Developing novel drug formulations and progressing them to the clinical environment relies on preclinical in vitro studies and animal tests to evaluate efficacy and toxicity. However, these current techniques have failed to accurately predict the clinical success of new therapies with a high degree of certainty. The main reason for this failure is that conventional in vitro tissue models lack numerous physiological characteristics of human organs, such as biomechanical forces and biofluid flow. Moreover, animal models often fail to recapitulate the physiology, anatomy, and mechanisms of disease development in human. These shortfalls often lead to failure in drug development, with substantial time and money spent. To tackle this issue, organ-on-chip technology offers realistic in vitro human organ models that mimic the physiology of tissues, including biomechanical forces, stress, strain, cellular heterogeneity, and the interaction between multiple tissues and their simultaneous responses to a therapy. For the latter, complex networks of multiple-organ models are constructed together, known as multiple-organs-on-chip. Numerous studies have demonstrated successful application of organ-on-chips for drug testing, with results comparable to clinical outcomes.
The full version of the paper can be viewed in Bioengineering 2022, 9(4), 150; https://doi.org/10.3390/bioengineering9040150
1. Introduction
Intensive and costly preclinical tests on novel therapeutic agents often involve animal studies prior to human trials. In addition to being ethically controversial, animal models have been increasingly criticized for their limited ability to predict the efficacy, safety, and toxicity of numerous drugs in humans [1,2]. Animal testing is predisposed—by its xenogeneic nature and failure to represent the complicated anatomical and physiological systems in humans—to lead to discordant results and, consequently, to failures in translating the results to clinical trials. Conventional in vitro models that utilize two-dimensional (2D) or three-dimensional (3D) cell cultures, on the other hand, are limited in their predictive capabilities of in vivo conditions due to the absence of critical physiological factors, such as fluid flow and biomechanical forces [3]. Consequently, the development of novel methodologies that could accurately represent the physiological conditions of the human body in an in vitro platform to perform drug testing is of critical importance to accelerate the development of novel therapeutics that can be used in clinical settings. Intensive and costly preclinical tests on novel therapeutic agents often involve animal studies prior to human trials. In addition to being ethically controversial, animal models have been increasingly criticized for their limited ability to predict the efficacy, safety, and toxicity of numerous drugs in humans [1][2]. Animal testing is predisposed—by its xenogeneic nature and failure to represent the complicated anatomical and physiological systems in humans—to lead to discordant results and, consequently, to failures in translating the results to clinical trials. Conventional in vitro models that utilize two-dimensional (2D) or three-dimensional (3D) cell cultures, on the other hand, are limited in their predictive capabilities of in vivo conditions due to the absence of critical physiological factors, such as fluid flow and biomechanical forces [3]. Consequently, the development of novel methodologies that could accurately represent the physiological conditions of the human body in an in vitro platform to perform drug testing is of critical importance to accelerate the development of novel therapeutics that can be used in clinical settings.
The development of micro-structured functional human organ models, known as organ-on-chip technology, is a potential solution for providing a physiologically relevant in vitro platform and has attracted increasing interest [3]. Organ-on-chips aim to provide a translational model for human organs to predict human responses to therapeutic agents. As a result, they can deliver reliable and accurate outcome measures and also likely have the potential to predict clinical trial results. Since its advent, organ-on-chip technology has been widely studied and found to offer numerous advantages in recapitulating organ physiology to study human diseases and its potential for drug testing. Current reviews on the application of organ-on-chips for in vitro drug tests mainly focus on models of certain organs, their microfluidic designs and structures, and their relevance to healthy or diseased tissues whilst providing examples of their potential application for testing drugs [4,5,6,7,8]. In addition, these reviews elaborate on the advances in organ-on-chips and their future opportunities for commercialization of these platforms for drug testing [3,9,10,11]. The development of micro-structured functional human organ models, known as organ-on-chip technology, is a potential solution for providing a physiologically relevant in vitro platform and has attracted increasing interest [3]. Organ-on-chips aim to provide a translational model for human organs to predict human responses to therapeutic agents. As a result, they can deliver reliable and accurate outcome measures and also likely have the potential to predict clinical trial results. Since its advent, organ-on-chip technology has been widely studied and found to offer numerous advantages in recapitulating organ physiology to study human diseases and its potential for drug testing. Current reviews on the application of organ-on-chips for in vitro drug tests mainly focus on models of certain organs, their microfluidic designs and structures, and their relevance to healthy or diseased tissues whilst providing examples of their potential application for testing drugs [4][5][6][7][8]. In addition, these reviews elaborate on the advances in organ-on-chips and their future opportunities for commercialization of these platforms for drug testing [3][9][10][11]. Table 1 provides an overview of the different relevant reviews and their comparison with the current review on the application of organ-on-chips for drug testing. This review will provide a pharmaceutical perspective by focusing on the application of organ-on-chips for different preclinical drug tests with improved relevance. Hence, the studies on organ-on-chips will be discussed based on the assays used to evaluate drug efficacy and toxicity in vitro, which are important for drug development and commercialization. Further, the advantages of organ-on-chips in drug testing will be elaborated based on their physiologically relevant dynamic design [12,13,14], emulation of the inter-organ crosstalk in the human body [15,16], enabling patient-specific drug testing [17], and high throughput time-efficient assays by integrated miniaturised analytical tools [18,19]. Liver, kidney, and respiratory system models will be the focus of this review due to their broad applicability in toxicology [20], drug metabolism [21], and drug delivery/transport [22] studies. provides an overview of the different relevant reviews and their comparison with the current entry on the application of organ-on-chips for drug testing. This entry will provide a pharmaceutical perspective by focusing on the application of organ-on-chips for different preclinical drug tests with improved relevance. Hence, the studies on organ-on-chips will be discussed based on the assays used to evaluate drug efficacy and toxicity in vitro, which are important for drug development and commercialization. Further, the advantages of organ-on-chips in drug testing will be elaborated based on their physiologically relevant dynamic design [12][13][14], emulation of the inter-organ crosstalk in the human body [15][16], enabling patient-specific drug testing [17], and high throughput time-efficient assays by integrated miniaturised analytical tools [18][19]. Liver, kidney, and respiratory system models will be the focus of this entry due to their broad applicability in toxicology [20], drug metabolism [21], and drug delivery/transport [22] studies.
