Injectable hydrogels (IHs) are smart biomaterials and are the most widely investigated and versatile technologies, which can be either implanted or inserted into living bodies with minimal invasion. Their unique features, tunable structure and stimuli-responsive biodegradation properties make these IHs promising in many biomedical applications, including tissue engineering, regenerative medicines, implants, drug/protein/gene delivery, cancer treatment, aesthetic corrections and spinal fusions. Regarding their current prospective and ongoing research, hydrogel formulations have some limitations in their applications, clinical practices and sustainability. Many hydrogel systems (natural/synthetic), such as thermosensitive hydrogels, are free-flowing sols at a low temperature, while upon raising to body temperature (physiological temperature), they are converted to a stable visco-elastic gel phase, such as poly (phosphazene), pluronic and poly (N-isopropyl acrylamide).
1. Introduction
Biomaterial with desirable therapeutic efficacy, drug-delivery capabilities and enhanced properties has paved the way for the effective targeted treatment of diseases and injured tissue repair. It has become a promising area of human health-related research in biomedical material, agricultural, environmental, chemical, engineering and other applied sciences
[1]. Over the last decade, hydrogels and their desirable biomedical applications, such as biocompatibility, non-toxicity, biodegradability, flexibility, biofunctionality, sol–gel transitions, tunable properties, physico-chemical properties, degree of swelling and porosity, synthesis, crosslinking, drug-encapsulation, sustained/control release of therapeutic agents (drug, proteins, genes, cells, etc.), tissue regeneration/repairing, wound healing, cancer chemotherapy and the treatment of superbug bacterial infections, have been extensively observed and investigated
[1][2][3][4][1,2,3,4]. Hydrogels are a hydrophilic polymer system that has the capability of retaining a significant amount of water and swelling in an aqueous medium. However, due to their three-dimensional (3D) crosslinking structure, they remain insoluble in water and biological fluids
[1][4][1,4]. The high water content and their polymeric meshwork and side chain maintain their well-defined structures due to their highly adsorptive surfaces, as well as spatiotemporal control over their physico-chemical properties and the release of encapsulated drug from hydrogel cores
[5].
The typical administration of a hydrogel formulation begins from its early use in contact lenses to its extensively developed complicated applications, mostly in tissue engineering and gene/DNA delivery for sustained and controlled drug delivery. Wound healing dressing, sensors, mucoadhesive, bioactive factor delivery, bug targeting and cancer chemotherapy are other typical applications
[6]. Extensive research on hydrogel formulations and dosage-form preferences has widened their biomedical applications and availability to consumers. IHs are gaining traction over the traditional intravenous therapies, which have many systemic toxicities in comparison, including myelosuppression, liver or kidney dysfunctions, non-targeted delivery, prolonged/controlled release and neuro- and other organ-toxicities. IHs can competently avoid these problems by releasing drugs at the infective/tumor site or target sites with localized drug toxicities
[2][4][7][2,4,7].
IHs possesses a unique biocompatibility and hydrophilicity, as well as a phase transitions ability—sol (liquid) to gel (solid) to form solid-like gel states to administer and assist in the encapsulation and release of drugs, genes, DNA, proteins and cells in a sustained and controlled manner
[8]. They are prepared from natural and synthetic polymers through various mechanisms, such as physical and chemical crosslinking methods (discussed in 1.2 classification and synthesis) into different types with their respective advantages and disadvantages
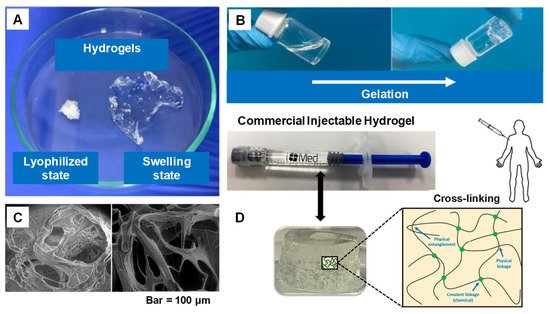
[7]. Some of the characteristics associated with IHs are shown in
Figure 1 [9], whereas
Figure 2 [10] shows the designated and fabricated IHs for photothermal antitumor therapy.
