Sarcopenia, characterized by an aging-related progressive decline of skeletal muscle mass, strength, and physical performance, is frequently encountered in patients undergoing peritoneal dialysis (PD) and is associated with adverse clinical outcomes. However, the best screening tools facilitating the rapid detection of sarcopenia among patients undergoing PD remain unknown.
- SARC-F
- SARC-CalF
- calf circumference
- sarcopenia
- peritoneal dialysis
1. Introduction
2. Sarcopenia Screening among Patients Undergoing Peritoneal Dialysis
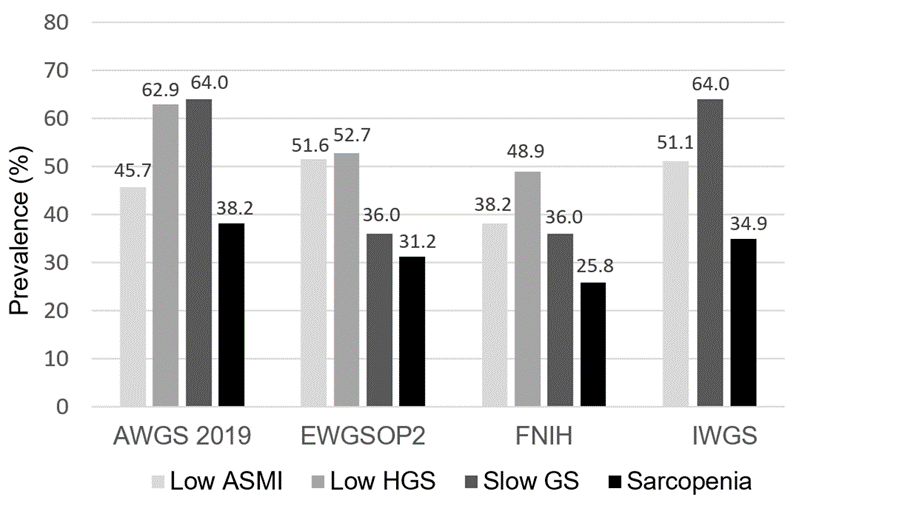
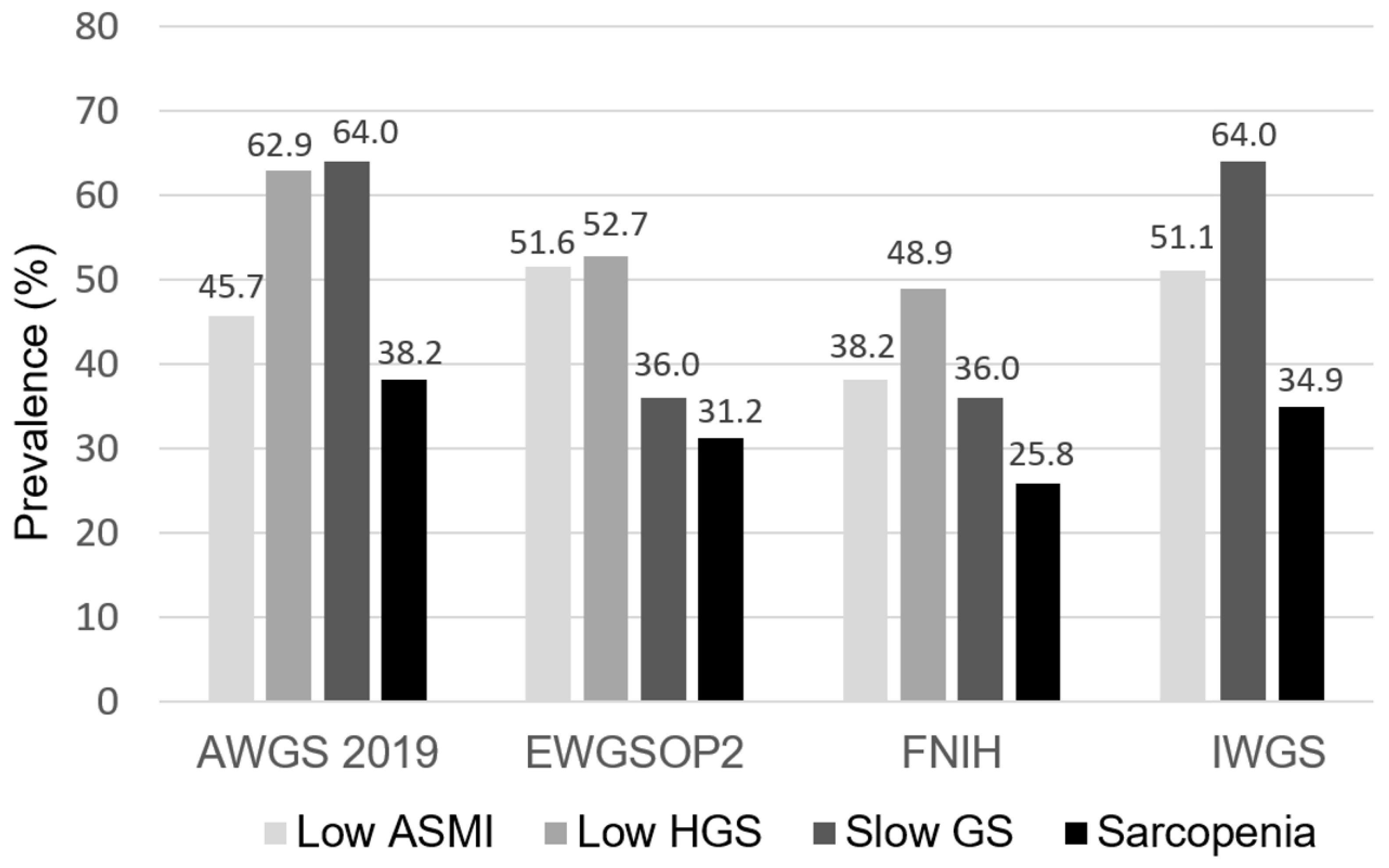
The prevalence of low ASMI, low HGS, slow GS, and sarcopenia across four sarcopenia criteria among patients undergoing PD. ASMI, appendicular skeletal muscle index; HGS, handgrip strength; GS, gait speed; AWGS, Asian Working Group for Sarcopenia; EWGSOP, European Working Group on Sarcopenia in Older People; FNIH, Foundation for the National Institutes of Health; IWGS, International Working Group on Sarcopenia.
The correlations of SARC-F, SARC-CalF, and CC with anthropometric and skeletal muscle measurements are shown in Table 1. SARC-F correlated significantly with HGS (r = −0.363, p < 0.001) and GS (r = −0.452, p < 0.001) but not with ASMI (r = −0.125, p = 0.090) and anthropometric measurements. In contrast, SARC-CalF and CC correlated not only with HGS (r = −0.445, p < 0.001 for SARC-CalF; r = 0.522, p < 0.001 for CC) and GS (r = −0.293, p < 0.001 for SARC-CalF; r = 0.181, p = 0.019 for CC) but also with ASMI (r = −0.421, p < 0.001 for SARC-CalF; r = 0.683, p < 0.001 for CC).Table 1.
The correlations of SARC-F, SARC-CalF, and CC with anthropometric and skeletal muscle measurements.