Table 1. Overview of the primary focus of relevant reviews in the application of OOCs for preclinical drug testing compared with the current review.
Overview of the primary focus of relevant reviews in the application of OOCs for preclinical drug testing compared with the current entry.
2. Drug Testing Capabilities Using Liver-, Kidney-, and Lung-on-Chip Models
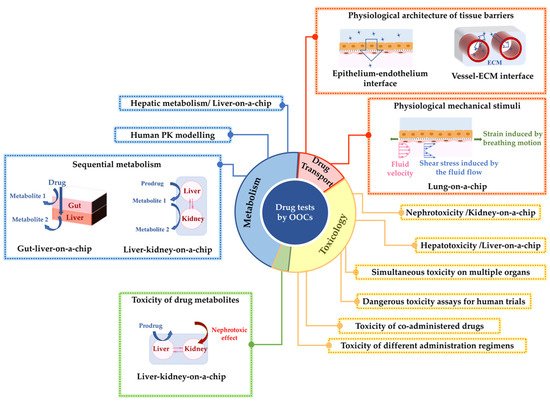
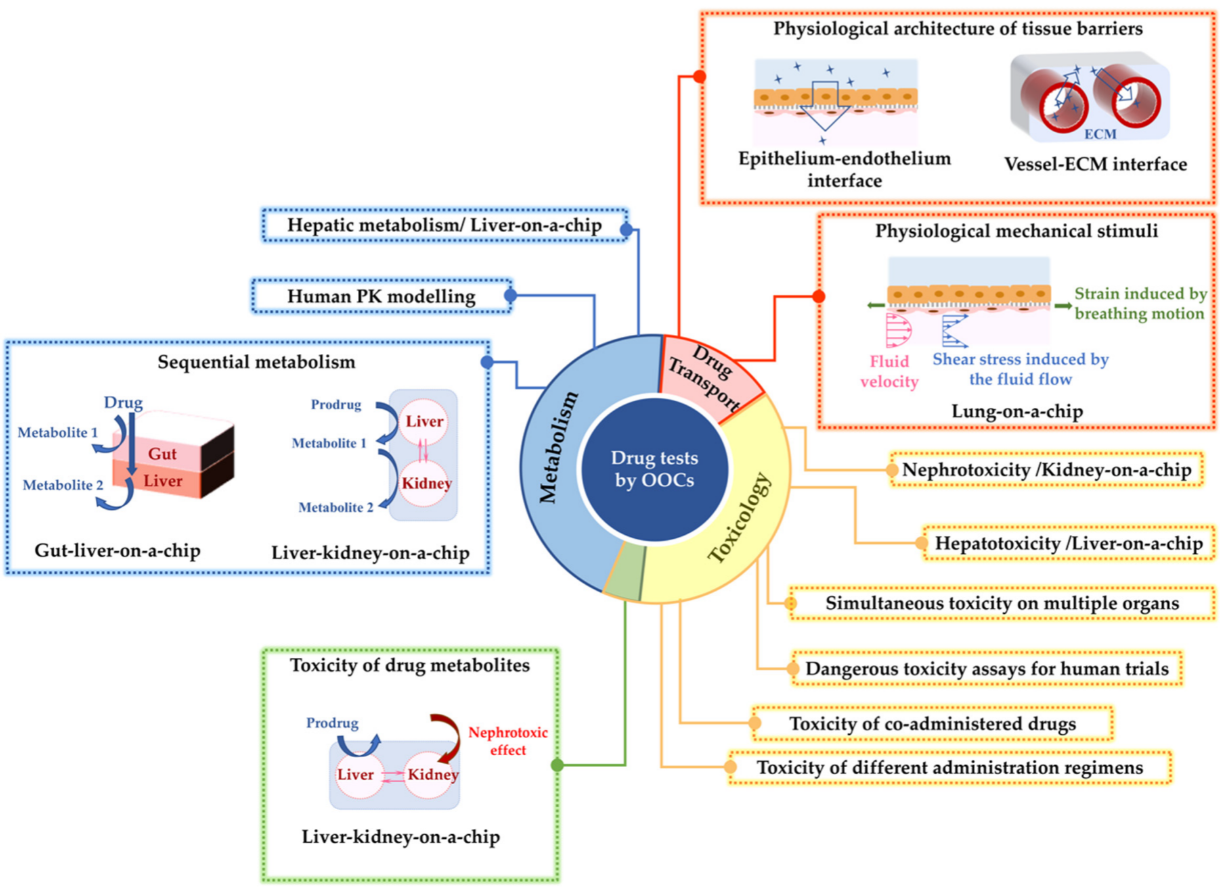
Liver-, kidney-, and lung-on-chip models have recreated some key functions of their respective organs for drug metabolism, expression of cytotoxic response to drugs, and barrier function against drug permeation.
