Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Camila Xu and Version 1 by Marina Carrasco-Llatas.
Drug-induced sleep endoscopy (DISE) is a diagnostic tool to assess the upper airway of snorers and obstructive sleep apnea patients in conditions that mimic natural sleep.
- drug-induced sleep endoscopy
- DISE
- sedation
- obstructive sleep apnea
1. Introduction
Obstructive sleep apnea (OSA) is a common health problem that is associated with an increase in cardiovascular morbimortality, a decrease in quality of life, and a higher risk of traffic accidents due to hypersomnolence [1,2]. Standard treatment for OSA is positive upper airway pressure, usually delivered in a continuous mode, known as continuous positive airway pressure (CPAP) therapy. CPAP acts like a pneumatic splint that opens the upper airway (UA), regardless of the site of obstruction. Nevertheless, CPAP adherence can be poor, and therefore alternative therapies are necessary [3]. On the other hand, surgery has 100% compliance but has limited effect on unselected patients [4]. With the arrival of new technologies such as transoral robotic surgery (TORS) and coblation, new modalities for the treatment of tongue base obstruction is now available. The sleep surgeon needs to know the exact area or areas of upper airway collapse in order to select patients that may improve with surgery and determine the areas that need to be surgically addressed.
Routine UA assessment is performed when patients are awake—a state with no UA collapse or oxygen desaturation. In a small percentage of OSA patients, the anatomical causes of the obstruction are obvious (e.g., grade 4 palatine and/or lingual tonsils). However, for most patients, the cause is not so obvious, as they may have long soft palate, a relatively large tongue with grade 1 tonsils, or previous tonsillectomy. Therefore, it is of utmost importance to understand the UA behavior during sleep so that tailor-made treatment can be decided for every patient.
In the late 1970s, evaluation of the UA during natural sleep was proposed [5]. Unfortunately, observation of the UA during natural sleep is complicated and impractical in daily practice. On the other hand, with the aid of sedation, the UA can be observed dynamically to allow the sleep surgeon to have an accurate idea of what is happening during sleep and the possible treatment options. Other diagnostic tools such as MRI or CT scan under sedation are also possible. Although MRI and CT scans have the advantage of having complete visualization of the UA simultaneously, they are limited by the facilities available and the need to collaborate with the radiology department. Maneuvers or changes in the position during sleep MRI or CT scan are also almost impossible. For this reason, drug-induced sleep endoscopy (DISE) has spread all over the world and is the preferred diagnostic technique to assess the UA of patients who snore or have OSA in a state that simulates natural sleep [6].
1. Introduction
Obstructive sleep apnea (OSA) is a common health problem that is associated with an increase in cardiovascular morbimortality, a decrease in quality of life, and a higher risk of traffic accidents due to hypersomnolence [1][2]. Standard treatment for OSA is positive upper airway pressure, usually delivered in a continuous mode, known as continuous positive airway pressure (CPAP) therapy. CPAP acts like a pneumatic splint that opens the upper airway (UA), regardless of the site of obstruction. Nevertheless, CPAP adherence can be poor, and therefore alternative therapies are necessary [3]. On the other hand, surgery has 100% compliance but has limited effect on unselected patients [4]. With the arrival of new technologies such as transoral robotic surgery (TORS) and coblation, new modalities for the treatment of tongue base obstruction is now available. The sleep surgeon needs to know the exact area or areas of upper airway collapse in order to select patients that may improve with surgery and determine the areas that need to be surgically addressed.
Routine UA assessment is performed when patients are awake—a state with no UA collapse or oxygen desaturation. In a small percentage of OSA patients, the anatomical causes of the obstruction are obvious (e.g., grade 4 palatine and/or lingual tonsils). However, for most patients, the cause is not so obvious, as they may have long soft palate, a relatively large tongue with grade 1 tonsils, or previous tonsillectomy. Therefore, it is of utmost importance to understand the UA behavior during sleep so that tailor-made treatment can be decided for every patient.
In the late 1970s, evaluation of the UA during natural sleep was proposed [5]. Unfortunately, observation of the UA during natural sleep is complicated and impractical in daily practice. On the other hand, with the aid of sedation, the UA can be observed dynamically to allow the sleep surgeon to have an accurate idea of what is happening during sleep and the possible treatment options. Other diagnostic tools such as MRI or CT scan under sedation are also possible. Although MRI and CT scans have the advantage of having complete visualization of the UA simultaneously, they are limited by the facilities available and the need to collaborate with the radiology department. Maneuvers or changes in the position during sleep MRI or CT scan are also almost impossible. For this reason, drug-induced sleep endoscopy (DISE) has spread all over the world and is the preferred diagnostic technique to assess the UA of patients who snore or have OSA in a state that simulates natural sleep [6].