Figure 1. (
A) Swelling ability of hydrogels from lyophilized state. (
B) Example of a gelation time measurement by inverted vial method. (
C) Cross-section SEM images of freeze-dried injectable hyaluronic acid hydrogel. (
D) Physical interactions and chemical linkages of the chemical structure of an injectable hydrogel. Adapted with permission from ref.
[9]. Copyright © 2021
Polymer MDPI.
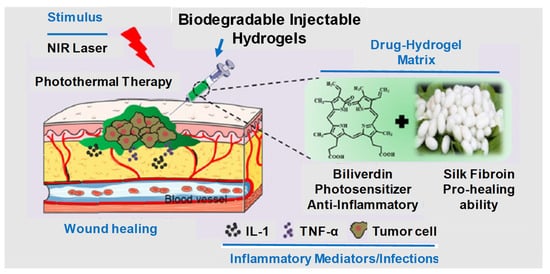
Figure 2. Graphical illustration depicting the design and fabrication of injectable hydrogel for photothermal antitumor therapy and following wound repair and regeneration. Adapted with permission from ref.
[10]. Copyright © 2020
Theranostics.
2. Current Trends
2.1. IHs and Its Application in Drug Delivery System and Biomedical Engineering Applications
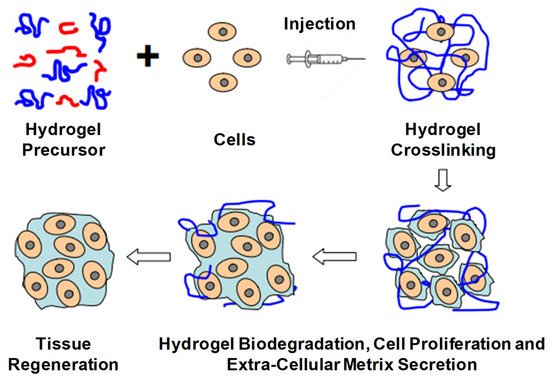
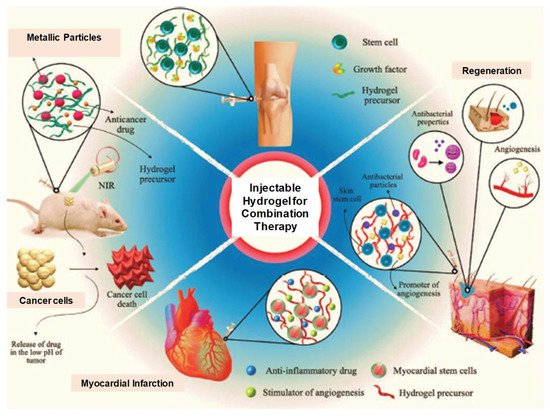
The current trends in biodegradable injectable hydrogel research and its wide application in the biomedical field make it one of the most important therapeutic formulations in drug delivery systems and regenerative medicines—for instance, its application in cartilage regenerations, where its physical properties can be designed such that they can properly match with articular cartilages, in association with their mechanical robustness and scaffold with native tissues. The current research diversifies, proceeds and focuses on the application of gene/drug/DNA/protein delivery, cancer therapy, immunotherapy, tissue regeneration (
Figure 316) and engineering, vaccine delivery, implants, stem cell therapy, wound healing and many more—e.g., controlled, prolonged and sustained release formulations
[9][11][12][13][14][15][16][17][18][19][20][21][22][9,12,13,14,20,25,29,34,43,51,52,53,54].
Figure 316. Schematic illustration of biodegradable injectable hydrogel for tissue regeneration approaches. Cells are isolated from a small biopsy, expanded in vitro and encapsulated in hydrogel precursors, which are subsequently transplanted into the patient by injection using a needle. Hydrogels provide initial structural support and retain cells in the defective area for cell growth, metabolism and new extracellular matrix (ECM) synthesis. The hydrogel is readily degradable when the cells secrete ECM. This strategy enables the clinician to transplant the cell, growth factor and hydrogel combination in a minimally invasive manner. Adapted with permission from ref.
[6]. Copyright © 2010
Material by MDPI.
