The recent pandemic caused by Sars-Cov-2 has caused a lot of confusion regarding containment protocols. Unfortunately, many of the characteristics of this virus are still unclear. The purpose of this article is to clarify what are the current notions regarding the persistence of the virus in the environment. Different factors were considered such as surfaces, temperature, humidity and pH; in relation to the inactivation time of the virus.
- Sars-Cov-2
- Coronavirus
- Virus
- Persistance
- enviroinments
- disinfection
- surfaces
- temperature
- humidity
Note:All the information in this draft can be edited by authors. And the entry will be online only after authors edit and submit it.
Definition:The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is responsible for the Coronavirus disease 2019 (COVID-19). The incubation period of this infectious disease varies from about 2 to 14 days (with some reported cases of 29 days), during this time the patient could be contagious [1,2].
1. Introduction
Coronaviruses are responsible for respiratory diseases, from the common cold to severe ones, such as Middle Eastern respiratory syndrome (MERS) and severe acute respiratory syndrome (SARS). They are spherical viruses, covered with a helically symmetrical capsid and a pericapsid crossed by glycoprotein structures that give it the typical ‘crown’ appearance. The viral genome consists of single-stranded RNA. The Orthocoronavirinae subfamily of the Coronaviridae family includes four coronavirus (CoV) genera: Alpha-, Beta-, Delta- and Gamma-coronavirus. The betacoronavirus is divided into five subgenera. Coronaviruses are capable of infecting both humans and some animal species, these viruses were first identified around the 1960s. Epithelial cells of the respiratory and gastrointestinal tract are those mainly affected by these viruses. To date, seven Coronaviruses are able to infect humans:
2. Data Description
2.1. Data Features
Results were singularly analyzed by the authors, and items about viruses’ persistence on different surface materials were evaluated and shown as follow:
A table has been designed to show a summary of inherent virus features.
The
1 items are as follows:
| Virus | Authors and Year | |||
|---|---|---|---|---|
| ] | aerosols | 3 h | Reduction from 103.5 to 102.7 TCID | |
| 2019-nCoV | Van Doremalen et al. 2020 [3] | aerosols | 3 h | Reduction from 103.5 to 102.7 TCID |
| 50 | ||||
| per liter of air | ||||
| plastic | 72 h | Reduction from 103.7 to 100.6 TCID | ||
| 50 | ||||
| per millimeter | ||||
| stainless steel | 48 h | from 103.7 to 100.6 TCID | ||
| Paper | 3 h | From 4.76 TCID | ||
| 50 | ||||
| at 0 min to 2.18 TCID | ||||
| 50 | ||||
| at 30 min | ||||
| Wood | 48 h | From 5.66 TCID | ||
| 50 | ||||
| at 0 min to 2.47 TCID | ||||
| 50 | ||||
| at 6 h | ||||
| Cloth | 48 h | From 4.84 TCID | ||
| 50 | ||||
| at 0 min to 2.25 TCID | ||||
| 50 | ||||
| at 6 h | ||||
| Glass | 96 h | From 5.83 TCID | ||
| 50 | ||||
| at 0 min to 5.06 TCID | ||||
| 50 | ||||
| at 6 h | ||||
| Stainless Steel | 7 days | From 5.80 TCID | ||
| 50 | ||||
| at 0 min to 5.24 TCID | ||||
| 50 | ||||
| at 6 h | ||||
| Plastic | 7 days | From 5.81 TCID | ||
| 50 | ||||
| at 0 min to 4.68 TCID | ||||
| 50 | ||||
| at 6 h | ||||
| Mask (inner layer) | 7 days | From 5.88 TCID | ||
| 50 | ||||
| at 0 min to 5.01 TCID | ||||
| 50 | Kampf et al. 2020 [34] | paper | 5 min up to 5 days | 10 |
| Kampf et al. 2020 [5] | paper | 5 min up to 5 days | 10 | |
| 5 | ||||
| TCID | ||||
| 50 | ||||
| per millimeter | ||||
| glass | 4–5 days | 10 | ||
| 4 | ||||
| TCID | ||||
| 50 | ||||
| per millimeter | ||||
| plastic | 2–9 days | 10 | ||
| 6 | ||||
| TCID | ||||
| 50 | ||||
| per millimeter | ||||
| PVC | 5 days | 10 | ||
| 3 | ||||
| TCID | ||||
| 50 | ||||
| per millimeter | ||||
| silicon rubber | 5 days | 10 | ||
| 3 | ||||
| TCID | ||||
| 50 | ||||
| per millimeter | ||||
| surgical gloves (latex) | 5 days | 10 | ||
| 3 | ||||
| TCID | ||||
| 50 | ||||
| per millimeter | ||||
| disposable gowns | 1–2 days | 10 | ||
| 5 | ||||
| TCID | ||||
| 50 | ||||
| per millimeter | ||||
| Warnes et al. 2015 [35] | polyfluorotetraethylene (PTFE) | 5 days | 10 | |
| Warnes et al. 2015 [6] | polyfluorotetraethylene (PTFE) | 5 days | 10 | |
| 3 | ||||
| TCID | ||||
| 50 | ||||
| per millimeter | ||||
| ceramic | 5 days | 10 | ||
| 3 | ||||
| TCID | ||||
| 50 | ||||
| per millimeter | ||||
