Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 3 by Jessie Wu and Version 2 by Jessie Wu.
The surgical extraction of the lower third molars is widely practiced in oral surgery. Subsequent inflammatory complications such as pain, facial swelling, and trismus can negatively affect the quality of life of the patients. Non-medication methods used to minimize tissue injury after third-molar extraction and without side effects include the use of photobiomodulation.
- photobiomodulation
- laser
- low level laser therapy
- tooth extraction
- oral surgery
- pain
- swelling
- trismus
1. Introduction
The surgical extraction of the third mandibular molars is the most frequent procedure in oral and maxillo-facial surgery[1].
An impacted third molar can cause different consequences such as pericoronitis, distal caries and periodontal pocket of the second molar, odontogenic abscesses, and the development of follicular cysts[2].
The healing period following the surgical extraction of an impacted third mandibular molar is associated with an intense inflammatory response. This process is responsible for postoperative pain, facial swelling, and trismus, which negatively affect the quality of life of the patients during 7–10 days after the surgery[3]. These signs and symptoms are a consequence of the surgical wound and the duration of the surgery itself[4], as the result of a direct trauma on the blood and lymphatic vessels[5]. After local anesthesia wears off, the pain usually reaches maximum intensity 3 to 5 h after surgery, continuing for 2 to 3 days, and gradually diminishing until the seventh day[6][7]. Swelling reaches peak intensity in 12 to 48 h, influencing facial esthetics and social interactions. It usually resolves between the fifth and seventh days. Trismus may be considered initially as having a protective function by encouraging the patient to rest the surgical site and permit healing. However, it may lead to difficulty in eating and functioning if it persists for more than a few days.
Piezoelectric devices, which can be used instead of conventional burs, may be beneficial for surgeries at complex anatomical sites because they can preferentially cut mineralized structure[8]; furthermore, some authors reported a reduction in postoperative sequelae using the piezoelectric surgical technique in third molar extraction[9][10].
The standard therapeutic approach to reduce the postoperative complications is the administration of medications such as non-steroidal anti-inflammatories (FANS), corticosteroids (CS), and analgesics. However, even if they are effective, these drugs present some important adverse effects such as the tendency to systemic bleeding, gastrointestinal irritation, and allergic reactions. In addition, antibiotics reduce the risk of postoperative infection and alveolitis, but the possibility of developing bacterial resistance makes their administration indicated only in selected cases[11].
These considerations justify the effort to find alternative and innovative methods for the resolution of the symptomatology that follows the surgical extraction of the impacted mandibular third molars, possibly without adverse effects. Non-medication methods used to minimize the postoperative after third molar extraction include cryotherapy, acupuncture, and photobiomodulation (PBM)[12][13][14].
PBM is the application of near-infrared (NIR) light for therapeutic purpose. The “optical window” in which the effective penetration of light into tissues is maximized is between approximately 600 and 1200 nm. Low-energy laser light produces photochemical effects whereby it penetrates the mucosa without overheating or producing other side effects[15].
In literature, the conclusions of the effectiveness of PBM after third molars surgical extractions are controversial. The current evidence on the effect of PBM on pain, swelling, and trismus after third molars surgery are summarized and reported.
2. Description of the Studies
A detailed flow chart of the selection process is shown in Figure 1.
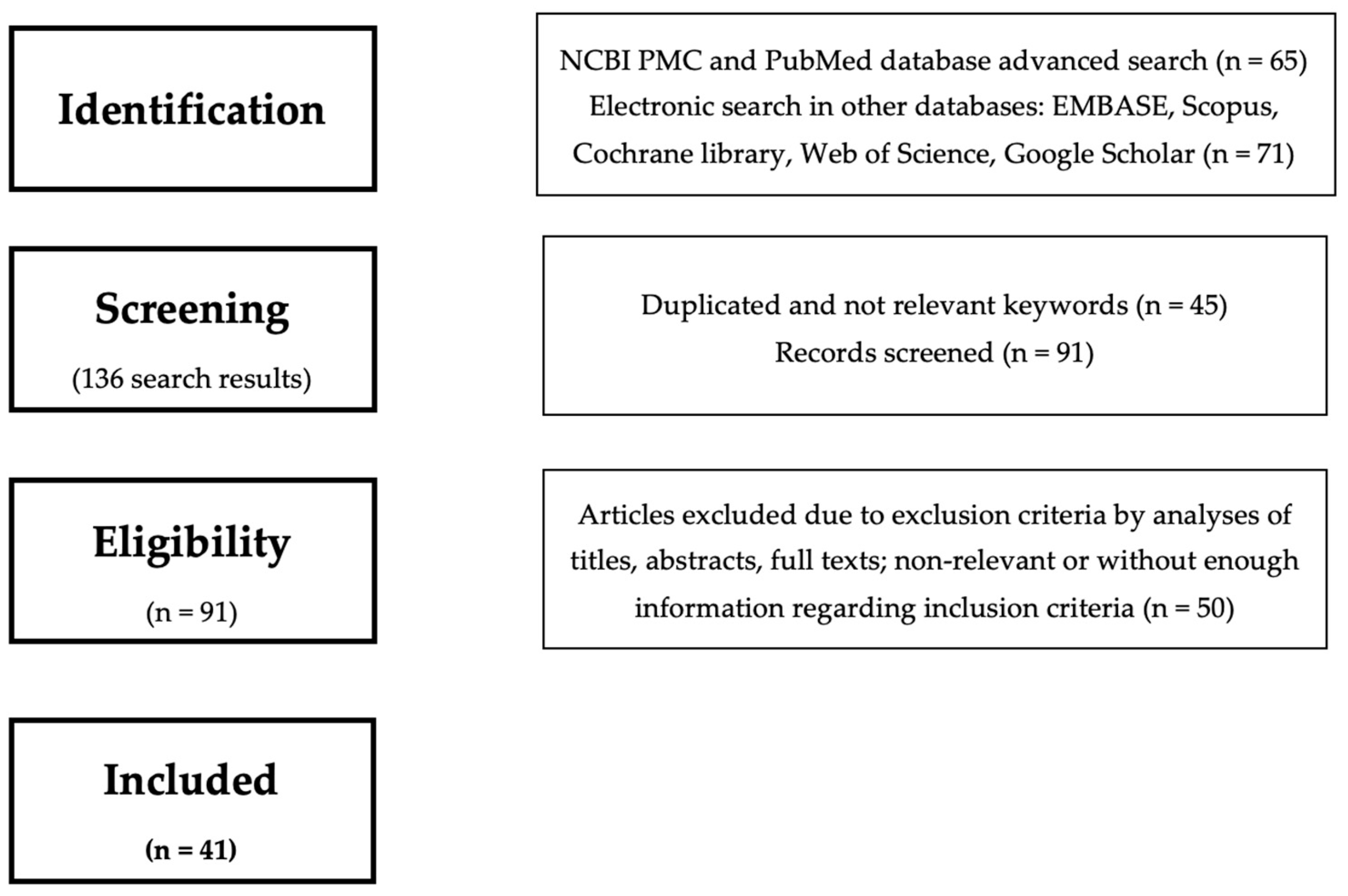
Figure 1. Flow chart illustrating the search strategy.