2. Drug Testing Capabilities Using Liver-, Kidney-, and Lung-on-Chip Models
Liver-, kidney-, and lung-on-chip models have recreated some key functions of their respective organs for drug metabolism, expression of cytotoxic response to drugs, and barrier function against drug permeation.
Figure 1 summarizes how these organ-on-chips have been used for studies on drug metabolism, toxicology, and transport.
summarizes how these organ-on-chips have been used for studies on drug metabolism, toxicology, and transport.
Figure 1. A summary of the investigations on three important drug assessments: drug metabolism, toxicology, and drug transport using liver-, kidney-, and lung-on-chip models. The figure summarizes the advantages of these organ-on-chip models to enhance drug testing.
2.1. Drug Metabolism Studies
The principal, although not the sole, site for metabolism of nearly all ingested drugs is the liver [23]. Consequently, first-pass hepatic metabolism has a paramount influence on the efficacy and side effects of drugs, which highlights the importance of simulating this biological process during drug testing. Organ-on-chip technology has been utilized for screening drug metabolism, where recapitulation conditions of the liver tissue have been the main focus [24,25]. A summary of the investigations on three important drug assessments: drug metabolism, toxicology, and drug transport using liver-, kidney-, and lung-on-chip models. The figure summarizes the advantages of these organ-on-chip models to enhance drug testing.
2.1. Drug Metabolism Studies
The principal, although not the sole, site for metabolism of nearly all ingested drugs is the liver [23]. Consequently, first-pass hepatic metabolism has a paramount influence on the efficacy and side effects of drugs, which highlights the importance of simulating this biological process during drug testing. Organ-on-chip technology has been utilized for screening drug metabolism, where recapitulation conditions of the liver tissue have been the main focus [24][25]. Table 2 summarizes the studies on the metabolism of different drugs using liver-on-chip models and the interconnection of the liver with other organs-on-chip.
The utilization of organ-on-chip technology to construct the network of multiple organs is beneficial to mimic the complex interaction between organs in metabolizing drugs, prodrugs, and micronutrients in vivo. For instance, a liver–kidney-on-chip with interconnected chambers for liver and kidney cell culture was developed by Tehobald et al. [26] to imitate sequential hepatic and renal metabolism of vitamin D. The device could mimic hepatic metabolism of vitamin D to 25-hydroxyvitamin D and its further metabolism to 1,25-dihydroxyvitamin D by the kidney analog. The latter bioactive metabolite is known for its anti-tumor effect and for inducing differentiation in multiple tumor cell types, such as acute myeloid leukemia cells.
Studying the drug metabolism process in multi-organs-on-chip models and their comparison with single-organ-on-chip models can shed insights into understanding the tissue–tissue crosstalk and individual contribution to the metabolic process [27]. In another study, Choe et al. reproduced the first-pass-metabolism process in a microfluidic gut–liver chip with two chambers separated by a membrane to culture gut epithelial and liver cells [28]. The gut cells’ culture chamber was located on top of the liver cells’ chamber, so that the drug molecules passing across the gut epithelial barrier could reach the liver cells. This enables emulation of the simultaneous drug absorption in the gut and metabolic reaction in the liver that the drug goes through after oral intake. The metabolic activity of the gut–liver chip was compared to the gut monoculture system, and the gut epithelial cells were highlighted to have significantly higher contribution in the metabolism of apigenin.
Another important factor that needs to be considered when designing in vitro drug-metabolism models is that the rates of absorption and metabolism are influenced by the volumes and dimensions of the designed organ model [29]. Hence, it is important to replicate the relative sizes of organ analogs and the circulating fluid flow connecting them based on the physiology of the human body in order to achieve accurate pharmacokinetic (PK) modelling using multi-organs-on-chip. Some studies on the application of multi-organs-on-chips to replicate human drug metabolism have focused on the design of devices based on mathematically modelled PK profiles [30,31]. These microfluidic chips are promising tools to emulate human-relevant PK in vitro. For instance, the first-pass metabolism of orally taken paracetamol was replicated in a gut–liver-on-chip [31]. The design parameters of the chip were such that the surface area of the gut and the volume of the liver compartment was optimized based on a mathematical PK model close to the human PK.
Taken together, organ-on-chips have been able to successfully model the metabolism of numerous drugs, either by a single tissue or multiple tissues interconnected. As shown in
summarizes the studies on the metabolism of different drugs using liver-on-chip models and the interconnection of the liver with other organs-on-chip.
The utilization of organ-on-chip technology to construct the network of multiple organs is beneficial to mimic the complex interaction between organs in metabolizing drugs, prodrugs, and micronutrients in vivo. For instance, a liver–kidney-on-chip with interconnected chambers for liver and kidney cell culture was developed by Tehobald et al. [26] to imitate sequential hepatic and renal metabolism of vitamin D. The device could mimic hepatic metabolism of vitamin D to 25-hydroxyvitamin D and its further metabolism to 1,25-dihydroxyvitamin D by the kidney analog. The latter bioactive metabolite is known for its anti-tumor effect and for inducing differentiation in multiple tumor cell types, such as acute myeloid leukemia cells.