| glass | 5 days | 10 | ||
| 3 | ||||
| TCID | ||||
| 50 | ||||
| per millimeter | ||||
| stainless steel | 5 days | 10 | ||
| 3 | ||||
| TCID | ||||
| 50 | ||||
| per millimeter |
-
Common human coronaviruses: HCoV-OC43 and HCoV-HKU1 (Betacoronavirus) and HCoV-229E and HCoV-NL63 (Alphacoronavirus); they cause common colds and severe lower respiratory infections
-
other human Coronaviruses (Betacoronavirus): SARS-CoV, MERS-CoV and 2019-nCoV (now called SARS-CoV-2).
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is responsible for the Coronavirus disease 2019 (COVID-19). The incubation period of this infectious disease varies from about 2 to 14 days (with some reported cases of 29 days), during this time the patient could be contagious [1,2][1][2]. COVID-19 is due to Coronavirus SARS-CoV-2 infection. The new coronavirus was named Coronavirus SARS-CoV-2 by the Coronavirus study group of the International Committee on Taxonomy of Viruses (the commission responsible for classifying and naming viruses) because it was considered to be a “brother” of the virus responsible for SARS (SARS- CoV).
Coronaviruses are common in animal species such as bats and camels, but they can evolve and infect humans; this ability of viruses in the animal world to become pathogenic to humans is called “species jump” or spillover. To date, seven types of human coronavirus have been discovered, the first were identified in the mid-seventies, while the last are recent (SARS-CoV, 2002; MERS-CoV, 2012), up to the new coronavirus SARS-CoV-2 of 2019.
| Investigated Material | Time | Note on Results |
|---|
| 2019-nCoV | Van Doremalen et al. 2020 [32 | |||
| 50 | ||||
| per millimeter | ||||
| copper | 4 h | No viable SARS-CoV-2 | ||
| cardboard | 24 h | No viable SARS-CoV-2 | ||
| 2019-nCoV | Chin et al. [33] | Paper | 3 h | From 4.76 TCID |
| 2019-nCoV | Chin et al. [4] | |||
| at 6 h | ||||
| Mask (outer layer) | ||||
| / | From 5.78 TCID | |||
| 50 | ||||
| at 0 min to 4.97 TCID | ||||
| 50 | ||||
| at 6 h to 2.79 at 7 days | ||||
| Other coronaviruses | Van Doremalen et al. 2020 [32] | aerosols | 3 h | reduction from 104.3 to 103.5 TCID |
| Other coronaviruses | Van Doremalen et al. 2020 [3] | aerosols | 3 h | reduction from 104.3 to 103.5 TCID |
| 50 | ||||
| per liter of air | ||||
| plastic | 72 h | from 103.4 to 100.7 TCID | ||
| 50 | ||||
| per millimeter | ||||
| stainless steel | 48 h | from 103.6 to 100.6 TCID | ||
| 50 | ||||
| per millimeter | ||||
| copper | 8 h | No viable SARS-CoV-1 | ||
| cardboard | 8 h | No viable SARS-CoV-1 | ||
| polyvinyl chloride (PVC) | 5 days | 10 | ||
| 3 | ||||
| TCID | ||||
| 50 | ||||
| per millimeter | ||||
| silicon rubber | 3 days | 10 | ||
| 3 | ||||
| TCID | ||||
| 50 | ||||
| per millimeter | ||||
| brasses containing copper | <40 min | 10 | ||
| 3 | ||||
| TCID | ||||
| 50 | ||||
| per millimeter | ||||
| copper nickels | 120 min | 10 | ||
| 3 | ||||
| TCID | ||||
| 50 | ||||
| per millimeter | ||||
| zinc | 60 min |
2.2. Data Synthesis
According to the World Health Organization (WHO), the transmission of coronavirus infections, including SARS-CoV-2, occurs through droplets, droplets of diameter ≥ 5 μm that originate from the acts of breathing, speaking, coughing and sneezing. Due to their size, the droplets travel in the air for short distances, generally less than one meter, and can directly reach susceptible subjects in the immediate vicinity, as well as settling on objects or surfaces that therefore become a source of spread of the virus. In fact, in this case, hands that have come into contact with the so contaminated objects can constitute a vehicle of transmission by indirect contact when they touch the mouth, nose and eyes. Given that hand washing is always the cornerstone of correct prevention, regular cleaning followed by disinfection of surfaces and internal environments play a crucial role in preventing and containing the spread of the virus. Studies on coronaviruses, not SARS-CoV-2, such as the SARS and MERS virus, suggest that the survival time of these pathogens on surfaces, in experimental conditions, varies from a few hours to a few days depending on the material involved, concentration, temperature and humidity. It should be emphasized that this data refers to the finding of the virus RNA and not to its isolation in vital form, and therefore not related to its real infectivity [16,25,26,39,40,41,42][7][8][9][10][11][12][13].
