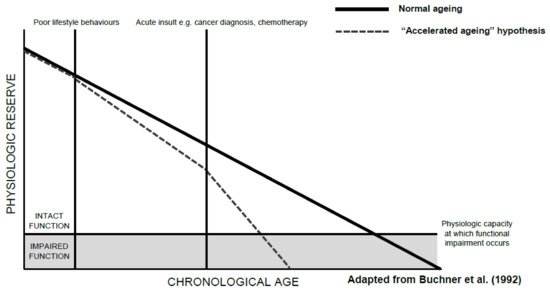
A decline in functional status, an individual’s ability to perform the normal activities required to maintain adequate health and meet basic needs, is part of normal ageing. Functional decline, however, appears to be accelerated in older patients with cancer. Such decline can occur as a result of a cancer itself, cancer treatment-related factors, or a combination of the two. The accelerated decline in function seen in older patients with cancer can be slowed, or even partly mitigated through routine assessments of functional status and timely interventions where appropriate. This is particularly important given the link between functional decline and impaired quality of life, increased mortality, comorbidity burden, and carer dependency.
- cancer
- elderly
- functional decline
- functional status
- frailty
- ageing
1. Introduction
2. Assessment of Functional Decline
Instrument | Method of Administration | Domains Assessed | Comments | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
Functional status | |||||||||||
3.2. Cancer-Related Functional Decline
3.3. Cancer Treatment-Related Functional Decline
3.3.1. Systemic Therapy
3.3.2. Radiotherapy
3.3.3. Surgery
4. Mechanisms Driving Functional Decline
Patient Characteristics and Social Factors | Clinical Factors | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Barthel Index [25] (Basic ADLs) | Patient-reported or direct observation | |||||||||||||
Cancer-related factors | Treatment-related factors | Feeding, toileting, bathing, dressing, and undressing, toilet transfers, incontinence, bed transfers, and ambulation | Intended for patients with stroke, neuromuscular disorders, musculoskeletal disorders, and cancer. | |||||||||||
Eastern Cooperative Oncology Group Performance Status (ECOG) [26] | ||||||||||||||
Patient-reported | Percentage of day spent ambulatory or in bed | 5-point scale, where 0 is “Fully active” and independent and 5 is “Dead”. Commonly used in oncology due to its simplicity [27]. Tends to have minimal direct input from the patient. Noted by the International Society of Geriatric Oncology (SIOG) to be a poor marker of function as functional impairment can occur in the presence of good performance status [28]. | ||||||||||||
Karnofsky Performance Status Scale (KPS) | (Both instrumental and basic ADLs) | Patient-reported | Activity, work, self-care | 10–100-point scale, gold-standard measurement of performance status in cancer. Thorne-modified KPS better suited to community-based and palliative care settings [29], while Australia-modified KPS is better suited to settings with multiple venues of care across both inpatient and outpatient settings [30]. Noted by SIOG to be a poor marker of function as functional impairment can occur in the presence of good performance status [28]. | ||||||||||
Katz Index of Independence in Activities of Daily Living Scale (ADL) [31] | (Basic ADLs) | Patient-reported | Bathing, dressing, toileting, transferring, continence, and feeding | Most commonly used instrument in studies assessing activities of daily living in adults with cancer [32]. Shortened versions are often used due to length: modified Katz-1 assesses dressing, bathing, transferring, eating, and toileting, but does not assess continence; modified Katz-2 assesses the original six domains in the Katz ADL scale, as well as walking across a small room [27]. | ||||||||||
Lawton Instrumental Activities of Daily Living Scale (IADL) [33] | Patient-reported | Ability to use telephone, shopping, food preparation, housekeeping, laundry, transport, responsibility for medications, and finances | Second-most commonly used instrument used in studies assessing activities of daily living in adults with cancer [32]. | |||||||||||
Rosow–Breslau Health Scale [33] | Patient-reported | Ability to do heavy housework, walk up and down stairs, and walk half a mile | Simple 3-point scale that can be easily implemented in the clinical setting. Less commonly used in patients with cancer and in oncology research. | |||||||||||
Functional Independence Measure (FIM) [34] | Direct observation | Self-care, sphincter control, transfers, locomotion, communication, and social cognition | Used for evaluation in the rehabilitation of patients post-stroke, traumatic brain injury, spinal cord injury, or cancer. | |||||||||||
Frail Elderly Functional Assessment Questionnaire (FEFA) [35] | Patient-reported | Mobility, transfers, housework, meal preparation, finances, telephone use, eating, dressing, personal hygiene, and medication management | Older, less-widely used tool. Validated against Katz ADL, IADL, and Barthel Index [36]. | |||||||||||
Elderly Functional Index (ELFI) [37] | Patient-reported | Physical functioning, role functioning, social functioning, and mobility | Newer tool derived from functional domains of common quality of life instrument European Organisation for Research and Treatment (EORTC) Quality of Life Questionnaire Core-30 (QLQ-C30). Suggested for use as an endpoint of functional status in clinical trials or in clinical practice. | |||||||||||
Physical performance measures | ||||||||||||||
Grip strength | Direct observation | Forearm strength | Requires a dynamometer for testing. Poorer scores are associated with poorer health-related quality of life [38] and increased mortality [39] in patients with cancer. | |||||||||||
Gait speed [40] | Direct observation | Walking speed over a short distance, typically 4, 6, 8, or 10 m | Poorer scores are associated with decreased survival outcomes and treatment-related complications in cancer survivors [41]. Requires a stopwatch, although electronic gait mats or automatic timing devices provide more accurate assessments [40]. | |||||||||||
6-Minute Walk Test (6MWT) [17] | Direct observation | Aerobic capacity and endurance over six minutes of walking | Good measure of cardiorespiratory fitness. Validated for use in patients with cancer [42]. Does not require specialised equipment, but does require a stopwatch and a walkway of known length. | |||||||||||
Timed Up and Go Test (TUG) [43] | Direct observation | Gait speed and mobility: measures the time taken to rise from a chair, walk three meters, turn around, walk back to the chair, and sit down while turning 180 degrees | Poorer scores are associated with decreased survival outcomes, treatment-related complications, and functional decline in cancer survivors [41]. Can be used as a substitute measure for gait speed. Does not require specialised equipment. | |||||||||||
Short Physical Performance Battery (SPPB) [44] | Direct observation | Lower limb muscle strength, balance, and mobility | Poorer scores are associated with decreased survival outcomes, treatment-related complications, and functional decline in cancer survivors [41]. Can be used as a substitute measure for gait speed. Does not require specialised equipment. | |||||||||||
Physical Performance Test (PPT) [45] | Direct observation | Writing, eating, dressing, grip strength, mobility, dexterity, communication, upper limb function, and balance | Requires various household items for assessment. Direct comparison with the KPS scale indicates that the PPT is more accurate in measuring functional status in older patients with cancer [46]. | |||||||||||