Studying the drug metabolism process in multi-organs-on-chip models and their comparison with single-organ-on-chip models can shed insights into understanding the tissue–tissue crosstalk and individual contribution to the metabolic process [27]. In another study, Choe et al. reproduced the first-pass-metabolism process in a microfluidic gut–liver chip with two chambers separated by a membrane to culture gut epithelial and liver cells [28]. The gut cells’ culture chamber was located on top of the liver cells’ chamber, so that the drug molecules passing across the gut epithelial barrier could reach the liver cells. This enables emulation of the simultaneous drug absorption in the gut and metabolic reaction in the liver that the drug goes through after oral intake. The metabolic activity of the gut–liver chip was compared to the gut monoculture system, and the gut epithelial cells were highlighted to have significantly higher contribution in the metabolism of apigenin.
Another important factor that needs to be considered when designing in vitro drug-metabolism models is that the rates of absorption and metabolism are influenced by the volumes and dimensions of the designed organ model [29]. Hence, it is important to replicate the relative sizes of organ analogs and the circulating fluid flow connecting them based on the physiology of the human body in order to achieve accurate pharmacokinetic (PK) modelling using multi-organs-on-chip. Some studies on the application of multi-organs-on-chips to replicate human drug metabolism have focused on the design of devices based on mathematically modelled PK profiles [30][31]. These microfluidic chips are promising tools to emulate human-relevant PK in vitro. For instance, the first-pass metabolism of orally taken paracetamol was replicated in a gut–liver-on-chip [31]. The design parameters of the chip were such that the surface area of the gut and the volume of the liver compartment was optimized based on a mathematical PK model close to the human PK.
Taken together, organ-on-chips have been able to successfully model the metabolism of numerous drugs, either by a single tissue or multiple tissues interconnected. As shown in
, the majority of these devices are evaluated based on the testing of only one drug molecule. Future research is needed to test a wide variety of drug candidates and formulations, with their excipients using these devices to validate them against existing in vivo observations and to study any drug–drug interactions that may occur as a result of concomitant drug uptake.
Summary of the drug metabolism and drug toxicity studies that include liver and/or kidney tissue models on organ-on-chips.
| Drug |
Toxicology |
Metabolism |
Tissue(s) |
Reference |
diclofenac
acetaminophen |
✓ |
|
liver |
[18] |
| troglitazone |
✓ |
|
liver |
[19] |
| acetaminophen |
✓ |
|
liver |
[32,33,34,35, | [33][34 | 36] | [32]][35][36] |
| acetaminophen |
✓ |
✓ |
liver |
[37,38] | [37][38] |
acetaminophen
isoniazid
rifampicin |
✓ |
✓ |
liver |
[39] |
rifampin
ketoconzazole
acetaminophen |
✓ |
✓ |
liver |
[40] |
bupropion
tolbutamide
omeprazole
testosterone |
|
✓ |
liver |
[24] |
| 7-ethoxy-4-trifluoromethyl coumarin |
|
✓ |
liver |
[25] |
acetaminophen
chlorpromazine
tacrine |
✓ |
|
liver |
[41] |
ccetaminophen
fialuridine |
✓ |
✓ |
liver |
[42] |
| diclofenac |
✓ |
✓ |
liver |
[43] |
cadmium
aspirin
caffein
troglitazone
rosiglitazone
pioglitazone
acetaminophen |
✓ |
|
liver |
[2] |
| cisplatin |
✓ |
|
kidney |
[14] |
| adriamycin |
✓ |
|
kidney |
[44] |
| gentamicin |
✓ |
|
kidney |
[45] |
| polymyxin B |
✓ |
|
kidney |
[46] |
| carboxylated polystyrene nanoparticles |
✓ |
|
GI tract–liver |
[47] |
| troglitazone |
✓ |
✓ |
liver–intestine
liver–skin |
[48] |
| apigenin |
|
✓ |
gut–liver |
[28] |
epirubicine
irinotecan
cyclophosphamide |
|
✓ |
small intestine–liver–lung |
[29] |
ifosfamide
verapamil |
✓ |
✓ |
liver–kidney |
[49] |
| paracetamol |
|
✓ |
liver–gut |
[31] |
mannitol
propranolol
caffeine |
|
✓ |
GI–liver |
[50] |
| combination of genistein and dacarbazine |
|
✓ |
intestine–liver |
[51] |
| 5-fluorouracil |
✓ |
|
liver–tumor–marrow |
[52] |
| paracetamol |
✓ |
✓ |
liver–kidney |
[53] |
diclofenac
ketoconazole
hydrocortisone
acetaminophen |
✓ |
|
liver–heart–skin |
[54] |
| luteolin |
|
✓ |
liver–tumor |
[30] |
capecitabine
tegafur |
|
✓ |
liver–cancer intestine–liver–cancer–connective tissue |
[27] |
| digoxin |
✓ |
|
intestine–kidney |
[55] |
| ifosfamide |
✓ |
✓ |
liver–kidney |
[56] |
| vitamin D |
|
✓ |
liver–kidney |
[26] |
2.2. Toxicology
Drug-induced toxicity is one of the major reasons for the failure of drug candidates and the withdrawal of approved drugs from the market [57]. The main reason for drug toxicity is the undesirable off-target activity of drug molecules or their reactive metabolites. Determining toxicity early in the drug discovery pipeline remains a challenge, as animal studies do not efficiently predict toxicity responses in human [3,58]. Therefore, accurate high-throughput assays for toxicity prediction are highly valuable in the pharmaceutical industry to reject potentially toxic drug candidates at the early stages. In this regard, the application of new technologies that could enable toxicity studies to be done in the context of organotypic biology as highly predictive models has attracted significant interest [57,59].