2. Technique
Since the first publication on DISE [7], several drugs or drug combinations have been used for sedation. Some authors also use nasal decongestion, local anesthesia, and/or anti-secretory drugs. So far, there is also no uniformity regarding how to perform the sedation. Nevertheless, this point is critical to achieve a sedation level that resembles natural sleep in order to obtain reliable DISE findings.
In the European position paper on DISE, and its later update, Ear, Nose and throat (ENT) experts on DISE put in their collective opinion and recommended possible set-up and techniques for DISE to be reliably practiced in different centers [6][8].
2.1. Where to Perform DISE and Materials
DISE must be performed in a room where all the basic resuscitation equipment (e.g., oxygen supply) are available, because safety is of utmost importance. The room should also be quiet and dark.
In order to perform DISE, the patient should be monitored with electrocardiogram (ECG) and pulse oximeter. Monitoring of sedation depth such as Bi-spectral index (BIS) is highly recommended, as the BIS level of sedation should be between 70 and 50 when the UA is evaluated in adults [6]. Evaluation of the UA in lighter sedation may underestimate the obstruction, whereas deeper sedation may cause artificial obstruction due to over sedation [9][10][11]. Having said that, one must be aware that sedation levels observed with these devices are an estimate of actual sedation, as some people are not well sedated at those recommended levels, although the majority of adult people are. For children, these BIS levels might not be applicable.
The thinnest possible fiber endoscope, ideally with working channel to aspirate secretions, is recommended. The researchers also recommend a recording system for video and sound, if possible. The recording is useful, as the videos can be replayed to the patients to help them understand their problem better as well as the potential difficulty in addressing the obstruction. The videos may also be useful in the future if the results of the UA surgery do not achieve the desired outcomes.
2.2. Drugs for Sedation and Method
Based on the literature, many drugs (midazolam, propofol, dexmedetomidine, remifentanil, ketamine) are used, either alone or in combination, in order to achieve the ideal level of sedation [6]. All of them have their own advantages and disadvantages. Discussing this specific subject is beyond the scope of this entry; more details are explained elsewhere [12][13]. In this manuscript, only sedation with propofol using target-controlled infusion (TCI) pump will be described, as it is the sedation method that is evidence-proven to demonstrate UA collapses resembling natural sleep. Studies comparing natural sleep and TCI-propofol sleep have shown that the critical closing pressure, UA muscle responsiveness, apnea hypopnea index (AHI), levels of sedation measured by BIS and sites of obstruction are equivalent to those observed during N2 and N3 stages of natural sleep [14][15][16][17][18][19]. It is important to note that REM sleep cannot be reproduced with propofol sedation [15]. DISE usually takes 15–30 min. Within this short duration, only N2 sleep can be achieved [20]. Nevertheless, it is during this stage that most of the events occur (unless the patient has events only in REM sleep). Therefore, DISE should be considered a snapshot of what happens during the night, but it cannot provide information for the entire night. This is a limitation of the procedure, but as-long-as there is no tool that can show the behavior of every structure of the UA during natural sleep for the whole night, DISE will continue to be the best tool available.
It is recommended to titrate the TCI-propofol pump slowly to achieve the ideal level of sedation (BIS: 70–50, does not respond to verbal stimuli). According to Heiser et al. and the personal experience, this level of sedation is achieved when the brain concentration is approximately 3 µg/mL [9]. In order to reach this concentration as quickly as possible without causing central apneas, the pump can be programmed to 2 or 2.5 µg/mL, with an increase of 0.5 µg/mL every two minutes until the level of sedation is achieved. An addition of 1–2 mg of midazolam at the beginning of the sedation will shorten the time to the observation window, although it may also cause an increase in sneezing, making the assessment more difficult [21].
DISE is not a painful technique, therefore local anesthesia of the nose is not necessary. Neither is nasal decongestion [6]. Antisecretory drugs such as atropine are not recommended for routine use as atropine’s effect on the UA is unknown [6]. Nevertheless, the visualization of the UA dynamics can be extremely difficult in the presence of secretions, and therefore the physician performing DISE has to balance the pros and cons and act accordingly.