A total of 1833 subjects participated across the 41 studies. Nine studies did not record participants’ gender; in the other studies, there were 727 female participants and 1106 male participants.
The characteristics of the included studies are presented in Table 1 and Table 2.
Table 1. Characteristics of the included studies.
| Authors and Year of Publication | Laser Properties | Outcomes | Sample Size | |||
|---|---|---|---|---|---|---|
Table 2. Method of evaluation of the outcomes and main results of the included studies.
| Method of Evaluation | Comparison | Results | ||||
|---|---|---|---|---|---|---|
| (nm) | (mW) | (J/cm | 2) | |||
| Pain | Swelling | Trismus |
|---|
| Asutay et al. (2018)[16] | 810 | 300 | 4 | pain, trismus, swelling | Reduction | Not statistically significant | 45 | |||||
| Not statistically significant | Hamid et al. (2017) | |||||||||||
| [17] | [17] | 810 | 100 | 32, 86 | pain | 30 | ||||||
| VAS | vs. placebo | Reduction | Landucci et al. (2016)[18] | 780 | 10 | 7, 5 | pain, trismus, swelling | |||||
| [ | 22 | |||||||||||
| 18] | VAS, NRS | vs. placebo | Not statistically significant | Reduction | Reduction | Sierra et al. (2015) | ||||||
| [19] | [19] | 660, 808 | 100 | VAS, FDM, MO | 106 | pain | 60 | |||||
| vs. placebo | Reduction | |||||||||||
| [20 | Sierra et al. (2016)[20] | 660, 808 | ] | 100 | 106 | FDM, MO | 808 nm vs. 660 nm | 808 Reduction | pain | 60 | ||
| 808 Reduction | Pol et al. (2016)[21] | 650, 904 | 8–500, 70 | no reported | pain, swelling | 25 | ||||||
| [21] | VAS, FDM | vs. placebo | Reduction | Reduction | Abdel-Alim et al. (2015)[22] | |||||||
| [22 | 830 | ] | MO, Bello’s FSA | 4 | no reported | pain, trismus, swelling | 80 | |||||
| vs. delayed PBM | Reduction | Reduction | Reduction | Fabre et al. (2015)[23] | 660 | 35 | 5 | pain, trismus, swelling | 10 | |||
| [23] | VAS, FDM, MO | vs. placebo | Reduction | Reduction | Reduction | |||||||
| [24 | Merigo et al. (2015)[24] | 650, 910 | ] | no reported | 480, 31 | pain, swelling | 59 | |||||
| VAS, FDM | vs. placebo | Reduction | Reduction | Ferrante et al. (2013)[25] | 980 | 300 | no reported | pain, trismus, swelling | 30 | |||
| [25] | VAS, FDM, MO | vs. placebo | Reduction | Reduction | Koparal et al. (2018)[26] | 810 | 300 | 4 | pain, trismus, swelling | 45 | ||
| Reduction | ||||||||||||
| [26] | VAS, MO, 3dMD FP | vs. placebo | Reduction | Not statistically significant | Not statistically significant | Raisesian et al. (2017)[27] | 980 | 300 | 18 | pain, trismus, swelling | 44 | |
| [27 | Petrini et al. (2017)[28] | 980 | 300 | no reported | pain, trismus, swelling | 45 | ||||||
| ] | Kahraman et al. (2017)[29] | 830 | 100 | 3 | pain | 53 | ||||||
| Alan et al. (2016)[30] | 810 | 300 | 4 | pain, trismus, swelling | 15 | |||||||
| VAS, FDM, MO | Eroglu et al. (2016)[31] | 940 | no reported | 4 | pain, trismus, swelling | 35 | ||||||
| vs. drug therapy | Reduction | Not statistically significant | Not statistically significant | |||||||||
| [28] | VAS, FDM, MO | vs. drug therapy | Reduction | Reduction | Not statistically significant | |||||||
| [29] | VAS | intraoral vs. extraoral | Reduction | |||||||||
| [30] | VAS, MO, 3dMD FP | vs. placebo | Reduction | Not statistically significant | Not statistically significant | |||||||
| [31] | VAS, FDM, MO | vs. placebo | Not statistically significant | Not statistically significant | Not statistically significant | |||||||
| [32 | Eshghpour et al. (2016)[32] | 660 | ] | 200 | 85, 7 | pain, swelling | 40 | |||||
| VAS, ECE | vs. placebo | Kazancioglu et al. (2014)[33] | 808 | 100 | 4 | pain, trismus, swelling | 60 | |||||
| Reduction | Reduction | |||||||||||
| [33] | VAS, FDM, MO | vs. ozone therapy | Reduction | Reduction | Tuk et al. (2017)[34] | 660 | 198 | 67,5 | pain | 163 | ||
| Reduction | ||||||||||||
| [34] | HR, SR, Questionnaire | vs. placebo | Not statistically significant | Farhadi et al. (2017)[35] | 550 | 100 | 5 | pain, trismus, swelling | 48 | |||
| [35 | Pedreira et al. (2016)[36] | 808 | no reported | 2 | pain, trismus, swelling | 24 | ||||||
| ] | Not statistically significant | Lopez Ramirez et al. (2012)[37] | 810 | 500 | ||||||||
| [37] | VAS, FDM, MO | vs. placebo | 5 | pain, trismus, swelling | 20 | |||||||
| Not statistically significant | Not statistically significant | Not statistically significant | Amarillas et al. (2010)[38] | 810 | c100 | 4 | pain, trismus, swelling | 30 | ||||
| VAS, FDM, MO | ||||||||||||
| [38] | VAS, FDM, MO | vs. placebo | Not statistically significant | Not statistically significant | Not statistically significant | Roynesdal et al. (1993)[39] | 830 | 40 | no reported | pain, trismus, swelling | 25 | |