|
Variables |
SARC-F |
|
SARC-CalF |
|
CC |
|||
|
r |
||||||||
p |
||||||||
| ||||||||
| ||||||||
| ||||||||
r | p |
|
r |
p |
||||
|
Anthropometric measures |
|
|
||||||
|
CC | ||||||||
| ||||||||
|
| |||||||
0.813 (0.749–0.866)a,b | ||||||||
|
|
| ||||||
<0.001* |
||||||||
|
Weight (kg) |
−0.029 |
0.692 |
|
−0.435 |
<0.001* |
|
0.721 |
<0.001* |
|
BMI (kg/m2) |
−0.009 |
0.900 |
|
−0.382 |
<0.001* |
|
0.625 |
<0.001* |
|
WC (cm) |
||||||||
|
SARC-CalF |
0.739 (0.670–0.801)a,c |
|||||||
0.120 |
0.104 |
|
−0.224 |
0.002* |
|
0.436 |
<0.001* |
|
|
MAMC (cm) |
−0.056 |
0.451 |
|
−0.395 |
<0.001* |
|
0.617 |
<0.001* |
|
FTI (kg/m2) |
0.136 |
0.067 |
|
−0.146 |
0.050* |
|
0.298 |
<0.001* |
<0.001* | ||||||||
|
SARC-F |
0.587 (0.513–0.659)b,c |
0.033* |
||||||
|
EWGSOP2 |
|
|
||||||
|
CC |
0.776 (0.709–0.834)b |
<0.001* |
||||||
|
SARC-CalF |
0.748 (0.679–0.809)c |
<0.001* |
||||||
|
Skeletal muscle measures |
|
|||||||
|
SARC-F |
0.625 (0.551–0.695)b,c | |||||||
|
|
|||||||
0.003* | ||||||||
|
|
|
|
|
||||
|
ASMI (kg/m2) |
−0.125 |
0.090 |
|
−0.421 |
||||
|
FNIH |
|
| ||||||
<0.001* |
| 0.683 |
<0.001* |
|||||
|
HGS (kg) |
−0.363 |
|||||||
|
CC | ||||||||
<0.001* | ||||||||
| ||||||||
0.652 (0.579–0.721) |
<0.001* | |||||||
−0.445 | <0.001* |
|
0.522 |
<0.001* |
||||
|
GS (m/s)a |
−0.452 |
|||||||
|
SARC-CalF | ||||||||
<0.001* | ||||||||
|
0.648 (0.575–0.717) | ||||||||
| −0.293 |
<0.001* |
|
0.181 |
0.019* |
|||
Table 2. The diagnostic performance of SARC-F, SARC-CalF, and CC on sarcopenia based on four operational definitions in the overall study population.
|
Definitions |
AUC (95% CI) |
p |
|
AWGS 2019 | ||
0.002* | ||
SARC-F | ||
0.587 (0.513–0.659) |
0.063 |
|
|
IWGS |
|
|
|
CC |
0.750 (0.682–0.811)b |
<0.001* |
|
SARC-CalF |
0.710 (0.639–0.774)c |
<0.001* |
|
SARC-F |
0.621 (0.547–0.691)b,c |
0.004* |
AUC, area under curve; CI, confidence interval; AWGS, Asian Working Group for Sarcopenia; CC, calf circumference; EWGSOP, European Working Group on Sarcopenia in Older People; FNIH, Foundation for the National Institutes of Health; IWGS, International Working Group on Sarcopenia. a p < 0.05 indicates significant difference of AUCs between CC and SARC-CalF. b p < 0.05 indicates significant difference of AUCs between CC and SARC-F. c p < 0.05 indicates significant difference of AUCs between SARC-CalF and SARC-F. *The AUC was significantly different from 0.5.
In patients undergoing HD, Yamamoto et al. have reported that the AUCs of the SARC-F questionnaire for muscle weakness and poor physical performance range from 0.76 to 0.87, indicating its good diagnostic performance for identifying patients undergoing HD with physical disability [19]. Furthermore, a close relationship between SARC-F scores and overall mortality in patients undergoing HD has been demonstrated in our previous study [20]. Unfortunately, the AUCs of SARC-F for sarcopenia, defined as both low muscle mass and strength, were less satisfactory in geriatric and dialysis populations [20][21]. Similarly, in our PD cohort, the diagnostic performance of SARC-F on sarcopenia was generally poor across the four different criteria. In patients undergoing HD, Marini et al. have reported that SARC-F is more closely associated with muscle functionality than muscle mass [22]; similarly, we disclosed a poor correlation of SARC-F with skeletal muscle mass, including MAMC and ASMI, in patients undergoing PD. These findings suggest that the score of SARC-F primarily reflected the status of skeletal muscle strength and physical performance rather than muscle mass, the latter of which is considered as an essential criterion for sarcopenia diagnosis. In contrast, CC yielded the highest correlation with ASMI in our analysis. In this regard, SARC-CalF, which adds the CC item into SARC-F, could improve the weakness of SARC-F in the aspect of skeletal muscle mass assessment. Not surprisingly, the improved performance of SARC-CalF over SARC-F exhibited in our PD cohort had been consistently reported in the geriatric and cancer population [12][13][14][15]. In particular, CC is considered a strong and reliable marker for skeletal muscle mass in the general population, which exhibited a high correlation with appendicular lean mass in a large-scale NHANES 1999–2006 cohort [23]. The good diagnostic performance of CC for detecting sarcopenia was affirmed in middle-aged and older adults [9][10][11][24] and in patients with chronic liver disease [25] and stroke [26]. In our patients undergoing PD, CC yielded the best correlation not only with ASMI but also with HGS among the three screening tools. The discriminative power of CC was even significantly better than that of SARC-CalF when we adopted the AWGS 2019—the criteria that may be most suitable for our Taiwanese population over the other three definitions. These findings emphasize that CC could be a simple-to-measure and valuable tool for the initial screening of sarcopenia among patients undergoing PD.3. Implications for Clinical Practice
Among the widely used screening tools for sarcopenia, CC and SARC-CalF outperformed SARC-F in the diagnostic accuracy of sarcopenia among patients undergoing PD, and both could serve as optimal screening tools for sarcopenia in clinical settings.
