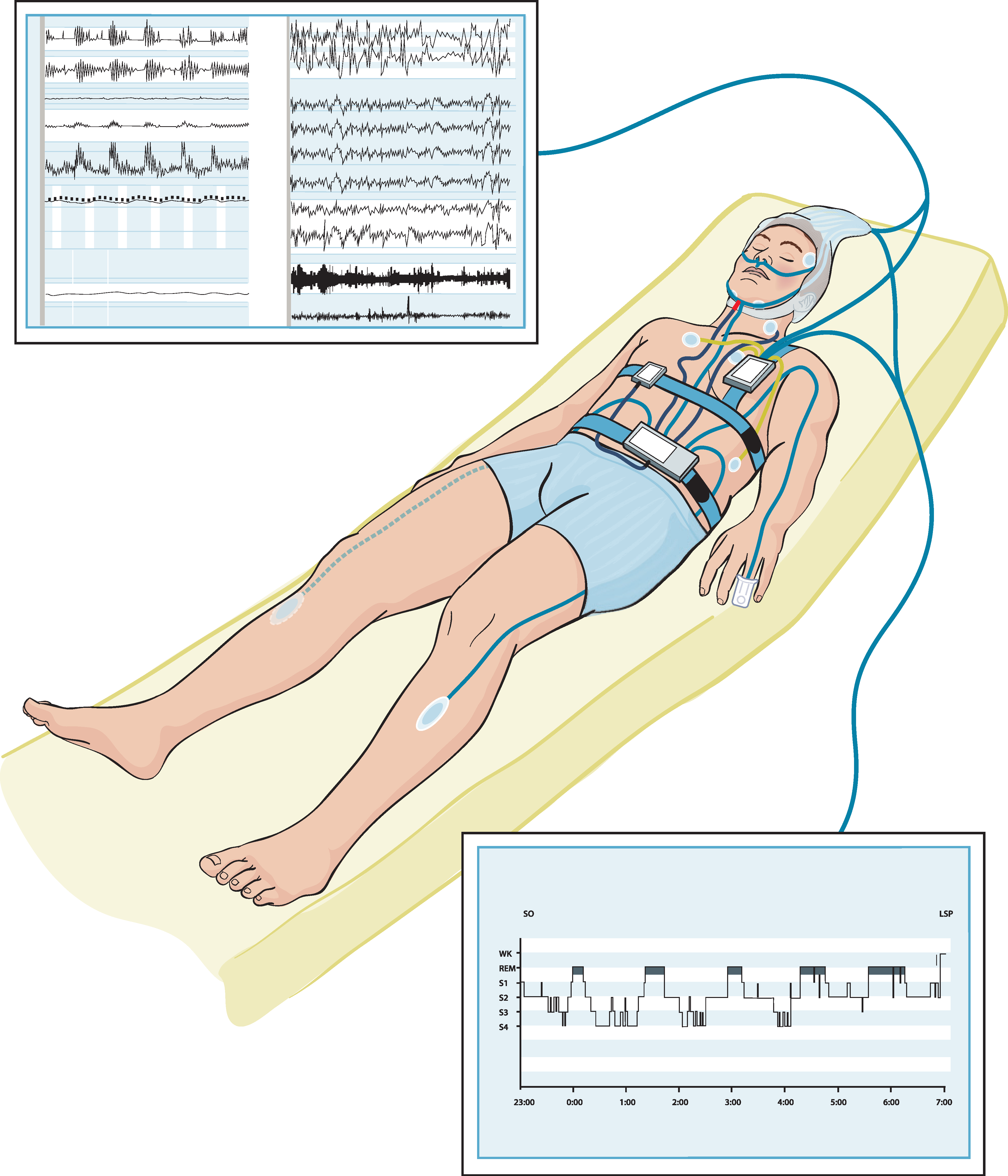
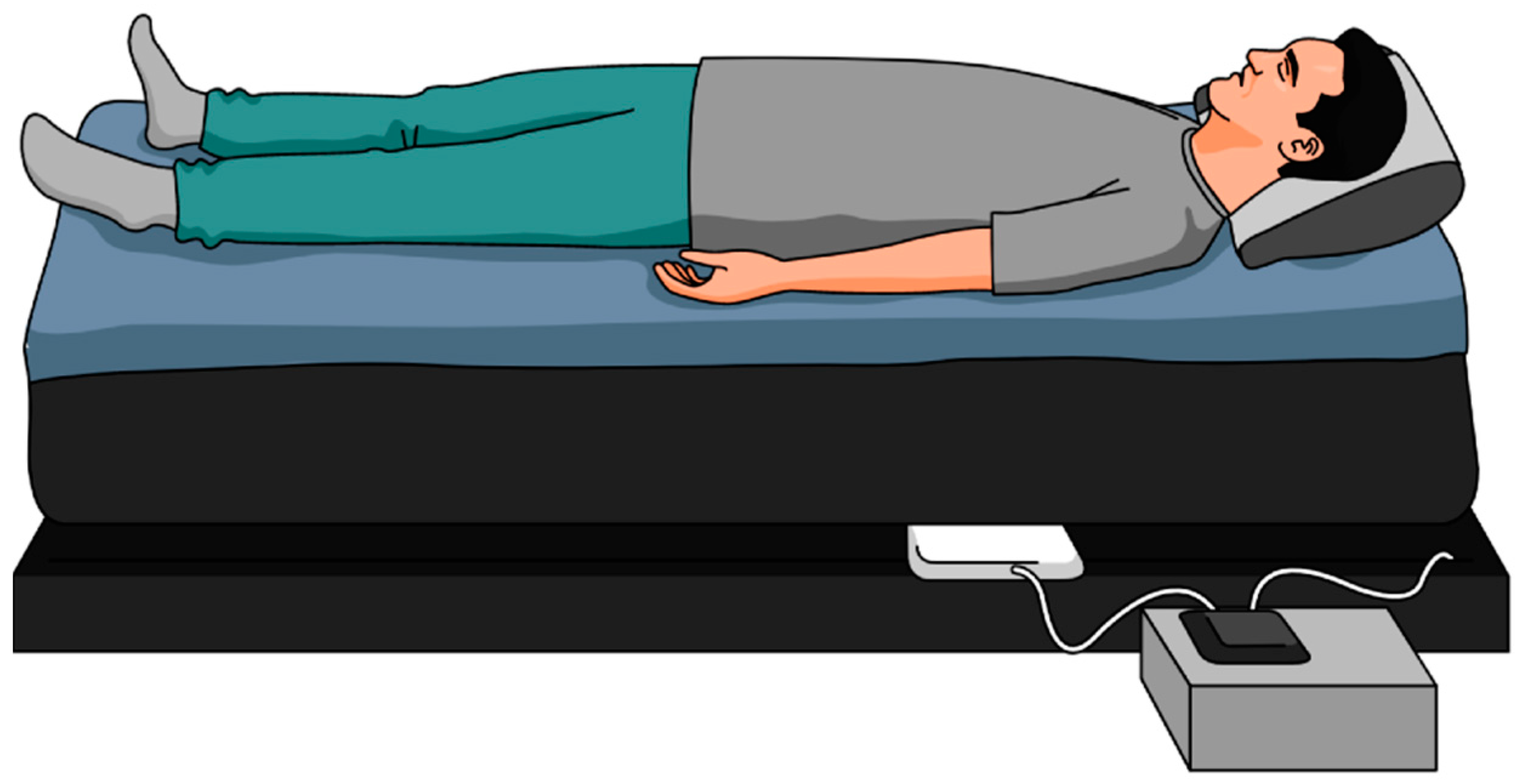
Polysomnography is the gold-standard method for measuring sleep but is inconvenient and limited to a laboratory or a hospital setting. As a result, the vast majority of patients do not receive a proper diagnosis. In an attempt to solve this issue, sleep experts are continually looking for unobtrusive and affordable alternatives that can provide longitudinal sleep tracking. Collecting longitudinal data on sleep can accelerate epidemiological studies exploring the effect of sleep on health and disease. These alternatives can be in the form of wearables (e.g., actigraphs) or nonwearable (e.g., under-mattress sleep trackers).
- ballistocardiography
- sleep cycles
- home monitoring
1. Introduction
2. Current Insights of Sleep Monitoring Methods
It can be noted that there is an increasing interest in sleep monitoring (in particular, sleep cycles) using unobtrusive sensors. Due to the unsuitability of PSG for in-home monitoring, researchers have developed and are developing various unobtrusive systems as alternatives, leveraging on recent technological advancements. Generally, proposed sleep monitoring methods are based on one or a combination of the following: respiratory cycle, cardiac cycle, body movement [20][34]. It was also observed that the majority of the proposed systems are limited to three-stage sleep classification [20][34]. Although the results from the abovementioned studies are encouraging in terms of accuracy, commercial devices cannot produce identical results to PSG. It makes sense because EEG-based systems are the most accurate for detecting all the stages of sleep [21][35].