| [39] | VAS, FS, MO | vs. placebo | Not statistically significant | Not statistically significant | Not statistically significant | Fernando et al. (1993)[40] | 830 | 30 | no reported | pain, swelling | 52 | |
| vs. placebo | ||||||||||||
| [40] | VAS, Swelling scale | vs. placebo | Not statistically significant | Not statistically significant | ||||||||
| [41] | Markovic et al. (2007)[41] | 637 | 50 | 4 | swelling | 120 | ||||||
| Not statistically significant | FDM | vs. placebo | Reduction | 100 | 4 | swelling, trismus | 32 | |||||
| [42] | Amin Laskin FS, MO | vs. placebo | Reduction | Reduction | Aras et al. (2010)[43] | 808 | 100 | 4 | ||||
| [43] | Amin Laskin FS, MO | swelling, trismus | 48 | |||||||||
| Not statistically significant | intraoral vs. extraoral | Feslihan et al. (2019)[44] | 810 | 300 | 6 | pain, trismus, swelling | 30 | |||||
| Santos et al. (2020)[45] | 780 | 70 | 52, 5 | pain | 32 | |||||||
| Not statistically significant | ||||||||||||
| [36] | VAS, FDM, MO | vs. placebo | Not statistically significant | Not statistically significant | Aras et al. (2009)[42] | 808 | Reduction | Reduction | ||||
| [44] | VAS, FDM, MO | vs. methylprednisolone | Not statistically significant | Not statistically significant | Not statistically significant | |||||||
| [45] | VAS | vs. split mouth | Reduction | Lakshmi et al. (2021)[46] | ||||||||
| [ | 980 | 300 | no reported | 46] | pain, trismus, swelling | 100 | ||||||
| VAS, FS, MO | vs. placebo | Not statistically significant | El Saeed et al. (2020)[47] | 980 | 500 | 4 | pain, trismus, swelling | 20 | ||||
| Reduction | Reduction | |||||||||||
| [47] | VAS, FS, MO | vs. placebo | Reduction | Reduction | Reduction | Nejat et al. (2021)[48] | 660, 980 | 200 | ||||
| [48] | 1.5, 6 | pain | 80 | |||||||||
| VAS | vs. placebo | Reduction | Kamal et al. (2021)[49] | 980 | 100 | no reported | pain, trismus, swelling | |||||
| [49 | 24 | |||||||||||
| ] | VAS, FS, MO | vs placebo | Reduction | Reduction | Reduction | Bianchi de Moraes et al. (2020)[50] | 660 | 30 | 10, 30 | pain, trismus, swelling | 57 | |
| [50] | VAS, MO, 3dMD FP | 10 J/cm2 vs. 30 J/cm2 vs. placebo | Not statistically significant | Kumar Gulia et al. (2021)[51] | 940 | 500 | 10 | pain, trismus, swelling | 32 | |||
| Scarano et al. (2021)[52] | 1064 | 1000 | no reported | pain, swelling | 20 | |||||||
| Momeni et al. (2021)[53] | 940 | 500 | 10 | pain, trismus, swelling | 25 | |||||||
| Hadad et al. (2021)[54] | 810 | Fraga et al. (2020)[55] | 808 | 100 | 133 |
| [16] | VAS, MO, 3dMD FP | vs. placebo | ||||||||
| Not statistically significant | ||||||||||
| Not statistically significant | ||||||||||
| [ | ||||||||||
| 51 | ||||||||||
| ] | ||||||||||
| VAS, FS, MO | ||||||||||
| vs. placebo | ||||||||||
| Reduction | ||||||||||
| Not statistically significant | ||||||||||
| Not statistically significant | ||||||||||
| [ | ||||||||||
| 52 | ||||||||||
| ] | ||||||||||
| VAS, FS | ||||||||||
| vs. placebo | ||||||||||
| Reduction | ||||||||||
| Reduction | ||||||||||
| [ | ||||||||||
| 53] | VAS, FS, MO | vs. placebo | Reduction | Not statistically significant | Not statistically significant | |||||
| 100 | 212 | pain, trismus, swelling | 13 | |||||||
| [54] | VAS, FS, MO | vs. placebo | Reduction | Reduction | Not statistically significant | |||||
| [ | pain, swelling | 55] | 40 | |||||||
| VAS, FS | LLLT + aPDT vs. placebo | Reduction | Not statistically significant | Mohajerani et al. (2020)[56] | 810, 632 | 500 | 5, 2 | pain, trismus, swelling | 40 |
| [ |
| 56 |
| ] |
| VAS, FS, MO |
| vs. split mouth |
| Reduction |
| Reduction |
| Not statistically significant |
Legend: aPDT, antimicrobial photodynamic therapy, FDM, facial distance measuring, FS, facial swelling, MO, maximum mouth opening, NRS, numeric rating scale, PRS, pain rating scale, VAS, visual analog scale, 3dMD FP, 3dMD face photogrammetric.
3. Efficacy of PBM
3.1. Pain
Twenty-five studies reported a reduction of pain when compared to placebo[16][17][19][21][22][23][24][25][26][27][28][29][30][32][33][45][46][47][51][52][53][54][55][56]. In these studies, lasers were used both intraorally and extraorally, and the laser’s parameters were as follows: wavelengths ranged from 632 to 1064 nm; powers were between 4 and 1000 mW; energy densities were between 3 and 212 J/cm2. Eleven articles reported no statistically significant difference of PBM on reducing pain in comparison with placebo[18][31][34][35][36][37][38][39][40]. The lasers used in these studies were diode lasers with wavelengths of 660 nm, 810 nm, and 980 nm, different powers (30–500 mW) and energy densities (2–60 J/cm2). The most successful wavelengths in reducing pain were 810 and 980 nm (Figure 2).