2.2. Toxicology
Drug-induced toxicity is one of the major reasons for the failure of drug candidates and the withdrawal of approved drugs from the market [57]. The main reason for drug toxicity is the undesirable off-target activity of drug molecules or their reactive metabolites. Determining toxicity early in the drug discovery pipeline remains a challenge, as animal studies do not efficiently predict toxicity responses in human [3][58]. Therefore, accurate high-throughput assays for toxicity prediction are highly valuable in the pharmaceutical industry to reject potentially toxic drug candidates at the early stages. In this regard, the application of new technologies that could enable toxicity studies to be done in the context of organotypic biology as highly predictive models has attracted significant interest [57][59]. Table 2 summarizes the studies utilizing kidney and liver tissues-on-chip for drug toxicity assays (since nephrotoxicity [14,44,45,46,49,55,56] and hepatotoxicity [32,33,38,40,41,42,43,51,60] are the most common adverse effects reported in drug development).
2.2.1. Toxicology Studies by the Kidney- or Liver-on-Chip Models
The liver- and kidney-on-chip models were developed to have in vivo-like tissue functionalities, and they have demonstrated superiority over the conventional cell culture platforms in predicting toxic drug responses [14]. For instance, a kidney-glomerulus-on-chip was developed using pluripotent stem cells differentiated into kidney podocytes [44]. The cells in this device expressed morphological, molecular, and functional characteristics similar to mature human podocytes. Indeed, the renal toxicity associated with albuminuria induced by a cancer drug, Adriamycin, was successfully simulated by this device. Furthermore, the hepatotoxic effect of acetaminophen was also modelled by liver-on-chip models, where the toxic response of the tissue model to the drug treatment was evaluated based on the disruption in basic liver function or secretion of biomarkers similar to in vivo observations [34,35].
The application of organ-on-chips in toxicology has also been expanded to simulate specific drug administration schedules. Previous studies have shown that organ-on-chips can differentiate dosage regimens, where the modality of drug administration or the interaction of drugs may influence the toxicity response of organ tissues. A kidney-on-chip model simulated the nephrotoxicity of gentamicin in two different administration regimens: bolus injection and continuous infusion [45]. These different treatment regimens, given in the same dose, led to significantly different nephrotoxicity outcomes, with increased cytotoxicity detected for continuous infusion. Organ-on-chips also enabled the simulation of toxicity response to drug–drug interactions in patients undergoing treatment of multiple diseases with coadministration of medicines. A study by Ma et al. reported an in vitro, 3D, liver-lobule-like microtissue [39] that was used to simulate adverse drug reactions caused by the interaction of acetaminophen and omeprazole, rifampicin, ciprofloxacin, or probenecid. The consequent hepatotoxic effects reported in vivo could be simulated in vitro by this chip. It was observed that the pretreatment of the chip with omeprazole or probenecid resulted in an increased hepatotoxic effect of acetaminophen. However, the toxicity effect was alleviated by pretreatment of the cells with rifampicin or ciprofloxacin.
Another benefit of performing toxicology studies in organ-on-chips is that they can be used to assess poisonous molecules that are not ethically acceptable to subject healthy humans to. One example of this application are studies on radiation-induced injuries and testing the efficacy of radioprotective drugs or assessing radiotherapies [61]. Since the experimental exposure of healthy people to radiation is unethical, the organ-on-chips can offer valuable input in this area to conduct these assessments safely and rapidly. Another study that supports this application is the coculture of mammary epithelial cells and hepatic carcinoma cells on a chip [62]. The chip was exposed to gamma radiation to mimic the space-like environment, where the radioprotection effect of amifostine prodrug on human mammary epithelial cells after metabolism by the liver could be modelled in vitro.
2.2.2. Toxicology Studies by the Kidney- and Liver-on-Chip Models Interconnected with Other Organs
Simulating a network of organs based on physiological PK has been promising in toxicology studies [63]. An example of this network is a lung–liver-on-chip that simulated the decreased toxicity of inhaled toxicants in the lung tissue because of the detoxification process in the liver tissue [64]. Such multi-organs-on-chip platforms also enable the simulation of drug metabolism in one organ and the consequent toxic effect of the formed metabolites in another organ [47,53,55]. Similarly, severe nephrotoxicity of ifosfamide anticancer prodrug observed in the clinic could be emulated by a liver–kidney-on-chip that mimicked the interaction of kidney and liver [56]. Multi-organs-on-chips also allow simultaneous evaluation of the cytotoxic effects on the targeted and untargeted organs, where a study by Theobald et al. was able to model both the hepatotoxicity and nephrotoxicity of Aflatoxin B1 in a kidney–liver-on-chip [65].
The multi-organ-on-chips—in their advanced form involving more organ analogs—could eventually mimic the drug toxicity in the whole human body, significantly helping the prediction of side effects of drug candidates at a very early stage in vitro.
2.3. Drug Delivery/Transport
Transport of therapeutics across tissue barriers is one of the major challenges in drug delivery that can influence the bioavailability of drugs [66] and, hence, requires considerations and optimizations during drug discovery. Skin, epithelium, intestine, and blood-brain barrier (BBB) are examples of tissue in the human body that provide effective barriers against the delivery of therapeutics via transdermal, respiratory, oral, and intravenous drug delivery routes, respectively. Drug transport across in vitro tissue barrier models is another assessment where the application of the organ-on-chip models can be beneficial.