2.3. Maneuvers and Position
The patients are usually observed in supine decubitus position, because this is the position where most of the events occur. However, assessment of the UA in a lateral position does give additional information, especially for those patients that sleep mostly in a lateral decubitus position. If the patient’s history suggests that he or she should be assessed in a lateral decubitus position, it may be easier to start DISE in this position, including doing the necessary maneuvers, before changing to supine position. Although the initial study by the de Vries group noted that the UA findings were similar in lateral decubitus compared with supine decubitus with the head turned to one side [22], a recent study with a larger sample size proved that their initial findings were inaccurate, emphasizing the need to observe the UA in lateral decubitus [23].
2. Technique
Since the first publication on DISE [7], several drugs or drug combinations have been used for sedation. Some authors also use nasal decongestion, local anesthesia, and/or anti-secretory drugs. So far, there is also no uniformity regarding how to perform the sedation. Nevertheless, this point is critical to achieve a sedation level that resembles natural sleep in order to obtain reliable DISE findings.
In the European position paper on DISE, and its later update, Ear, Nose and throat (ENT) experts on DISE put in their collective opinion and recommended possible set-up and techniques for DISE to be reliably practiced in different centers [6,8].
2.1. Where to Perform DISE and Materials
DISE must be performed in a room where all the basic resuscitation equipment (e.g., oxygen supply) are available, because safety is of utmost importance. The room should also be quiet and dark.
In order to perform DISE, the patient should be monitored with electrocardiogram (ECG) and pulse oximeter. Monitoring of sedation depth such as Bi-spectral index (BIS) is highly recommended, as the BIS level of sedation should be between 70 and 50 when the UA is evaluated in adults [6]. Evaluation of the UA in lighter sedation may underestimate the obstruction, whereas deeper sedation may cause artificial obstruction due to over sedation [9,10,11]. Having said that, one must be aware that sedation levels observed with these devices are an estimate of actual sedation, as some people are not well sedated at those recommended levels, although the majority of adult people are. For children, these BIS levels might not be applicable.
The thinnest possible fiber endoscope, ideally with working channel to aspirate secretions, is recommended. The authors also recommend a recording system for video and sound, if possible. The recording is useful, as the videos can be replayed to the patients to help them understand their problem better as well as the potential difficulty in addressing the obstruction. The videos may also be useful in the future if the results of the UA surgery do not achieve the desired outcomes.
2.2. Drugs for Sedation and Method
Based on the literature, many drugs (midazolam, propofol, dexmedetomidine, remifentanil, ketamine) are used, either alone or in combination, in order to achieve the ideal level of sedation [6]. All of them have their own advantages and disadvantages. Discussing this specific subject is beyond the scope of this article; more details are explained elsewhere [12,13]. In this manuscript, only sedation with propofol using target-controlled infusion (TCI) pump will be described, as it is the sedation method that is evidence-proven to demonstrate UA collapses resembling natural sleep. Studies comparing natural sleep and TCI-propofol sleep have shown that the critical closing pressure, UA muscle responsiveness, apnea hypopnea index (AHI), levels of sedation measured by BIS and sites of obstruction are equivalent to those observed during N2 and N3 stages of natural sleep [14,15,16,17,18,19]. It is important to note that REM sleep cannot be reproduced with propofol sedation [15]. DISE usually takes 15–30 min. Within this short duration, only N2 sleep can be achieved [20]. Nevertheless, it is during this stage that most of the events occur (unless the patient has events only in REM sleep). Therefore, DISE should be considered a snapshot of what happens during the night, but it cannot provide information for the entire night. This is a limitation of the procedure, but as-long-as there is no tool that can show us the behavior of every structure of the UA during natural sleep for the whole night, DISE will continue to be the best tool available.
It is recommended to titrate the TCI-propofol pump slowly to achieve the ideal level of sedation (BIS: 70–50, does not respond to verbal stimuli). According to Heiser et al. and our personal experience, this level of sedation is achieved when the brain concentration is approximately 3 µg/mL [9]. In order to reach this concentration as quickly as possible without causing central apneas, the pump can be programmed to 2 or 2.5 µg/mL, with an increase of 0.5 µg/mL every two minutes until the level of sedation is achieved. An addition of 1–2 mg of midazolam at the beginning of the sedation will shorten the time to the observation window, although it may also cause an increase in sneezing, making the assessment more difficult [21].