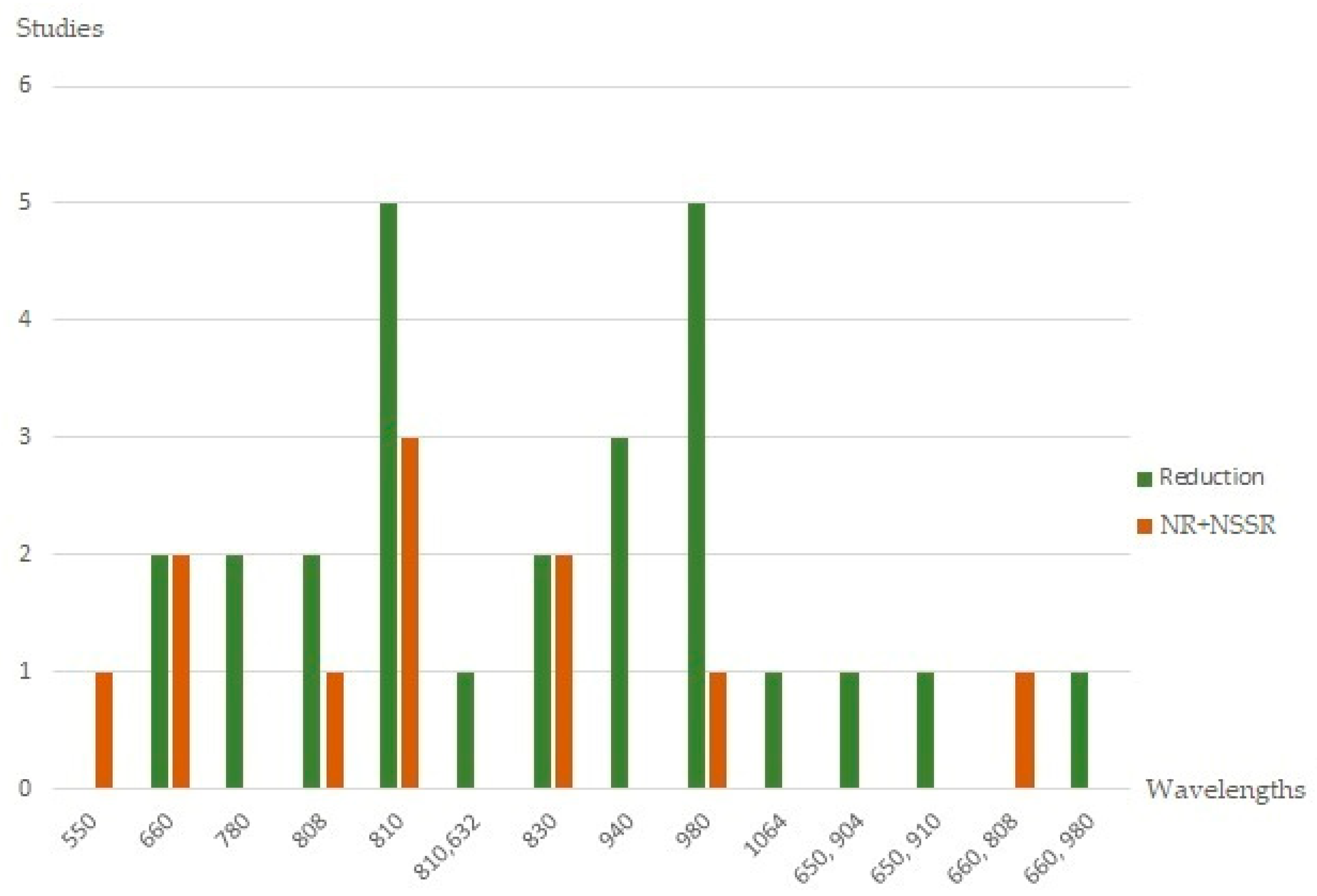
Figure 2. Histograms showing the pain outcome according to the wavelengths of the included studies. Legend: NR, no reduction, NSSR, no statistically significant results.
3.2. Facial Swelling
Facial swelling was assessed in 36 studies[16][18][21][22][23][24][25][26][27][28][35][36][37][38][39][40][41][42][44][46][49][50][51][52][53][54][55][56]. Nineteen articles reported significant decrease in facial swelling after PBM application when compared with placebo[18][20][21][22][23][24][25][32][33][41][42][43][46][47][49][52][54][56]. The laser’s parameters of the included articles were as follows: wavelengths ranged from 650 to 1064 nm; powers were between 4 and 1000 mW; energy densities were between 2 and 480 J/cm2. The wavelength of 810 nm induced the smallest facial swelling reduction (Figure 3).
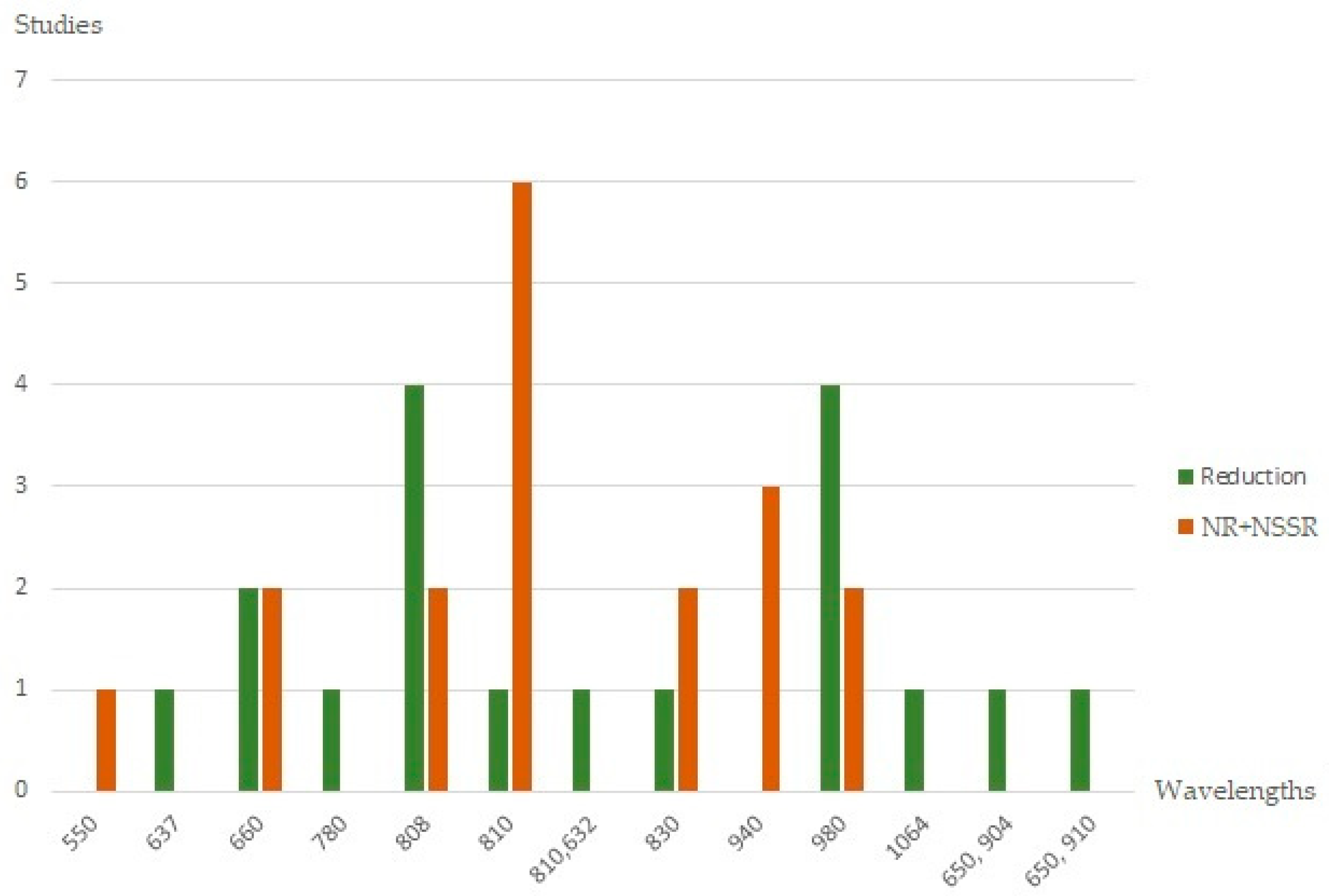
Figure 3. Histograms showing the swelling outcome according to the wavelengths of the included studies. Legend: NR, no reduction, NSSR, no statistically significant results.