References
- Rosenberg, I.H. Sarcopenia: Origins and clinical relevance. J Nutr 1997, 127, 990S-991S.
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.P.; Rolland, Y.; Schneider, S.M., et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010, 39, 412-423.
- Chen, L.-K.; Liu, L.-K.; Woo, J.; Assantachai, P.; Auyeung, T.-W.; Bahyah, K.S.; Chou, M.-Y.; Chen, L.-Y.; Hsu, P.-S.; Krairit, O. Sarcopenia in Asia: Consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc 2014, 15, 95-101.
- Fahal, I.H. Uraemic sarcopenia: Aetiology and implications. Nephrol Dial Transplant 2014, 29, 1655-1665.
- Blumenkrantz, M.J.; Gahl, G.M.; Kopple, J.D.; Kamdar, A.V.; Jones, M.R.; Kessel, M.; Coburn, J.W. Protein losses during peritoneal dialysis. Kidney Int 1981, 19, 593-602.
- Malmstrom, T.K.; Morley, J.E. Sarc-f: A simple questionnaire to rapidly diagnose sarcopenia. J Am Med Dir Assoc 2013, 14, 531-532.
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyere, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A., et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16-31.
- Chen, L.K.; Woo, J.; Assantachai, P.; Auyeung, T.W.; Chou, M.Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S., et al. Asian working group for sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc 2020, 21, 300-307 e302.
- Kawakami, R.; Murakami, H.; Sanada, K.; Tanaka, N.; Sawada, S.S.; Tabata, I.; Higuchi, M.; Miyachi, M. Calf circumference as a surrogate marker of muscle mass for diagnosing sarcopenia in Japanese men and women. Geriatr Gerontol Int 2015, 15, 969-976.
- Kim, S.; Kim, M.; Lee, Y.; Kim, B.; Yoon, T.Y.; Won, C.W. Calf circumference as a simple screening marker for diagnosing sarcopenia in older korean adults: The Korean frailty and aging cohort study (KFACS). J Korean Med Sci 2018, 33.
- Chen, C.Y.; Tseng, W.C.; Yang, Y.H.; Chen, C.L.; Lin, L.L.; Chen, F.P.; Wong, A.M.K. Calf circumference as an optimal choice of four screening tools for sarcopenia among ethnic Chinese older adults in assisted living. Clin Interv Aging 2020, 15, 2415-2422.
- Barbosa-Silva, T.G.; Menezes, A.M.; Bielemann, R.M.; Malmstrom, T.K.; Gonzalez, M.C. Enhancing SARC-F: Improving sarcopenia screening in the clinical practice. J Am Med Dir Assoc 2016, 17, 1136-1141.
- Fu, X.; Tian, Z.; Thapa, S.; Sun, H.; Wen, S.; Xiong, H.; Yu, S. Comparing SARC-F with SARC-CalF for screening sarcopenia in advanced cancer patients. Clin Nutr 2020, 39, 3337-3345.