2.2. Drug Delivery
CAs we know, conventional drug delivery approaches are associated with undesirable drug absorption, rapid metabolism, repeated dosing, systemic toxicities and easy degradation under certain physiological conditions. Injectable hydrogel with sustained drug release properties, degradability and tunable physical properties make it a promising smart drug delivery system, which can overcome and optimize all those disadvantages. Biocompatibility, good syringeability with minimal invasiveness and responsiveness to environmental or enzymatic stimuli make these IHs smart therapeutic systems
[23][41]. In comparison with other systemic or topical administrations, drugs using IHs are promising for controlled biodistribution and sustained release purposes. The 3D structure and water dispersed phase hydrogels can encapsulate water-soluble drugs, though water-insoluble drugs can also be loaded. Macromolecular compounds or bioactive molecules, such as genes, peptides, proteins or even living cells or organs can also be entrapped in hydrogels
[13][22][24][25][14,54,55,56].
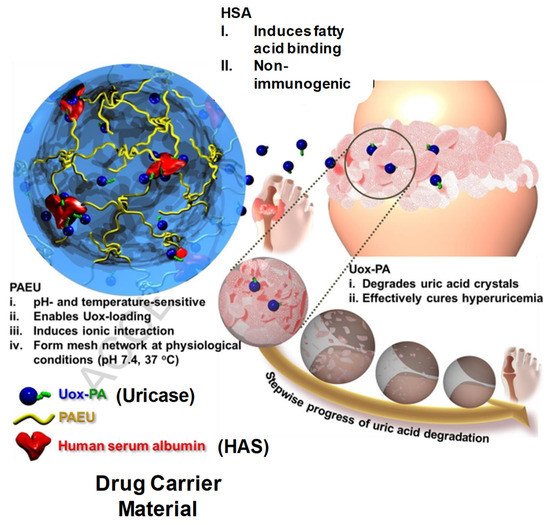
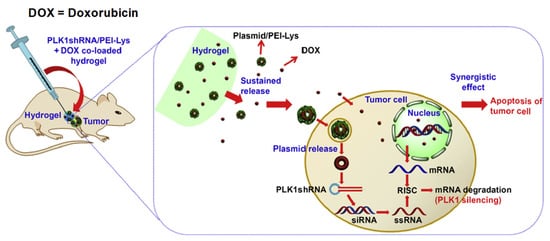
Figure 417 [26][57] and
Figure 518 [27][58] illustrate drug delivery of IHs.
Figure 417. Schematic illustration of Uox-loaded PEG-PAEU/HSA hydrogels and their controlled release of Uox for degradation of uric acid crystals in hyperuricemia mice models. Reprinted with permission from ref.
[26][57]. Copyright © 2017 from
Journal of Control Release, Elsevier.
Figure 518. Schematic illustration for the synergistic effect of PLK1shRNA/PEI-Lys and DOX co-loaded hydrogel on a tumor in nude mice. Reprinted with permission from ref.
[27][58]. Copyright © 2014 from
Biomaterial, Elsevier.
2.3. Therapeutic Applications
2.3.1. Cancer Therapy
Systemic cytotoxicity is associated with the conventional chemotherapy of cancers. The localized non-invasive chemotherapeutics of IHs can overcome the associated toxicities and ensure drug/protein sustained release at tumor sites. In more detail, these IHs (natural and synthetic polymers) are responsive to certain stimuli, such as pH, temperature and immuno-sensitivity, which can be used for cancer chemotherapy/gene therapy or immune therapy
[28][29][30][24][31][36,38,40,55,66]. Some of the commercially available synthetic IHs, such as TraceIT
® and SpaceOAR
®, are therapeutically used for cancerous cell applications, which can protect healthy cells from radiotherapy-induced damage. TraceIT
® contains tissue markers and polyethylene glycol (PEG) hydrogel microparticles, with covalently bond iodine, which helps in the visualization and identification of cancerous tissue for up to three months using ultrasound, computed tomography (CT) and magnetic-resonance imaging (MRI). SpaceOAR
® hydrogel has also been fabricated to protect normal tissues from radiation during radiotherapy for carcinoma. Hence, improving the persistence and rigidity of natural IHs may have significant importance in the treatment of carcinomas and tumors ((
Figure 621)
[32][67] and (
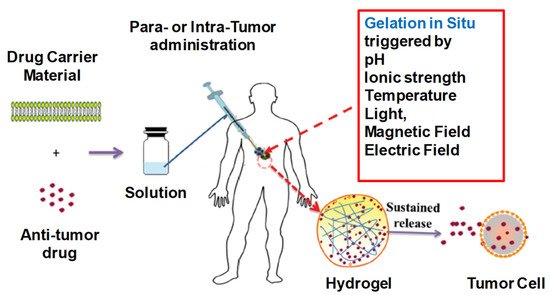
Figure 722)
[28] [36]).