3.3. Trismus
Twenty-eight studies assessed the impact of PBM on postoperative trismus. Eleven studies reported reducing of trismus with PBM[19][20][22][23][25][33][42][43][46][47][49]. In the included studies, wavelengths ranged between 660 and 980 nm, power ranged between 4 and 500 mW, and energy densities were between 4 and 212 J/cm2. As for swelling, the wavelength of 810 nm was the one that induced the worst outcome. Instead, the wavelength of 980 nm determined the better reduction of trismus (Figure 4).
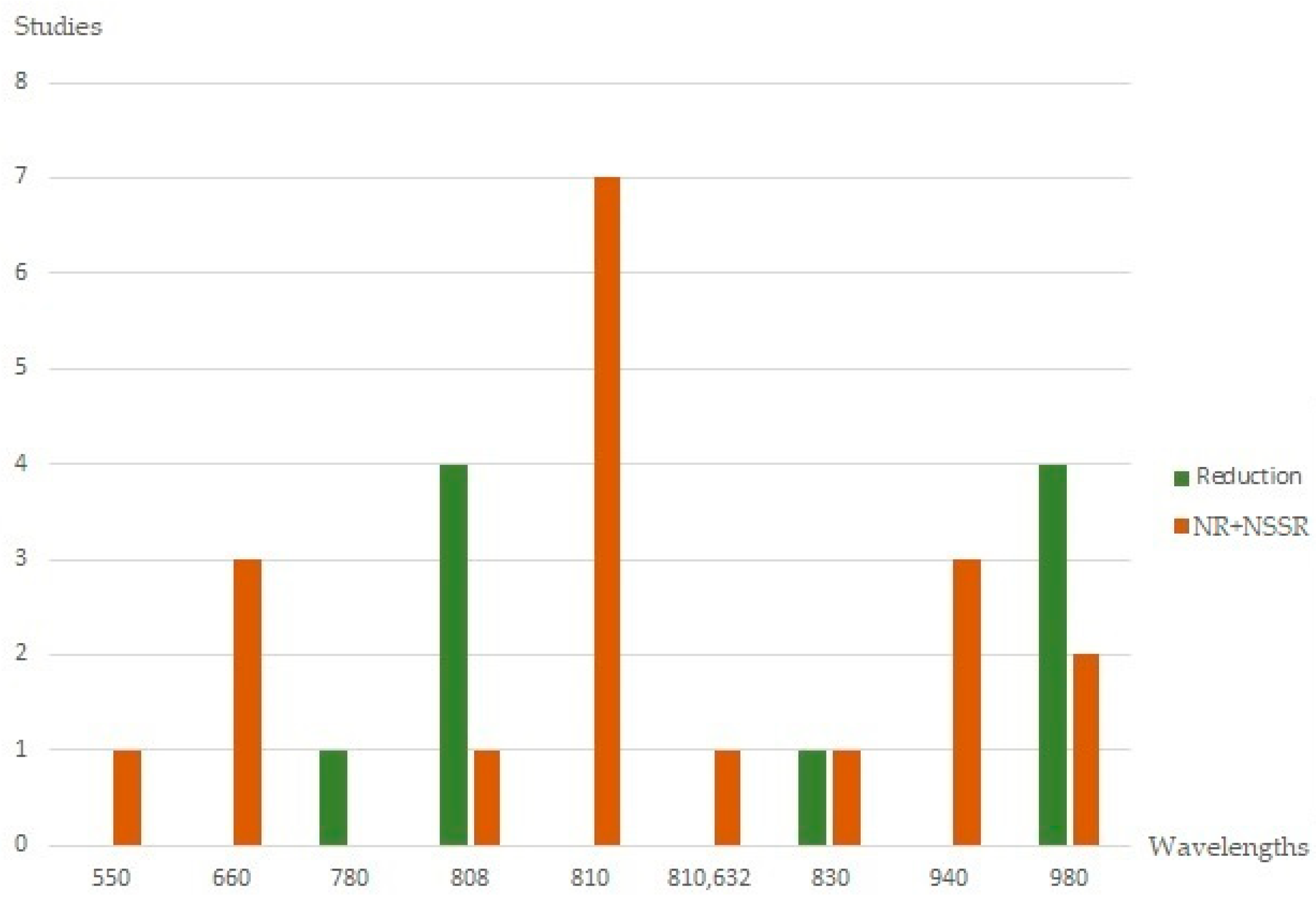
Figure 4. Histograms showing the trismus outcome according to the wavelengths of the included studies. Legend: NR, no reduction, NSSR, no statistically significant results.
References
- Matteo Chiapasco; Lorenzo De Cicco; Guido Marrone; Side effects and complications associated with third molar surgery. Oral Surgery, Oral Medicine, Oral Pathology 1993, 76, 412-420, 10.1016/0030-4220(93)90005-o.
- Vijay Apparaju; Nikhil Srivastava; Akshay Shetty; Rahul Dev Goswami; Vivek Bagga; Saurabh Kale; Incidence of distal caries in mandibular second molars due to impacted third molars: Nonintervention strategy of asymptomatic third molars causes harm? A retrospective study. International Journal of Applied and Basic Medical Research 2017, 7, 15-19, 10.4103/2229-516x.198505.
- Virendra Singh; Ashish Garg; Amrish Bhagol; S. Savarna; Santosh Kumar Agarwal; Photobiomodulation Alleviates Postoperative Discomfort After Mandibular Third Molar Surgery. Journal of Oral and Maxillofacial Surgery 2019, 77, 2412-2421, 10.1016/j.joms.2019.06.009.
- Kyösti Oikarinen; Postoperative pain after mandibular third-molar surgery. Acta Odontologica Scandinavica 1991, 49, 7-13, 10.3109/00016359109041135.