2.2.1. Coronaviruses in Different Temperatures and Humidity
A recent study of Chin et al. [33] [4] assessed the stability of the SARS-CoV-2 virus at different temperatures, showing that the virus is highly stable at 4 °C, but sensitive to heat. In fact, at 4 °C there was a reduction of about 0.7 logarithmic units of the viral titre on the 14th day. By increasing the incubation temperature to 56 °C, a significant decrease in viral infectivity was observed within 10 min and, after 30 min, the virus was no longer detectable. Raising the temperature to 70 °C, the virus was no longer detectable after 5 min. The stability of the SARS-CoV-2 virus on different surfaces was also assessed in the same study. The viral titer on each surface was determined after 30 min, 3 h, 6 h, 1 day, 2 days, 4 days and 7 days of incubation, as illustrated in Table 21, Table 32 and Table 43 (Figure 1). The real novelty of this study is that persistence on some surfaces, such as the external surface of the masks, can last up to seven days [43][14]. Different pH seems to not statistically influence the virus persistence (Table 43). The factors influencing the persistence of microorganisms in the air/aerosol can be defined as:
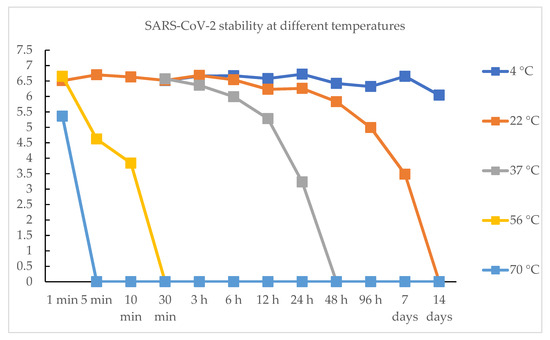
Figure 1. SARS-CoV-2 stability at different temperature over time. TCID50 on y axis and time on x axis (0 is equal to “not detectable” virus (≤103 TCID50/mL)).
Table 32. Stability of SARS-CoV-2 at different temperatures (“/”: not available data).
Table 43. Stability of SARS-CoV-2 at different pH.
Relative humidity of the air;
-
Air temperature and sunlight;
-
Aerosol composition.
| Time | 4 °C | 22 °C | 37 °C | 56 °C | 70 °C |
|---|
| pH | Log TCID50/mL |
|---|
| 1 min | / | 6.51 TCID50 | / | 6.65 TCID50 | 5.36 TCID50 |
| 3 | 5.55 | ||||||
| 5 min | / | 6.7 TCID50 | / | 4.62 TCID50 | / | ||
| 4 | 5.67 | 30 min | 6.51 TCID50 | 6.52 TCID50 | 6.57 TCID50 | / | / |
| 6 h | |||||||
| 5 | 5.73 | 6.67 TCID50 | 6.54 TCID50 | 5.99 TCID50 | / | / | |
| 6 | 5.75 | 12 h | 6.58 TCID50 | 6.23 TCID50 | 5.28 TCID50 | / | / |
| 24 h | 6.72 TCID50 | 6.26 TCID50 | 3.23 TCID50 | / | / | ||
| 7 days | 6.65 TCID50 | 3.48 TCID50 | / | / | / | ||
| 14 days | 6.04 TCID50 | / | / | / | / |
| 7 | |
| 5.58 | |
| 8 | 5.70 |
| 9 | 5.54 |
| 10 | 5.51 |
-
Resistance of the microorganism;
Always considering that the air sampling method can affect the obtained results.