Figure 621. Depiction of in situ gel formation process and its sustained release of drugs from the hydrogel into tumor cells. Reprinted with permission from ref.
[32][67]. Copyright © 2020 from
Drug delivery, Taylor and Francis.
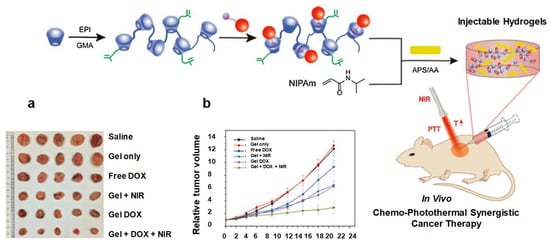
Figure 722. Schematic diagram showing hydrogel formation. (
a) Photograph of excised tumors after mice were euthanized on the 21st day. (
b) Changes in relative tumor volume. Reprinted with permission from ref.
[28][36]. Copyright © 2020 Copyright © 2017,
International Journal of Biological Macromolecules, Elsevier.
2.3.2. Wound Healings
CAs we know, common clinical traumas are associated with tumors, fractures and diabetes, which often go hand in hand with serious infections, including superbugs. Hydrogel dressings with excellent antibacterial properties, bioadhesiveness, good compatibility and biodegradability are preferred over conventional wound healing. They have been fabricated to control infections, improve angiogenesis and uphold angiogenesis. Hydrogels that are photothermal sensitive have the ability to convert NIR irradiation intensity time, photothermal-initiator concentration ratio, cycling time, etc. Increasing the temperature from >50 °C can inhibit bacterial growth effectively, while at 41–43 °C it accelerates wound closure and healing. Nanoparticles (NPs) of copper (GelMA/BACA–Cu) hydrogels possess good photothermal capability under NIR irradiations. After ten minutes of exposure to NIR, hyperthermia (>55 °C) can efficiently inhibit bacterial growth, while its Cu
2+ combination can enhance its antibacterial efficacy. The wound closure rate was 95% in the NIR + GelMA/BACA–Cu NPs hydrogel group, in comparison with the control group, 79%. It also plays a major role in accelerating angiogenesis and encouraging the propagation of fibroblasts. Similarly, Chu et al. developed a NIR + Cu-carbon dots biomaterial in which the wound closure rate reached 96% (control = 62%) after treatments for 14 days, while its H&E staining showed more collagen depositions, neovascularization and re-epithelization in comparison with the control group. However, NIR-induced hyperthermia has short-term antibacterial efficacy, so when it is stopped, the remaining pathogens cannot be effectively inhibited. Therefore, in order to address these concerns issues, some studies have suggested the encapsulation of antibiotics in combination therapies
[33][28][34][21,36,46], see
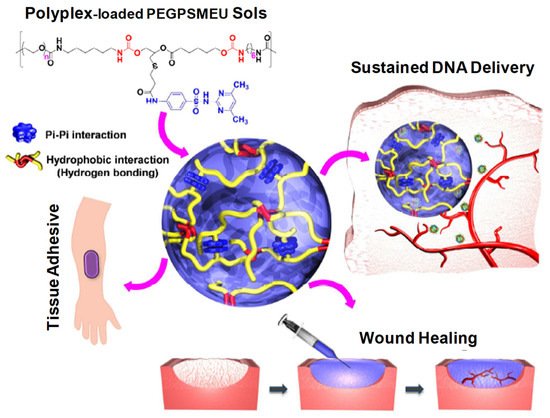
Figure 823 [7] and
Figure 924 [35][42].
Figure 823. Schematic concept of sol-to-gel phase transition of polyplex-loaded PEGPSMEU copolymers sols, subcutaneous administration, controlled released via diffusion, effective absorption onto skin and wound healing. Reprinted with permission from ref.
[7]. Copyright © 2020 from
Journal of Controlled Release, Elsevier.
Figure 924. Illustration of the potential application of multifunctional IHs for cancer multi-therapy as well as regeneration after tissue damage. Reprinted with permission from ref.