- Bahat, G.; Oren, M.M.; Yilmaz, O.; Kılıç, C.; Aydin, K.; Karan, M.A. Comparing SARC-F with SARC-CalF to screen sarcopenia in community living older adults. J Nutr Health Aging 2018, 22, 1034-1038.
- Yang, M.; Hu, X.; Xie, L.; Zhang, L.; Zhou, J.; Lin, J.; Wang, Y.; Li, Y.; Han, Z.; Zhang, D., et al. Screening sarcopenia in community-dwelling older adults: SARC-F vs SARC-F combined with calf circumference (SARC-CalF). J Am Med Dir Assoc 2018, 19, 277.e271-277.e278.
- Do, J.Y.; Seo, J.H.; Kang, S.H. Validation of the SARC-F for assessing sarcopenia in patients on peritoneal dialysis. J Ren Nutr 2021, 21, S1051-2276.
- Studenski, S.A.; Peters, K.W.; Alley, D.E.; Cawthon, P.M.; McLean, R.R.; Harris, T.B.; Ferrucci, L.; Guralnik, J.M.; Fragala, M.S.; Kenny, A.M., et al. The FNIH sarcopenia project: Rationale, study description, conference recommendations, and final es-timates. J Gerontol A Biol Sci Med Sci 2014, 69, 547-558.
- Fielding, R.A.; Vellas, B.; Evans, W.J.; Bhasin, S.; Morley, J.E.; Newman, A.B.; Abellan van Kan, G.; Andrieu, S.; Bauer, J.; Breuille, D., et al. Sarcopenia: An undiagnosed condition in older adults. Current consensus definition: Prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc 2011, 12, 249-256.
- Yamamoto, S.; Matsuzawa, R.; Harada, M.; Watanabe, T.; Shimoda, T.; Suzuki, Y.; Kamiya, K.; Osada, S.; Yoshida, A.; Matsunaga, A. SARC-F questionnaire: Rapid and easy tool for identifying physical limitations in hemodialysis patients. JCSM Clinical Reports 2019, 4, 1-12.
- Lin, Y.L.; Hou, J.S.; Lai, Y.H.; Wang, C.H.; Kuo, C.H.; Liou, H.H.; Hsu, B.G. Association of SARC-F questionnaire and mor-tality in prevalent hemodialysis patients. Diagnostics (Basel, Switzerland) 2020, 10, 890.
- Kera, T.; Kawai, H.; Hirano, H.; Kojima, M.; Watanabe, Y.; Motokawa, K.; Fujiwara, Y.; Osuka, Y.; Kojima, N.; Kim, H., et al. Limitations of SARC-F in the diagnosis of sarcopenia in community-dwelling older adults. Arch Gerontol Geriatr 2020, 87, 103959.
- Marini, A.; Perez, D.; Fleuri, J.; Pimentel, G. SARC-F is better correlated with muscle function indicators than muscle mass in older hemodialysis patients. J Nutr Health Aging 2020, 24, 999-1002.
- Gonzalez, M.C.; Mehrnezhad, A.; Razaviarab, N.; Barbosa-Silva, T.G.; Heymsfield, S.B. Calf circumference: Cutoff values from the NHANES 1999–2006. Am J Clin Nutr 2021, 113, 1679-1687.
- Mo, Y.H.; Zhong, J.; Dong, X.; Su, Y.D.; Deng, W.Y.; Yao, X.M.; Liu, B.B.; Wang, X.Q.; Wang, X.H. Comparison of three screening methods for sarcopenia in community-dwelling older persons. J Am Med Dir Assoc 2021, 22, 746-750 e741.
- Nishikawa, H.; Yoh, K.; Enomoto, H.; Iwata, Y.; Sakai, Y.; Kishino, K.; Shimono, Y.; Ikeda, N.; Takashima, T.; Aizawa, N., et al. Calf circumference as a useful predictor of sarcopenia in patients with liver diseases. In Vivo 2020, 34, 2561-2569.
- Inoue, T.; Maeda, K.; Shimizu, A.; Nagano, A.; Ueshima, J.; Sato, K.; Murotani, K. Calf circumference value for sarcopenia screening among older adults with stroke. Arch Gerontol Geriatr 2021, 93, 104290.