3. Conclusions
It currently appears that the persistence of the virus is favored by a low temperature (4 °C) and is gradually inactivated by the increase of the latter. Furthermore, could be said how the pH weakly influence this persistence unlike the type of surface, in fact plastic has the longest persistence times of the virus in active form instead of surfaces with active properties against the virus such as copper, where it is inactivated in a few hours. Having these results regarding temperature, humidity and surface material is useful for setting guidelines for prevention. Certainly, other studies would be useful, and should further clarify the resistance to climatic conditions of this virus. It would be useful to understand if the conditions of pollution or particulate matter in the air can favor the persistence of the virus in the aerosol, and also to evaluate the effectiveness of the sun’s rays. It would also be interesting to know if the virus has different persistence times on human skin, or if some virucidal activity is carried out against it.
References
- Centers for Disease Control and Prevention. Symptoms of Coronavirus. Available online: https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fabout%2Fsymptoms.html (accessed on 17 August 2020).
- Expert Reaction to News Reports That the China Coronavirus May Spread before Symptoms Show. Available online: https://www.sciencemediacentre.org/expert-reaction-to-news-reports-that-the-china-coronavirus-may-spread-before-symptoms-show/ (accessed on 17 August 2020).
- Neeltje Van Doremalen; Trenton J Bushmaker; Dylan H. Morris; Myndi G. Holbrook; Amandine Gamble; Brandi N. Williamson; Azaibi Tamin; Jennifer Harcourt; Natalie J. Thornburg; Susan Gerber; et al.James O. Lloyd-SmithEmmie De WitVincent J. Munster Aerosol and surface stability of HCoV-19 (SARS-CoV-2) compared to SARS-CoV-1. N. Engl. J. Med. 2020, 382, 1564-1567, 10.1101/2020.03.09.20033217.
- Alex W H Chin; Julie T S Chu; Mahen R A Perera; Kenrie P Y Hui; Hui-Ling Yen; Michael C W Chan; Malik Peiris; Leo L. M. Poon; Stability of SARS-CoV-2 in different environmental conditions. The Lancet Microbe 2020, 1, e10-e10, 10.1016/s2666-5247(20)30003-3.
- Günter Kampf; Daniel Todt; Stephanie Pfaender; Eike Steinmann; Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. Journal of Hospital Infection 2020, 104, 246-251, 10.1016/j.jhin.2020.01.022.
- Sarah L. Warnes; Zoë R. Little; C. William Keevil; Human Coronavirus 229E Remains Infectious on Common Touch Surface Materials. mBio 2015, 6, -15, 10.1128/mbio.01697-15.
- The Lancet; COVID-19: fighting panic with information. The Lancet 2020, 395, 537-537, 10.1016/s0140-6736(20)30379-2.
- Mascitti, M.; Campisi, G. Dental Public Health Landscape: Challenges, Technological Innovation and Opportunities in the 21st Century and COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 3636.
- Cervino, G.; Oteri, G. COVID-19 Pandemic and Telephone Triage before Attending Medical Office: Problem or Opportunity? Medicina 2020, 56, 250.
- Paoli, A.; Musumeci, G. Elite Athletes and COVID-19 Lockdown: Future Health Concerns for an Entire Sector. J. Funct. Morphol. Kinesiol. 2020, 5, 30.
- Giudice, A.; Barone, S.; Muraca, D.; Averta, F.; Diodati, F.; Antonelli, A.; Fortunato, L. Can Teledentistry Improve the Monitoring of Patients during the Covid-19 Dissemination? A Descriptive Pilot Study. Int. J. Environ. Res. Public Health 2020, 17, 3399.
- Cavallo, L.; Marcianò, A.; Cicciù, M.; Oteri, G. 3D Printing beyond Dentistry during COVID 19 Epidemic: A Technical Note for Producing Connectors to Breathing Devices. Prosthesis 2020, 2, 46–52.
- Fiorillo, L.; Leanza, T. Worldwide 3D Printers against the New Coronavirus. Prosthesis 2020, 2, 9.
- Jacques Demongeot; Yannis Flet-Berliac; Hervé Seligmann; Temperature Decreases Spread Parameters of the New Covid-19 Case Dynamics. Biology 2020, 9, 94, 10.3390/biology9050094.