[35][42]. Copyright © 2020
Advance Health Care Materials, Wiley-VCH GmbH.
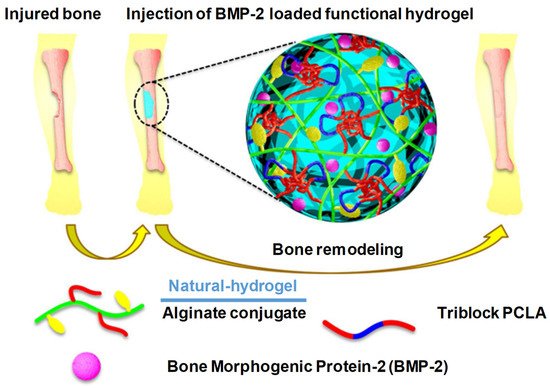
2.3.3. Bone Regeneration
According to Kim et al., alginate-based conjugating temperature-responsive poly(ε-caprolactone-co-lactide)-b-poly(ethylene glycol)-b-poly(ε-caprolactone-co-lactide) and O-phosphoryl-ethanolamine can be used as phosphorylation functional groups (PCLA-b-PEG-b-PCLA-/Alg) to obtain bioconjugate-injectable scaffold systems that have the ability to accelerate bone biomineralization
[12][13] (
Figure 1025). When the temperature was elevated from room temperature to physiological temperature, these bioconjugates showed a sol–gel transition. In in vivo and in vitro situ biomineralization, the XRD analysis confirmed that such bioconjugate hydrogel could result in a reduction in crystalline hydroxyl apatite, and it also released BMP-2 (mitogenic factors) for more than three days. These BMP-2-containing PCLA-b-PEG-b-PCLA/Alg bioconjugate hydrogels also possess calcium deposition at the eroded sites, which suggests mineralization and bone regeneration; see
Figure 1025 [12][20][13,52].
Figure 1025. Schematic illustration of recruitment of host cells into PCLA-b-PEG-b-PCLA/BSA hydrogels and subsequent activation in response to DNA vaccine-bearing polyplexes released from these hydrogels. Reprinted with permission from ref.
[7]. Copyright © 2020 from
Journal of Controlled Release, Elsevier.
3. Future Prospects
3.1. Limitations and Outcomes/Overcomes
Regarding their current prospective and ongoing research, hydrogel formulations have some limitations in their applications, clinical practices and sustainability. Many hydrogel systems (natural/synthetic), such as thermosensitive hydrogels, as mentioned, are free-flowing sols at a low temperature, while upon raising to body temperature (physiological temperature), they are converted to a stable visco-elastic gel phase, such as poly (phosphazene), pluronic and poly (
N-isopropyl acrylamide). However, their biomedical uses are restricted due to their limited non-biodegradable and biocompatible characteristics, as shown in
Table 15. However, poly (ester)-based copolymers are a good alternative for overcoming these limitations, but they still require more extensive research. Moreover, PEG and poly(ester)-based hydrogels (local drug-carriers) are not effective for prolonged therapeutics. Their oral and nasal route administrations are inappropriate, though they have been approved by the FDA for in vivo implantation. Similarly, injectable hydrogels used for proteins and peptide-controlled delivery, chemical interactions, structure compatibilities and burst release (when charged proteins are added to uncharged formulations) are also facing future challenges
[12][13].
Table 15.
Injectable hydrogels synthesized through chemical and physical crosslinking methods, their application and limitations.