- A.N. Beech; S. Haworth; G.J. Knepil; Measurement of generic compared with disease-specific quality of life after removal of mandibular third molars: a patient-centred evaluation. British Journal of Oral and Maxillofacial Surgery 2017, 55, 274-280, 10.1016/j.bjoms.2017.01.005.
- Lucía Lago-Méndez; Márcio Diniz-Freitas; Carmen Senra; Francisco Gude-Sampedro; José Manuel Gándara Rey; Abel Garcia-Garcia; Relationships Between Surgical Difficulty and Postoperative Pain in Lower Third Molar Extractions. Journal of Oral and Maxillofacial Surgery 2007, 65, 979-983, 10.1016/j.joms.2006.06.281.
- W. L. He; F. Y. Yu; C. J. Li; J. Pan; R. Zhuang; P. J. Duan; A systematic review and meta-analysis on the efficacy of low-level laser therapy in the management of complication after mandibular third molar surgery. Lasers in Medical Science 2014, 30, 1779-1788, 10.1007/s10103-014-1634-0.
- Roberto Lo Giudice; Francesco Puleio; David Rizzo; Angela Alibrandi; Giorgio Lo Giudice; Antonio Centofanti; Luca Fiorillo; Debora Di Mauro; Fabiana Nicita; Comparative Investigation of Cutting Devices on Bone Blocks: An SEM Morphological Analysis. Applied Sciences 2019, 9, 351, 10.3390/app9020351.
- E.A. Al-Moraissi; Y.A. Elmansi; Y.A. Al-Sharaee; A.E. Alrmali; A.S. Alkhutari; Does the piezoelectric surgical technique produce fewer postoperative sequelae after lower third molar surgery than conventional rotary instruments? A systematic review and meta analysis. International Journal of Oral and Maxillofacial Surgery 2015, 45, 383-391, 10.1016/j.ijom.2015.10.005.
- Francesco Sortino; Eugenio Pedullà; Veronica Masoli; The Piezoelectric and Rotatory Osteotomy Technique in Impacted Third Molar Surgery: Comparison of Postoperative Recovery. Journal of Oral and Maxillofacial Surgery 2008, 66, 2444-2448, 10.1016/j.joms.2008.06.004.
- Giovanni Lodi; Lara Figini; Andrea Sardella; Antonio Carrassi; Massimo Del Fabbro; Susan Furness; Antibiotics to prevent complications following tooth extractions. Cochrane Database of Systematic Reviews 2012, 11, CD003811, 10.1002/14651858.cd003811.pub2.
- do Nascimento-Júnior EM, Dos Santos GMS, Tavares Mendes ML, Cenci M, Correa MB, Pereira-Cenci T, Martins-Filho PRS.; Cryotherapy in reducing pain, trismus, and facial swelling after third-molar surgery: Systematic review and meta-analysis of randomized clinical trials. . J Am Dent Assoc 2019, 150 (4), 269-277, 10.1016/j.adaj.2018.11.008..
- A.C.V. Armond; J.C.R. Glória; C.R.R. dos Santos; R. Galo; S.G.M. Falci; Acupuncture on anxiety and inflammatory events following surgery of mandibular third molars: a split-mouth, randomized, triple-blind clinical trial. International Journal of Oral and Maxillofacial Surgery 2019, 48, 274-281, 10.1016/j.ijom.2018.07.016.
- Cp. Isolan; Mateus De Azevedo Kinalski; Oa. Leão; Lk. Post; Tm. Isolan; Mb. dos Santos; Photobiomodulation therapy reduces postoperative pain after third molar extractions: A randomized clinical trial. Medicina Oral Patología Oral y Cirugia Bucal 2021, 26, e341-e348, 10.4317/medoral.24228.
- Alessandro Del Vecchio; Gianluca Tenore; Maria Clotilde Luzi; Gaspare Palaia; Ahmed Mohsen; Daniele Pergolini; Umberto Romeo; Laser Photobiomodulation (PBM)-A Possible New Frontier for the Treatment of Oral Cancer: A Review of In Vitro and In Vivo Studies.. Healthcare (Basel) 2021, 9 (2), 134, 10.3390/healthcare9020134..
- F Asutay; Ayse Ozcan Kucuk; H Alan; M Koparal; Three-dimensional evaluation of the effect of low-level laser therapy on facial swelling after lower third molar surgery: A randomized, placebo-controlled study. Nigerian Journal of Clinical Practice 2018, 21, 1107-1113.
- May Ayad Hamid; Low-level laser therapy on postoperative pain after mandibular third molar surgery. Annals of Maxillofacial Surgery 2017, 7, 207-216, 10.4103/ams.ams_5_17.
- A. Landucci; A.C. Wosny; L.C. Uetanabaro; Alexandre Moro; M.R. Araujo; Efficacy of a single dose of low-level laser therapy in reducing pain, swelling, and trismus following third molar extraction surgery. International Journal of Oral and Maxillofacial Surgery 2016, 45, 392-398, 10.1016/j.ijom.2015.10.023.
- Simone Oliveira Sierra; Alessandro Melo Deana; Sandra Kalil Bussadori; Ana Carolina Costa da Mota; Lara Jansiski Motta; Raquel Agnelli Mesquita Ferrari; Tatiana Dias Schalch; Kristianne Porta Santos Fernandes; Effect of low-intensity laser treatment on pain after extraction of impacted mandibular third molars: a randomised, controlled, clinical trial. British Journal of Oral and Maxillofacial Surgery 2015, 53, 996-1000, 10.1016/j.bjoms.2015.09.006.
- Simone Oliveira Sierra; Alessandro Melo Deana; Sandra Kalil Bussadori; Ana Carolina Costa da Mota; Raquel Agnelli Mesquita Ferrari; Katia Llanos Do Vale; Kristianne Porta Santos Fernandes; Choosing between intraoral or extraoral, red or infrared laser irradiation after impacted third molar extraction. Lasers in Surgery and Medicine 2016, 48, 511-518, 10.1002/lsm.22488.
- Renato Pol; Tiziana Ruggiero; Giorgia Gallesio; Massimo Riso; Laura Bergamasco; Carmen Mortellaro; Marco Mozzati; Efficacy of Anti-Inflammatory and Analgesic of Superpulsed Low Level Laser Therapy After Impacted Mandibular Third Molars Extractions. Journal of Craniofacial Surgery 2016, 27, 685-690, 10.1097/scs.0000000000002523.