DISE is not a painful technique, therefore local anesthesia of the nose is not necessary. Neither is nasal decongestion [6]. Antisecretory drugs such as atropine are not recommended for routine use as atropine’s effect on the UA is unknown [6]. Nevertheless, the visualization of the UA dynamics can be extremely difficult in the presence of secretions, and therefore the physician performing DISE has to balance the pros and cons and act accordingly.
2.3. Maneuvers and Position
The patients are usually observed in supine decubitus position, because this is the position where most of the events occur. However, assessment of the UA in a lateral position does give additional information, especially for those patients that sleep mostly in a lateral decubitus position. If the patient’s history suggests that he or she should be assessed in a lateral decubitus position, it may be easier to start DISE in this position, including doing the necessary maneuvers, before changing to supine position. Although the initial study by the de Vries group noted that the UA findings were similar in lateral decubitus compared with supine decubitus with the head turned to one side [22], a recent study with a larger sample size proved that their initial findings were inaccurate, emphasizing the need to observe the UA in lateral decubitus [23].
It is very common for patients to open their mouths during DISE, as they usually do at home. If the mouth is open, the tongue may move backward, pushing the soft palate and further obstructing the UA. Changes to the areas and pattern of obstruction can be observed by just closing the mouth. This maneuver (often called chin-lift) is different from the Esmarch maneuver, which gently pulls the mandible forward to simulate the effect of a mandibular advancement device (MAD). As showed by the Antwerp group, maximum advancement of the mandible does not represent what a MAD can achieve [24]. Other than the advancement of the mandible, the thickness of a MAD needs to be simulated as well. Therefore, an interincisive distance of approximately 5 mm is necessary to mimic a MAD. The authors pull the mandible by grabbing it with the fingers inside the mouth in order to mimic the thickness and the protrusion of the MAD in place. This maneuver is also believed to be less painful compared with pushing the mandible at its angle (
It is very common for patients to open their mouths during DISE, as they usually do at home. If the mouth is open, the tongue may move backward, pushing the soft palate and further obstructing the UA. Changes to the areas and pattern of obstruction can be observed by just closing the mouth. This maneuver (often called chin-lift) is different from the Esmarch maneuver, which gently pulls the mandible forward to simulate the effect of a mandibular advancement device (MAD). As showed by the Antwerp group, maximum advancement of the mandible does not represent what a MAD can achieve [24]. Other than the advancement of the mandible, the thickness of a MAD needs to be simulated as well. Therefore, an interincisive distance of approximately 5 mm is necessary to mimic a MAD. The researchers pull the mandible by grabbing it with the fingers inside the mouth in order to mimic the thickness and the protrusion of the MAD in place. This maneuver is also believed to be less painful compared with pushing the mandible at its angle (
Figure 1). Performing DISE with a custom-made MAD is also feasible. DISE can begin with the MAD in place. The device can be removed after observing the UA for potential collapse for at least two cycles (stable snoring, apneas/hypopneas and breathing), and the UA can be observed for another two or more cycles with different positions and maneuvers. This is because insertion of a MAD while the patient is sedated is extremely difficult, while removal is much easier with less arousal for the patient [24,25].
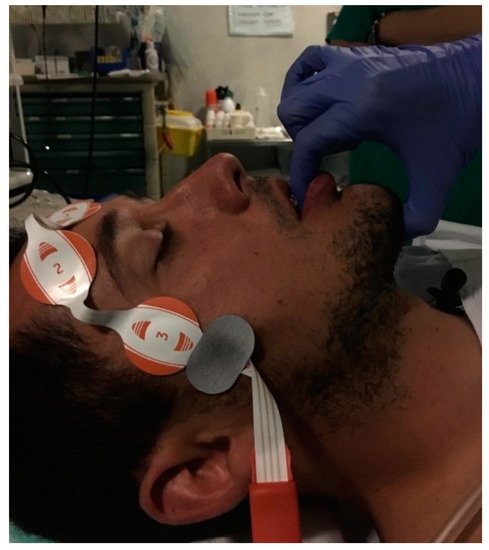
). Performing DISE with a custom-made MAD is also feasible. DISE can begin with the MAD in place. The device can be removed after observing the UA for potential collapse for at least two cycles (stable snoring, apneas/hypopneas and breathing), and the UA can be observed for another two or more cycles with different positions and maneuvers. This is because insertion of a MAD while the patient is sedated is extremely difficult, while removal is much easier with less arousal for the patient [24][25].