| Chemical/Physical Crosslinking |
Types of Hydrogel Material |
Hydrogel Synthesis Procedure |
Applications and Advantages |
Limitations and Disadvantages |
Reference |
| Hydrophobic interaction |
Hydrophilic monomers and hydrophobic co-monomers |
Free radical copolymerization of a hydrophilic monomer with a hydrophobic co-monomer |
Absence of crosslinking agents and relative ease of production |
Poor mechanical characteristics |
[36][65] |
| Ionic interaction |
Solution and multivalent ions of opposite charge |
Polyelectrolyte ionic interaction through simple ion exchange mechanisms and complex formation |
Crosslinking takes place at room temperature and physiological pH Properties can be fine-tuned by cationic and anionic constituents |
Limited to ionic polymers and sensitive to impurities |
[31][66] |
| Hydrogen bond |
Polymeric functional groups of high electron density with electron-deficient hydrogen atom |
Self-assembly through secondary molecular interactions |
Increase in polymer concentration can increase the stability of gel |
Influx of water can disperse/dissolve the gel within short duration |
[32][67] |
| Bulk polymerization |
Monomers and monomer-soluble initiators |
The polymerization reaction is initiated with radiation, ultraviolet or chemical catalysts at low rate of conversions |
A simple and versatile technique for preparing hydrogels with desired physical properties and forms |
Increase in viscosity during high rate of polymerization reaction can generate heat Weak polymer structure |
[37][68] |
| Solution polymerization |
Ionic or neutral monomers with the multifunctional crosslinking agent |
Reaction initiated thermally with UV irradiation or by redox initiator system |
Control of temperature
Performed in non-toxic aqueous medium at room temperature
High polymerization rate |
To be washed to eliminate reactants, the polymers and other impurities |
[38][69] |
| Suspension polymerization |
Hydrophilic monomers, initiators, cross-linkers and suspending agent |
The monomers and initiator are dispersed in the organic phase as a homogenous mixture |
Directly usable as powders, beads or microspheres
Restricted to water insoluble polymer |
Cooling jacket required to dissipate heat
Requirement of agitators and dispersant |
[39][70] |
| Grafting |
Viny polymers, initiators and crosslinking agents |
Covalent bonding of monomers on free radicals generated on stronger support structures |
Improve functional properties of the polymer |
Difficulty of characterizing side chains |
[40][71] |
| Irradiation |
High energy gamma beams and electron beams as initiators |
Irradiation of aqueous polymer solution results in the formation of radicals and macroradicals on the polymer chains |
Pure, sterile, residue-free hydrogel
Does not require catalyst and other additives
Irradiation dose can control swelling capacity |
Irradiation can cause polymer degradation via chain scission and crosslinking events |
[41][72] |
| Step growth polymerization |
Bi- or multifunctional monomers and each with attest two sites for bonding |
Multifunctional monomers react to form oligomers resulting in long chain polymers |
No initiator is required to start the polymerization and termination reactions |
Prolonged reaction times required to achieve a high degree of conversion and high molecular weights |
[42][73] |
In enzymatic stimuli responsiveness, fragile molecules, such as proteins, cells and drugs, are degraded or denatured by the use of cross-linker monomers and toxic catalysts. Homogenous encapsulation, loading and pre-mature release are also associated limitations and concerns
[4].
3.2. Injectable Formulation Challenges
Here, reswearchers describe the ongoing prospective of a targeted drug delivery system that improves the therapeutic regimen and enables target-specific delivery. In addition, self-assembled nanocarriers and their active targeting receptors/antigen overexpression in tumor cells are prospective major therapeutic approaches.
IHs, along with their specific applications, which have been already discussed, have some common notable concerns and require further exploration. The compatibility of the fragile molecules or cells with hydrogel crosslinkings and proliferation maintenance within a healthier environment are of the utmost importance, while they are essential for protecting DNA, peptides, proteins and oligonucleotides from enzymatic degradation or denaturation. Cytotoxicity and inflammatory responses need to be avoided by under-standing their interactions with the cellular and surrounding tissues. Low reproducibility; poorly defined structures; employed system considerations, including the gelation mechanism, rate kinetics, viscosity during the injection time; mechanical sturdiness after gelation; the degradation period; and release profile of bioactive factors should be properly taken in account
[43][31]. It should be noted that these IHs must have application-specific design measurements related to their chemical–physical crosslinking and biological computability, which should be specific and responsive to certain medical conditions or pathogenesis
[33][26][21,57].
3.2.1. Mechanical Robustness
The maintenance of a low viscosity and sustainability of sufficient elasticity in situ for repetitive load and volume is a major design challenge
[44][32]. As these hydrogels are administered through a needle and syringe, in situ gelation and repetitive doses are of great concern. Shear thinning polymers, such as hyaluronic acid, which are currently used as a dermal filler, are being replaced by an injectable for cartilage replacement
[2][45][46][2,11,15]. Thus, the polymer molecular weight, chains, extent of crosslinking and crosslinking mechanism and viscosity have a linear relationship with the molecular weight, while the elastic modulus has an inverse relation
[15][26][25,57].