2.3.1. Simulation of In Vivo-Level Barrier Functions On-Chip
Organ-on-chips can model tissue-specific barrier functions with reliable physiological relevance to study drug permeation. The organ-on-chip models used for drug permeation studies are mainly designed as dual-chamber structures with a donor and an acceptor chamber. The donor chamber is mainly located on top of the acceptor chamber, and the tissue barrier is represented by the culture of cells on a permeable membrane that separates the two chambers. The quantity of drug transported from the donor to the acceptor chamber is measured to evaluate the efficient permeation of the developed drugs across the tissue barriers [12,50,54]. A study by Chen et al. modelled gastrointestinal (GI) barrier functionality in a GI–liver system [50]. This coculture cell model was able to express the desired physiological relevance, as assessed by the transepithelial electrical resistance (TEER) similar to the human native gut, and allowed emulation of the in vivo absorption of drugs across the gut wall. TEER measures the electrical resistance of the developed epithelium model and is a quantitative representation of the tissue barrier function and formation of tight junctions (TJs) between the cells [67]. Additionally, the GI barrier functionality was demonstrated in terms of the permeability of mannitol, propranolol, and caffeine across the primary intestinal monolayer in this chip. Organ-on-chips can also recreate heterogenous cellular structures, where the transport of substances occurs across adjacent tissues. The goal is to simulate the neighbouring tissues-on-chip with the coculture of different cell types to create structures similar to the native organs in the human body. This was proven feasible by a lung-on-chip developed by Huh et al. that could mimic the interaction between the pulmonary alveoli and the neighboring vascular endothelium in the human lung [12]. Therefore, this model enables the consideration of regulatory functions of both the epithelial and endothelial tissues as a more reliable barrier model for pulmonary drug-delivery tests.
2.3.2. Simulation of Multiple Drug-Delivery Routes On-Chip
Multi-organs-on-chip structured by the coculture of different organs also enabled the evaluation of different drug delivery routes and resultant transport of drug to the target tissue. This was demonstrated in a study by de Melo et al., where the skin barrier and dermal drug absorption were modelled by a Strat-M
summarizes the studies utilizing kidney and liver tissues-on-chip for drug toxicity assays (since nephrotoxicity [14][44][45][46][49][55][56] and hepatotoxicity [32][33][38][40][41][42][43][51][60] are the most common adverse effects reported in drug development).
2.2.1. Toxicology Studies by the Kidney- or Liver-on-Chip Models
The liver- and kidney-on-chip models were developed to have in vivo-like tissue functionalities, and they have demonstrated superiority over the conventional cell culture platforms in predicting toxic drug responses [14]. For instance, a kidney-glomerulus-on-chip was developed using pluripotent stem cells differentiated into kidney podocytes [44]. The cells in this device expressed morphological, molecular, and functional characteristics similar to mature human podocytes. Indeed, the renal toxicity associated with albuminuria induced by a cancer drug, Adriamycin, was successfully simulated by this device. Furthermore, the hepatotoxic effect of acetaminophen was also modelled by liver-on-chip models, where the toxic response of the tissue model to the drug treatment was evaluated based on the disruption in basic liver function or secretion of biomarkers similar to in vivo observations [34][35].
The application of organ-on-chips in toxicology has also been expanded to simulate specific drug administration schedules. Previous studies have shown that organ-on-chips can differentiate dosage regimens, where the modality of drug administration or the interaction of drugs may influence the toxicity response of organ tissues. A kidney-on-chip model simulated the nephrotoxicity of gentamicin in two different administration regimens: bolus injection and continuous infusion [45]. These different treatment regimens, given in the same dose, led to significantly different nephrotoxicity outcomes, with increased cytotoxicity detected for continuous infusion. Organ-on-chips also enabled the simulation of toxicity response to drug–drug interactions in patients undergoing treatment of multiple diseases with coadministration of medicines. A study by Ma et al. reported an in vitro, 3D, liver-lobule-like microtissue [39] that was used to simulate adverse drug reactions caused by the interaction of acetaminophen and omeprazole, rifampicin, ciprofloxacin, or probenecid. The consequent hepatotoxic effects reported in vivo could be simulated in vitro by this chip. It was observed that the pretreatment of the chip with omeprazole or probenecid resulted in an increased hepatotoxic effect of acetaminophen. However, the toxicity effect was alleviated by pretreatment of the cells with rifampicin or ciprofloxacin.
Another benefit of performing toxicology studies in organ-on-chips is that they can be used to assess poisonous molecules that are not ethically acceptable to subject healthy humans to. One example of this application are studies on radiation-induced injuries and testing the efficacy of radioprotective drugs or assessing radiotherapies [61]. Since the experimental exposure of healthy people to radiation is unethical, the organ-on-chips can offer valuable input in this area to conduct these assessments safely and rapidly. Another study that supports this application is the coculture of mammary epithelial cells and hepatic carcinoma cells on a chip [62]. The chip was exposed to gamma radiation to mimic the space-like environment, where the radioprotection effect of amifostine prodrug on human mammary epithelial cells after metabolism by the liver could be modelled in vitro.