- Hala M. Abdel-Alim; Hassan Abdel-Dayem; Zeinab A. Mustafa; Amr Bayoumi; Ahmed Jan; Fatima Jadu; A Comparative Study of the Effectiveness of Immediate Versus Delayed Photobiomodulation Therapy in Reducing the Severity of Postoperative Inflammatory Complications. Photomedicine and Laser Surgery 2015, 33, 447-451, 10.1089/pho.2015.3923.
- Hebert S. C. Fabre; Ricardo L. Navarro; Paula V.P. Oltramari-Navarro; Rodrigo F. Oliveira; Deise A. A. Pires-Oliveira; Rodrigo A. C. Andraus; Nelson Fuirini; Karen B. P. Fernandes; Anti-inflammatory and analgesic effects of low-level laser therapy on the postoperative healing process. Journal of Physical Therapy Science 2015, 27, 1645-1648, 10.1589/jpts.27.1645.
- Elisabetta Merigo; Paolo Vescovi; Meirav Margalit; Enrico Ricotti; Stefano Stea; Marco Meleti; Maddalena Manfredi; Carlo Fornaini; Efficacy of LLLT in swelling and pain control after the extraction of lower impacted third molars.. LASER THERAPY 2015, 24, 39-46, 10.5978/islsm.15-OR-05.
- Maurizio Ferrante; Morena Petrini; Paolo Trentini; Giorgio Perfetti; Giuseppe Spoto; Effect of low-level laser therapy after extraction of impacted lower third molars. Lasers in Medical Science 2012, 28, 845-849, 10.1007/s10103-012-1174-4.
- Mahmut Koparal; Ayse Ozcan Kucuk; Hilal Alan; Fatih Asutay; Mehmet Avci; Effects of low-level laser therapy following surgical extraction of the lower third molar with objective measurement of swelling using a three-dimensional system. Experimental and Therapeutic Medicine 2018, 15, 3820-3826, 10.3892/etm.2018.5921.
- Shahrokh Raiesian; Mehdi Khani; Kazem Savojbolaghchi Khiabani; Ershad Hemmati; Mohammad Pouretezad; Assessment of Low-Level Laser Therapy Effects After Extraction of Impacted Lower Third Molar Surgery. Journal of Lasers in Medical Sciences 2017, 8, 42-45, 10.15171/jlms.2017.08.
- Morena Petrini; M Ferrante; P Trentini; G Perfetti; G Spoto; Effect of pre-operatory low-level laser therapy on pain, swelling, and trismus associated with third-molar surgery. Medicina Oral Patología Oral y Cirugia Bucal 2017, 22, e467-e472, 10.4317/medoral.21398.
- Sevil Altundag Kahraman; Sedat Cetiner; Robert A. Strauss; The Effects of Transcutaneous and Intraoral Low-Level Laser Therapy After Extraction of Lower Third Molars: A Randomized Single Blind, Placebo Controlled Dual-Center Study. Photomedicine and Laser Surgery 2017, 35, 401-407, 10.1089/pho.2016.4252.
- Alan H, Yolcu Ü, Koparal M, Özgür C, Öztürk SA, Malkoç S.; Evaluation of the effects of the low-level laser therapy on swelling, pain, and trismus after removal of impacted lower third molar. Head Face Med 2016, 12, 25, 10.1186/s13005-016-0121-1.
- Cennet Neslihan Eroglu; Serap Keskin Tunc; Effectiveness of Single Session of Low-Level Laser Therapy with a 940 nm Wavelength Diode Laser on Pain, Swelling, and Trismus After Impacted Third Molar Surgery. Photomedicine and Laser Surgery 2016, 34, 406-410, 10.1089/pho.2016.4101.
- Majid Eshghpour; Farzaneh Ahrari; Mohammad Takallu; Is Low-Level Laser Therapy Effective in the Management of Pain and Swelling After Mandibular Third Molar Surgery?. Journal of Oral and Maxillofacial Surgery 2016, 74, 1322.e1-1322.e8, 10.1016/j.joms.2016.02.030.
- Hakki Oguz Kazancioglu; Seref Ezirganli; Nihat Demirtas; Comparison of the influence of ozone and laser therapies on pain, swelling, and trismus following impacted third-molar surgery. Lasers in Medical Science 2013, 29, 1313-1319, 10.1007/s10103-013-1300-y.
- Jacco G.C. Tuk; Arjen J. van Wijk; Ine C. Mertens; Zühal Keleş; Jérôme A.H. Lindeboom; Dan M.J. Milstein; Analgesic effects of preinjection low-level laser/light therapy (LLLT) before third molar surgery: a double-blind randomized controlled trial. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology 2017, 124, 240-247, 10.1016/j.oooo.2017.04.017.
- Farrokh Farhadi; Hosein Eslami; Alireza Majidi; Vahid Fakhrzadeh; Milad Ghanizadeh; Sahar KhademNeghad; Evaluation of adjunctive effect of low-level laser Therapy on pain, swelling and trismus after surgical removal of impacted lower third molar: A double blind randomized clinical trial. LASER THERAPY 2017, 26, 181-187, 10.5978/islsm.17-or-13.
- Amanda A Pedreira; Flavia G Wanderley; Maira F Sa; Camila S Viena; Adriano Perez; Ryuichi Hoshi; Marcia P Leite; Silvia R A Reis; Alena P Medrado; Thermographic and clinical evaluation of 808-nm laser photobiomodulation effects after third molar extraction.. Minerva stomatologica 2016, 65, 213-222, PMID: 27374361.
- López-Ramírez M, Vílchez-Pérez MA, Gargallo-Albiol J, Arnabat-Domínguez J, Gay-Escoda C.; Efficacy of low-level laser therapy in the management of pain, facial swelling, and postoperative trismus after a lower third molar extraction. A preliminary study. Lasers Med Sci 2012, 27(3), 559-566, doi: 10.1007/s10103-011-0936-8.
- E. Darío Amarillas-Escobar; J. Martin Toranzo-Fernández; Ricardo Martínez-Rider; Miguel A. Noyola-Frías; J. Antonio Hidalgo-Hurtado; Víctor M. Fierro Serna; Antonio Gordillo-Moscoso; Amaury Pozos-Guillen; Use of Therapeutic Laser After Surgical Removal of Impacted Lower Third Molars. Journal of Oral and Maxillofacial Surgery 2010, 68, 319-324, 10.1016/j.joms.2009.07.037.
- A.K. Roynesdal; T. Björnland; P. Barkvoll; H.R. Haanaes; The effect of soft-laser application on postoperative pain and swelling: A double-blind, crossover study. International Journal of Oral and Maxillofacial Surgery 1993, 22, 242-245, 10.1016/s0901-5027(05)80646-0.