3.2.2. Loading and Release of Therapeutic Agents
The loading and release of therapeutic agents, such as small drug molecules, macromolecules (peptides, proteins, nucleic acid, etc.) or living cells, can be conveyed to the surrounding environment through IH carriers, which have respective physico-chemical characteristics. Their effective release is determined by the cargo-gel size, affinity and interactions. Currently, IHs in clinic practice include microparticle depot systems (small molecules or biologics). The most commonly available depot formulations are lidocaine (anesthetic agent), with a number of hyaluronic acid hydrogel injectables that have been approved for facial corrections. Hydrogel meshes disturb lidocaine release due to its rapid release from these gels. Similarly, the elution of other drugs from hydrogel formulations for the sustained release of proteins/drugs in wound dressings is vital
[15][25]. In such formulations, the hydrogel mesh size should be decreased via physical/chemical crosslinking to agitate the solute elution or increase its affinity to enhance its retention time
[36][65].
3.2.3. Hydrogel Bioactivity
The bulk hydrogel material must penetrate, alter and degrade bulk hydrogel materials for tissue regeneration purposes. For hydrogel bioactivity, it is essential that cells or growth factors stick to adhesive natural or synthetic materials such as hyaluronic acid, fibrin or gelatin. For instance, in some ongoing clinical trials, e.g., NCT04115345, NCT04115345 and NCT00981006, the hydrogel bioactivity of gelatin is used with cells and/growth factors. These bioactive hydrogels expedite kidney or myocardium tissue injury healing by generating a suitable cell-adhesive microenvironment. Some non-adhesive polymers, such as PEG and polyacrylamide, must be amended chemically with adhesive ligands to assist cell penetration and attachment. Conversely, some commercially available hydrogels, e.g., TraceIT
®, which is used for targeting tumor margins, have the design limitation of rapid biodegradation. Thus, it is essential to use or substitute a polymer hydrogel that degrades gradually over weeks to months
[1][10][11][15][47][1,10,12,25,64].
3.2.4. Immunological Compatibility
Provoking immunological responses to IH biomaterials has been a considerable area of research in recent decades. Thus, in injectable hydrogel formulations, it is imperative to minimize all kinds of immune responses during in situ gel transitions
[48][49][74,75]. Immunological responses are considered as the worst consequences of biomaterial injection, insertion and implantation, including inflammatory cascades, fibrosis and hypersensitivity reactions. These responses are considered harmful in their own prospects, associated physico-chemical shifts and responsiveness (i.e., changes in the local pH or temperature), which can affect the hydrogel material performance, function and further application
[50][76]. Thus, minimalizing IH-associated host-immune responses is a critical biological design parameter. Cell-based drug delivery systems (erythrocytes, leukocytes, platelets, cancer cells and hepatic cell membrane biomimetic nanosystem fabrications) can be utilized for immunocompatibility, immune escaping, prolonged release and sustained release
[51][52][53][54][55][56][57][58][59][60][61][62][63][77,78,79,80,81,82,83,84,85,86,87,88,89]. Some hydrogels have been used in these cell-based fabricated biomimetic nanosystems
[64][90].
3.2.5. Technological Challenges
Technological challenges, including chemistry, good manufacturing practices (GMP), controlled and well-defined regulatory guidelines, practical adoptability and high prices are major hurdles for successful clinical translations of hydrogel-based delivery systems. It is estimated that hydrogel fabrication system development and fabrication costs through clinical translation range from USD 50 million up to USD 800 million.
3.2.6. Scale-Up Strategies and GMP Processes
As most hydrogel systems are generated and synthesized at a small pilot-plant scale at pre-clinical stages, current good manufacturing practices (cGMP) for the clinical translation and integration of biomaterial-based hydrogels in large-scaled systems and their compatibility are required. Robustness, batch-to-batch variations, safety profiles, reproducibility and proficiency are predictable when executed at a large scale. Moreover, the high water content of hydrogels makes the synthesis, fabrication, storage, sustainability, sterilization and all relevant optimization processes even more demanding.
3.2.7. Regulatory Approvals
As
reswe
archers mentioned earlier, regulatory affairs and FDA approval are time-consuming processes and take years—from laboratory synthesis to market launch and surveillance. The diversity in injectable hydrogel scaffolds and the assortment of employed crosslinking polymers and biomaterials render their regulatory classification and approval challenging
[15][25].