2.2.2. Toxicology Studies by the Kidney- and Liver-on-Chip Models Interconnected with Other Organs
Simulating a network of organs based on physiological PK has been promising in toxicology studies [63]. An example of this network is a lung–liver-on-chip that simulated the decreased toxicity of inhaled toxicants in the lung tissue because of the detoxification process in the liver tissue [64]. Such multi-organs-on-chip platforms also enable the simulation of drug metabolism in one organ and the consequent toxic effect of the formed metabolites in another organ [47][53][55]. Similarly, severe nephrotoxicity of ifosfamide anticancer prodrug observed in the clinic could be emulated by a liver–kidney-on-chip that mimicked the interaction of kidney and liver [56]. Multi-organs-on-chips also allow simultaneous evaluation of the cytotoxic effects on the targeted and untargeted organs, where a study by Theobald et al. was able to model both the hepatotoxicity and nephrotoxicity of Aflatoxin B1 in a kidney–liver-on-chip [65].
The multi-organ-on-chips—in their advanced form involving more organ analogs—could eventually mimic the drug toxicity in the whole human body, significantly helping the prediction of side effects of drug candidates at a very early stage in vitro.
2.3. Drug Delivery/Transport
Transport of therapeutics across tissue barriers is one of the major challenges in drug delivery that can influence the bioavailability of drugs [66] and, hence, requires considerations and optimizations during drug discovery. Skin, epithelium, intestine, and blood-brain barrier (BBB) are examples of tissue in the human body that provide effective barriers against the delivery of therapeutics via transdermal, respiratory, oral, and intravenous drug delivery routes, respectively. Drug transport across in vitro tissue barrier models is another assessment where the application of the organ-on-chip models can be beneficial.
2.3.1. Simulation of In Vivo-Level Barrier Functions On-Chip
Organ-on-chips can model tissue-specific barrier functions with reliable physiological relevance to study drug permeation. The organ-on-chip models used for drug permeation studies are mainly designed as dual-chamber structures with a donor and an acceptor chamber. The donor chamber is mainly located on top of the acceptor chamber, and the tissue barrier is represented by the culture of cells on a permeable membrane that separates the two chambers. The quantity of drug transported from the donor to the acceptor chamber is measured to evaluate the efficient permeation of the developed drugs across the tissue barriers [12][50][54]. A study by Chen et al. modelled gastrointestinal (GI) barrier functionality in a GI–liver system [50]. This coculture cell model was able to express the desired physiological relevance, as assessed by the transepithelial electrical resistance (TEER) similar to the human native gut, and allowed emulation of the in vivo absorption of drugs across the gut wall. TEER measures the electrical resistance of the developed epithelium model and is a quantitative representation of the tissue barrier function and formation of tight junctions (TJs) between the cells [67]. Additionally, the GI barrier functionality was demonstrated in terms of the permeability of mannitol, propranolol, and caffeine across the primary intestinal monolayer in this chip. Organ-on-chips can also recreate heterogenous cellular structures, where the transport of substances occurs across adjacent tissues. The goal is to simulate the neighbouring tissues-on-chip with the coculture of different cell types to create structures similar to the native organs in the human body. This was proven feasible by a lung-on-chip developed by Huh et al. that could mimic the interaction between the pulmonary alveoli and the neighboring vascular endothelium in the human lung [12]. Therefore, this model enables the consideration of regulatory functions of both the epithelial and endothelial tissues as a more reliable barrier model for pulmonary drug-delivery tests.
2.3.2. Simulation of Multiple Drug-Delivery Routes On-Chip
Multi-organs-on-chip structured by the coculture of different organs also enabled the evaluation of different drug delivery routes and resultant transport of drug to the target tissue. This was demonstrated in a study by de Melo et al., where the skin barrier and dermal drug absorption were modelled by a Strat-M
® membrane incorporated in a heart–liver-body-on-chip system [54]. The chip system mimicked both transdermal and systemic drug delivery routes and, hence, could predict both hepatotoxicity and cardiotoxicity of four model drugs administered to the chip: diclofenac, ketoconazole, hydrocortisone, and acetaminophen. In another study, Ozkan et al. conducted drug permeation studies using a two-vessel structure-on-chip mimicking the vascularized microenvironments of the liver and breast tumors [68]. The two vessels were surrounded by collagen-based extracellular matrix (ECM) with breast cancer cells or liver cells cultured in each vessel. This chip allowed evaluation of particle diffusion from a vessel into its surrounding ECM and back into the vessel, as well as transportation between the two vessels. For this purpose, particles of different sizes were perfused through these vascularized microenvironments to replicate chemotherapy drugs and drugs conjugated with nanoparticles. The resultant permeability of the tumor microenvironment and the accumulation of particles observed in ECM from this chip were consistent with in vivo findings [68,69,70,71,72].
2.3.3. Drug Delivery Tests under In Vivo-Inspired Dynamic Conditions On-Chip
Another added benefit of organ-on-chips is the capability to perform drug transport studies under mechanically dynamic conditions. The physiological mechanical cues in native organs could be emulated in the engineered design of organ-on-chips. This can enable drug-transport studies across tissue barriers under more physiologically realistic conditions. This feature was prominent and was highlighted in the lung-on-chip model that had capabilities to emulate both the strain exerted on the alveolar–capillary barriers by breathing motions and the shear stress on the capillary endothelium induced by the blood flow [12]. The lung-on-chip could mimic the physiological breathing motion via cyclic vacuuming of two channels on the sides. This resulted in cyclic stretching motions of a membrane inside the cell-culture channel, inducing physiological levels of cyclic strain. This dynamic microenvironment was eventually found to influence the permeability of the alveolar–endothelium interface. Higher permeability of nanoparticles across the alveolar–capillary interface was observed when the physiological strain was emulated compared to the device at static condition. The control, static, Transwell culture was prepared with the coculture of the alveolar epithelial cells and capillary endothelial cells on the opposing sides of the membrane. In another study, a human nasal epithelial mucosa-on-chip with a dual-channel structure was developed to model the nasal epithelial barrier against nasal drug delivery [73]. The transport of ibuprofen across the modelled epithelium was evaluated under physiologically relevant flowing fluid conditions in the donor channel. It was observed that the circulating pulsatile fluid flow in the bottom channel resulted in an increase in the drug transport rate compared to the static condition in the chip. This observation was explained by the increase in the convective mass transfer coefficient in the fluid due to the flow condition, which highlights the necessity of conducting nasal drug transport studies under dynamic conditions.