- S. Fernando; C.M. Hill; R. Walker; A randomised double blind comparative study of low level laser therapy following surgical extraction of lower third molar teeth. British Journal of Oral and Maxillofacial Surgery 1993, 31, 170-172, 10.1016/0266-4356(93)90118-g.
- Aleksa Markovic; Lj. Todorovic; Effectiveness of dexamethasone and low-power laser in minimizing oedema after third molar surgery: a clinical trial. International Journal of Oral and Maxillofacial Surgery 2007, 36, 226-229, 10.1016/j.ijom.2006.10.006.
- Mutan Hamdi Aras; Metin Güngörmüş; The Effect of Low-Level Laser Therapy on Trismus and Facial Swelling Following Surgical Extraction of a Lower Third Molar. Photomedicine and Laser Surgery 2009, 27, 21-24, 10.1089/pho.2008.2258.
- Mutan Hamdi Aras; Metin Güngörmüş; Placebo-controlled randomized clinical trial of the effect two different low-level laser therapies (LLLT)—intraoral and extraoral—on trismus and facial swelling following surgical extraction of the lower third molar. Lasers in Medical Science 2009, 25, 641-645, 10.1007/s10103-009-0684-1.
- Erkan Feslihan; Cennet Neslihan Eroğlu; Can Photobiomodulation Therapy Be an Alternative to Methylprednisolone in Reducing Pain, Swelling, and Trismus After Removal of Impacted Third Molars?. Photobiomodulation, Photomedicine, and Laser Surgery 2019, 37, 700-705, 10.1089/photob.2019.4696.
- Pâmela Letícia Santos; Ana Paula Marotto; Thaiz Zatta da Silva; Mariele Pecorali Bottura; Mayra Valencise; Daniela Oliveira Marques; Thallita Pereira Queiroz; Is Low-Level Laser Therapy Effective for Pain Control After the Surgical Removal of Unerupted Third Molars? A Randomized Trial. Journal of Oral and Maxillofacial Surgery 2019, 78, 184-189, 10.1016/j.joms.2019.08.029.
- Lakshmi, K.P.; Ali Baig, S.; Walia, S.; Priyadharshini, V.; Vigneswaran, T.; Mazgaonkar, F.S.; Tiwari, R.V.C; Evaluation of effect of low level laser therapy post third molar surgery: An original research. Turk. J. Physiother. Rehabil. 2016, 32, 15240–15243, -.
- El Saeed, A.M.; Al-Fakharany, A.H.; Effect of Single Dose Low-Level Laser Therapy on Some Sequalae After Impacted Lower Third Molar Surgery. Al-Azhar Journal of Dental Science 2020, 23, 41-47, 10.21608/ajdsm.2020.108462.
- Amir Hossein Nejat; Majid Eshghpour; Nasrin Danaeifar; Majid Abrishami; Farshid Vahdatinia; Reza Fekrazad; Effect of Photobiomodulation on the Incidence of Alveolar Osteitis and Postoperative Pain following Mandibular Third Molar Surgery: A Double‐Blind Randomized Clinical Trial. Photochemistry and Photobiology 2021, 97, 1129-1135, 10.1111/php.13457.
- Mina Kamal Girgis; Eman Elsharrawy; Mohamed Hassan; Effect of Single Session of Low-Level Laser Therapy on Pain, Swelling, and Trismus after Surgical Extraction of Impacted Lower Third Molar : A Clinical Study. Dental Science Updates 2021, 2, 55-60, 10.21608/dsu.2021.25822.1030.
- Michelle Bianchi De Moraes; Rúbia Gomes De Oliveira; Fernando Vagner Raldi; Rodrigo Dias Nascimento; Mauro Pedrine Santamaria; Fábio Ricardo Loureiro Sato; Does the Low-Intensity Laser Protocol Affect Tissue Healing After Third Molar Removal?. Journal of Oral and Maxillofacial Surgery 2020, 78, 1920.e1-1920.e9, 10.1016/j.joms.2020.05.018.
- Gulia, S.K.; Kumar, a.; Singh, M.; Thakker, R.; Goya, P.; Tiwari, H.; Tiwari, R.V.C; Effectiveness of Low-Level Lasers Subsequent to Third Molar Surgery: An Original Research. . Ann. Rom. Soc. Cell Biol. 2021, 25, 2048–2053., -.
- Antonio Scarano; Felice Lorusso; Francesca Postiglione; Filiberto Mastrangelo; Morena Petrini; Photobiomodulation Enhances the Healing of Postextraction Alveolar Sockets: A Randomized Clinical Trial With Histomorphometric Analysis and Immunohistochemistry. Journal of Oral and Maxillofacial Surgery 2020, 79, 57.e1-57.e12, 10.1016/j.joms.2020.09.008.
- Ehsan Momeni; Hoda Barati; Melika Rajaei Arbabi; Behrouz Jalali; Mahdieh-Sadat Moosavi; Low‐level laser therapy using laser diode 940 nm in the mandibular impacted third molar surgery: double-blind randomized clinical trial. BMC Oral Health 2021, 21, 1-8, 10.1186/s12903-021-01434-1.
- Henrique Hadad; Ana Flávia Piquera Santos; Laís Kawamata de Jesus; Pier Paolo Poli; Ronaldo Célio Mariano; Leticia Helena Theodoro; Carlo Maiorana; Francisley Ávila Souza; Photobiomodulation Therapy Improves Postoperative Pain and Edema in Third Molar Surgeries: A Randomized, Comparative, Double-Blind, and Prospective Clinical Trial. Journal of Oral and Maxillofacial Surgery 2021, 80, 37.e1-37.e12, 10.1016/j.joms.2021.08.267.
- Renato Silva Fraga; Lívia Azeredo Alves Antunes; Walter Luis Soares Fialho; Maria Isabel Valente; Cinthya Cristina Gomes; Karla Bianca Fernandes Costa Fontes; Leonardo Santos Antunes; Do Antimicrobial Photodynamic Therapy and Low-Level Laser Therapy Minimize Postoperative Pain and Edema After Molar Extraction?. Journal of Oral and Maxillofacial Surgery 2020, 78, 2155.e1-2155.e10, 10.1016/j.joms.2020.08.002.
- Hassan Mohajerani; Faraj Tabeie; Arash Alirezaei; Ghazaleh Keyvani; Mehdi Bemanali; Does Combined Low-Level Laser and Light-Emitting Diode Light Irradiation Reduce Pain, Swelling, and Trismus After Surgical Extraction of Mandibular Third Molars? A Randomized Double-Blinded Crossover Study. Journal of Oral and Maxillofacial Surgery 2020, 79, 1621-1628, 10.1016/j.joms.2020.07.017.
More
