cells. The ability of T cells to recognise the antigens present on neoplastic cells and to produce an immune response capable of destroying them has long been known. In this type of immunotherapy for MSLN-positive cancers, Listeria monocytogenes, a Gram-positive bacterium, can be used as a vector. In humans, this bacterium causes infections with gastroenteritis, meningitis, and encephalitis; however, the human immune system is generally capable of controlling the disease
[40][41][103,104]. The CRS-207 vaccine uses attenuated Listeria monocytogenes (Lm) (Lm ΔactA/ΔinlB) bacteria that are engineered to express human MSLN and can be used to treat MSLN-positive neoplasms (
Figure 23B) (
Table 12)
[42][105].
The methods used to attenuate the virulence of Lm are mostly based on the deletion of certain genes that allow for sufficient infectivity and antigen production; however, it still has the potential to result in severe infection. Therefore, this treatment should be used with caution for patients with immunodeficiencies
[43][106].
Treatment using CRS-207 with human-MSLN-expressing Listeria allows for the stimulation of the immune system with a robust response against neoplastic cells via different mechanisms. After fusion with a lysosome in the cytoplasm of an antigen-presenting cell, Lm can be killed; the secretions of its antigens into the cytosol as well as those prior to degradation in the phagosome can be loaded onto major histocompatibility complex (MHC) I and MCH II, causing the activation of potent CD 4 helper lymphocytes and CD 8 cytotoxic lymphocytes. In addition, during its entry into the antigen-presenting cell, Lm can activate proinflammatory genes through Toll-like receptors, which can amplify the response against neoplastic cells through the use of inflammatory cytokines
[44][107] (
Figure 23B) (
Table 12).