That said, the ease and relative performance of actigraphy-based devices for sleep and sleep-cycle monitoring has given rise to numerous wearable devices and smartphone-based technologies. Actigraphy devices enable the user to wear dedicated sensors to help track vital signs and movements while sleeping. ItThis is shownreview shows that the use of wearable devices for sleep-cycle monitoring is feasible but inaccurate compared to the gold standard PSG [22][23][24][30,36,37]. This is because even in healthy adults accelerometry has high sensitivity but low specificity for sleep detection. These devices often tend to underestimate or overestimate some key parameters such as TST, sleep efficiency, wake, or the transition between the sleep stages [22][23][24][30,36,37]. Patients with sleep disorders, or those who are chronically sleep-deprived, are more likely to suffer from fragmented sleep and reduced ability to understand their functional impairment. Therefore, wearing sleep trackers with incorrect readings could have adverse effects on these patients. This happens because most patients do not realize that the claims of these devices typically outweigh the science to support them as devices to measure and improve sleep. As a result, the importance of precise measurements cannot be overstated [23][36].
A recent study by Chinoy et al. [25][38] has shown that off-the-shelf sleep trackers (i.e., Fatigue Science Readiband, Fitbit Alta HR, EarlySense Live, ResMed S+, SleepScore Max) provided mixed results for sleep stage classification and the trackers tended to perform worse on nights with poorer/disrupted sleep. Similarly, Roomkham et al. [26][39] have come to the same conclusion that further studies are needed to assess the longer-term performance of sleep trackers, namely, the Apple Watch in natural conditions, and against PSG in clinical settings. Furthermore, Kholghi et al. [27][40] concluded that EMFIT QS failed to distinguish sleep stages against PSG and additional development is needed before using EMIFT QS in clinical settings. Moreover, studies have shown that although smartphone-based sensing systems are simpler and less expensive, they correlate poorly with the PSG [28][41].