2.3.4. Further Improvements of Drug Delivery Studies by Organ-on-Chips
There remain unexplored areas to improve the relevance of drug-delivery studies by organ-on-chips. For instance, the simulation of realistic drug administration forms, namely the topical delivery of aerosolized solutions or dry powders within the dynamic microenvironments of organ-on-chips, has not been studied. Such simulations enable mimicking of the realistic deposition of fluidized particles to the target tissue and the aerosol characteristics that can influence the efficacy of aerosol drug delivery. These characteristics include particle size and flowrate of aerosolized particles, which can affect the delivered dose [74,75]. Additionally, physiological barriers that adversely affect the efficiency of drug-delivery routes have not been comprehensively studied by organ-on-chips. As a case-in-point, the mucociliary clearance mechanism that limits the residential time of drug particles in human airways is an unexplored area by in vitro models of lower [12,13,76] and upper [73] airways-on-chip. Simulation of this airway defense mechanism by future lung and nasal epithelium-on-chip models can profoundly enhance their physiological relevance and, eventually, their ability to model relevant clinical drug test results in vitro.
membrane incorporated in a heart–liver-body-on-chip system [54]. The chip system mimicked both transdermal and systemic drug delivery routes and, hence, could predict both hepatotoxicity and cardiotoxicity of four model drugs administered to the chip: diclofenac, ketoconazole, hydrocortisone, and acetaminophen. In another study, Ozkan et al. conducted drug permeation studies using a two-vessel structure-on-chip mimicking the vascularized microenvironments of the liver and breast tumors [68]. The two vessels were surrounded by collagen-based extracellular matrix (ECM) with breast cancer cells or liver cells cultured in each vessel. This chip allowed evaluation of particle diffusion from a vessel into its surrounding ECM and back into the vessel, as well as transportation between the two vessels. For this purpose, particles of different sizes were perfused through these vascularized microenvironments to replicate chemotherapy drugs and drugs conjugated with nanoparticles. The resultant permeability of the tumor microenvironment and the accumulation of particles observed in ECM from this chip were consistent with in vivo findings [68][69][70][71][72].
2.3.3. Drug Delivery Tests under In Vivo-Inspired Dynamic Conditions On-Chip
Another added benefit of organ-on-chips is the capability to perform drug transport studies under mechanically dynamic conditions. The physiological mechanical cues in native organs could be emulated in the engineered design of organ-on-chips. This can enable drug-transport studies across tissue barriers under more physiologically realistic conditions. This feature was prominent and was highlighted in the lung-on-chip model that had capabilities to emulate both the strain exerted on the alveolar–capillary barriers by breathing motions and the shear stress on the capillary endothelium induced by the blood flow [12]. The lung-on-chip could mimic the physiological breathing motion via cyclic vacuuming of two channels on the sides. This resulted in cyclic stretching motions of a membrane inside the cell-culture channel, inducing physiological levels of cyclic strain. This dynamic microenvironment was eventually found to influence the permeability of the alveolar–endothelium interface. Higher permeability of nanoparticles across the alveolar–capillary interface was observed when the physiological strain was emulated compared to the device at static condition. The control, static, Transwell culture was prepared with the coculture of the alveolar epithelial cells and capillary endothelial cells on the opposing sides of the membrane. In another study, a human nasal epithelial mucosa-on-chip with a dual-channel structure was developed to model the nasal epithelial barrier against nasal drug delivery [73]. The transport of ibuprofen across the modelled epithelium was evaluated under physiologically relevant flowing fluid conditions in the donor channel. It was observed that the circulating pulsatile fluid flow in the bottom channel resulted in an increase in the drug transport rate compared to the static condition in the chip. This observation was explained by the increase in the convective mass transfer coefficient in the fluid due to the flow condition, which highlights the necessity of conducting nasal drug transport studies under dynamic conditions.
2.3.4. Further Improvements of Drug Delivery Studies by Organ-on-Chips
There remain unexplored areas to improve the relevance of drug-delivery studies by organ-on-chips. For instance, the simulation of realistic drug administration forms, namely the topical delivery of aerosolized solutions or dry powders within the dynamic microenvironments of organ-on-chips, has not been studied. Such simulations enable mimicking of the realistic deposition of fluidized particles to the target tissue and the aerosol characteristics that can influence the efficacy of aerosol drug delivery. These characteristics include particle size and flowrate of aerosolized particles, which can affect the delivered dose [74][75]. Additionally, physiological barriers that adversely affect the efficiency of drug-delivery routes have not been comprehensively studied by organ-on-chips. As a case-in-point, the mucociliary clearance mechanism that limits the residential time of drug particles in human airways is an unexplored area by in vitro models of lower [12][13][76] and upper [73] airways-on-chip. Simulation of this airway defense mechanism by future lung and nasal epithelium-on-chip models can profoundly enhance their physiological relevance and, eventually, their ability to model relevant clinical drug test results in vitro.