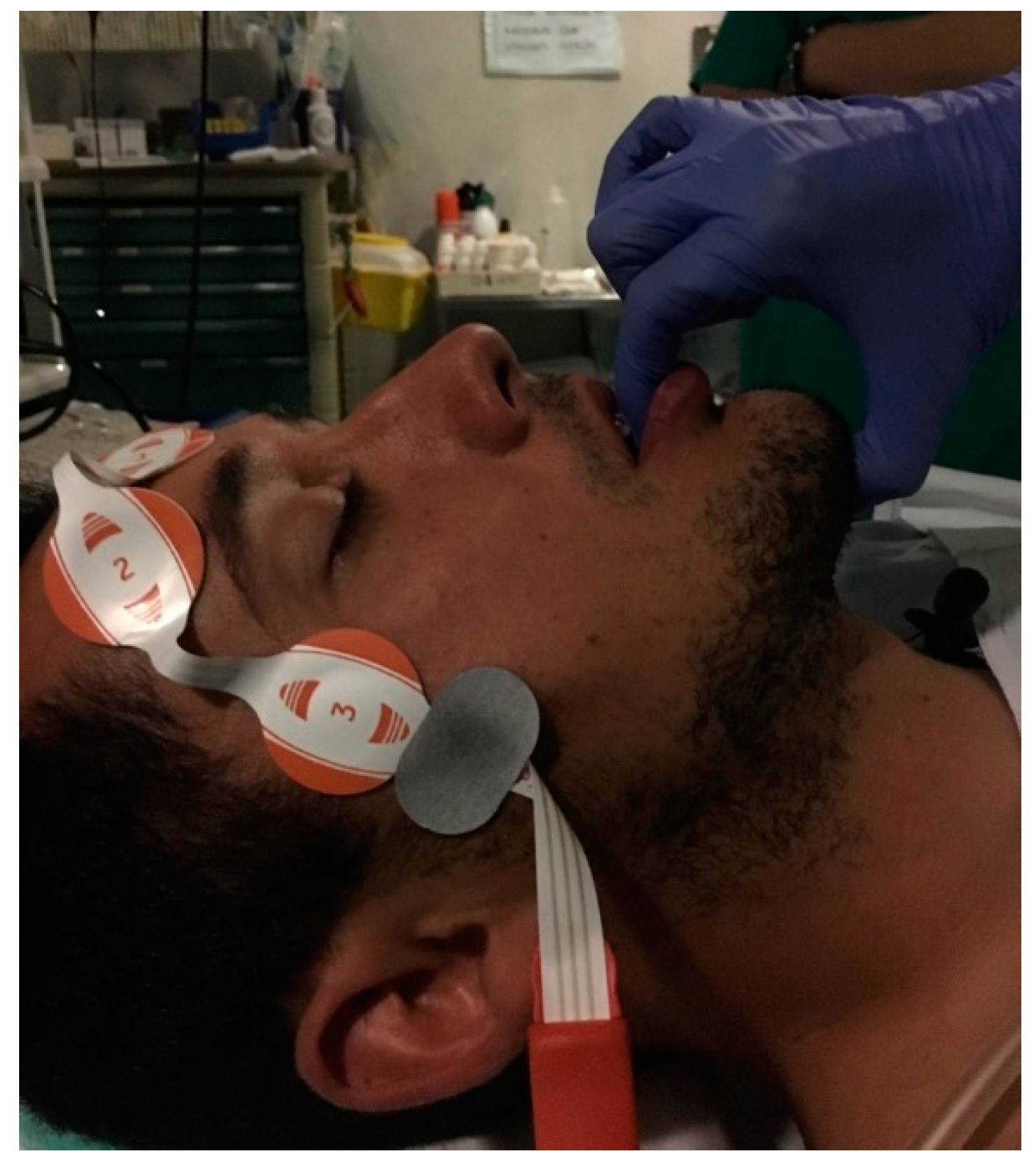
Figure 1. Modified Esmarch maneuverer grabbing the mandible of the patient to mimic the action of a mandibular advancement device (MAD).
Modified Esmarch maneuverer grabbing the mandible of the patient to mimic the action of a mandibular advancement device (MAD).
