The thyroid gland is a richly vascularized endocrine gland. It is an uneven organ located in a median position in the antero-lower region of the neck, between the fifth cervical vertebra and the first thoracic vertebra.
1. Introduction
The
thyroi
d gland is a richly vascularized endocrine gland [1]. It is an uneven organ located in a m
edian po
rtancesition in the antero-lower region of the neck, between the fifth cervical vertebra and the first thoracic vertebra.The importance of studying the vascularization of the thyroid gland and its variation is mainly due to its close relationship with other structures, especially muscle and vascular nerve bundles.
Topographically, the medial face of the thyroid gland is placed directly on the ventral surface of the larynx and the trachea, while the ventral surface of the gland, starting from the anterior and medial face of the organ, is covered by the subhyoid muscles (such as the sternothyroid, homohyoid and sternohyoid muscle) that are enclosed by the splitting of the middle cervical fascia.
Laterally, in correspondence of the lobes, there are the sternocleidomastoid muscle and, more superficially, the superficial cervical fascia and the platysma. Furthermore, the lateral surface of the two lobes is related to the vascular nerve bundle of the neck, covered by the carotid sheath holding the common carotid artery, the internal jugular vein, and the vagus nerve. Moreover, medially, between the thyroid gland sheath and the oesophagus–tracheal corner, it is worth noticing the recurrent laryngeal nerve, closest to the left lobe.
Concerning the thyroid isthmus, it is superficially covered by the sternohyoid muscle and, laterally, by the anterior jugular veins.
Finally, between the peri-thyroid sheath and the capsule that adheres to the parenchyma, the so-called “dangerous space” must remain intact when the gland is removed in order to avoid severe bleeding, since it holds the rich thyroid venous network.
For what may concern the blood supply, it is achieved through two superior thyroid arteries (STA), two inferior thyroid arteries (ITA), and sometimes by an additional artery, the thyroid ima artery (TIMA) that reaches the gland from below at the isthmus level.
By-the-book, the STA takes origin as first branch from the external carotid artery (ECA), at the height of a horizontal plane passing through the hyoid bone. Concerning its origin, it is behind the sternocleidomastoid muscle and it is in relationship, medially, with the inferior pharyngeal constrictor muscle, the larynx, and with the superior laryngeal nerve. Furthermore, different branches such as the infrahyoid, sternocleidomastoid, superior laryngeal, and cricothyroid artery originate from the STA.
On the other hand, the ITA originates as terminal artery from the thyrocervical trunk (TCT) that arises, as a short and wide artery, from the front of the first part of the subclavian artery (SA). The relationship between the ITA and the recurrent laryngeal nerve is extremely important since the ITA usually passes behind the nerve. However, closest to the thyroid gland, the right nerve is equally likely to be anterior, posterior or amongst, and the left nerve is usually posterior. Furthermore, on the left side, near its origin, the artery is crossed anteriorly by the thoracic duct as the latter curves infero-laterally to its termination. Furthermore, collateral branches arise from the ITA: the ascending cervical and the inferior laryngeal artery, and the oesophageal, pharyngeal and tracheal branches
[1][2][2,3].
However, part of the scientific literature tends to deny this “classic” origin and shows numerous anatomical variants.
2. The Origin of the Superior Thyroid Artery (STA)
One of the first variants characterizing the STA is its origin.
Table 1. Available data concerning STA origin.
5][6][7][8][9][10][11][12][13][20,25,35,36,37,38,39,40,41,42].
Table 5. Available data concerning the ITA origin.
| Author(s) |
Type of Study |
Number of Cases |
TCT Right |
TCT Left |
SA Right |
SA Left |
VA |
CCA Right |
CCA Left |
SSA |
| (Esen et al., 2018) |
TC angiography |
640 |
95 |
90.3 |
2.8 |
2 |
0.6 |
- |
- |
- |
| (Roshan et al., 2015) |
Cadavers |
100 * |
96 |
100 |
4 |
- |
|
- |
- |
- |
| (Hölbling Patscheider et al., 2011) |
Cadaver
(clinical case report) |
1 |
- |
100 |
100 |
- |
- |
- |
- |
- |
| (Ngo Nyeki et al., 2016) |
Surgery
(clinical case report) |
1 |
- |
100 |
- |
- |
- |
100 |
- |
- |
| (Mariolis-Sapsakos et al., 2014) |
Surgery
(clinical case report) |
1 |
- |
- |
- |
- |
- |
100 |
100 |
- |
| (Simmons et al., 1987) |
Surgery
(clinical case report) |
1 |
|
- |
- |
100 |
- |
100 |
- |
- |
| (Sherman and Colborn, 2003) |
Cadaver
(clinical case report) |
1 |
100 |
- |
- |
- |
- |
- |
- |
- |
| (Cigali et al., 2008) |
Cadaver
(clinical case report) |
1 |
- |
100 |
- |
- |
- |
- |
- |
100 (left, accessory) |
| (Lovasova et al., 2017) |
Cadaver
(clinical case report) |
1 |
100 |
- |
- |
- |
- |
100 |
- |
- |
| (González-Castillo et al., 2018) |
Cadaver
(clinical case report) |
1 |
- |
100 |
- |
- |
- |
- |
- |
- |
| Author(s) |
Type of Study |
Number of Cases |
ECA (%) |
CB (%) |
CCA (%) |
| (Lučev et al., 2000) |
Cadavers |
40 |
30 |
22.5 |
47.5 |
| (Ozgur et al., 2008) |
Cadavers |
40 * |
25 |
40 |
35 |
| (Vázquez et al., 2009) |
Cadavers |
207 * |
23 |
49 |
26.6 |
| (Natsis et al., 2011) |
Cadavers |
100 |
39 |
49 |
12 |
| (Anagnostopoulou and Mavridis, 2014) |
Cadavers |
68 |
23.5 |
4.4 |
17.6 |
| (Sanjeev et al., 2010) |
Cadavers |
37 |
64.86 |
- |
35.14 |
| (Ozgur et al., 2009) |
Cadavers |
40 * |
25 |
40 |
35 |
| (Gupta et al., 2014) |
Angiography |
25 |
72 |
20 |
8 |
| (Won et al., 2011) |
Cadaver (clinical case report) |
1 |
- |
- |
100 |
| (Ongeti and Ogeng’o, 2012) |
Cadavers |
46 |
80.4 |
2.2 |
10.9 |
| (Zümre et al., 2005) |
Cadavers |
40 * |
25 |
70 |
5 |
| (Troupis et al., 2014) |
Cadaver (clinical case report) |
1 |
- |
100 (right) |
100 (left) |
| (Nochikattil, 2017) |
Surgery (clinical case report) |
1 |
- |
- |
100 |
| (Motwani and Jhajhria, 2015) |
Cadaver (clinical case report) |
1 |
100 |
- |
- |
| (Lemaire et al., 2001) |
Cadaver (clinical case report) |
1 |
- |
- |
100 |
| (Jadhav et al., 2011) |
Cadaver (clinical case report) |
1 |
- |
100 right |
- |
| (Esen et al., 2018) |
TC angiography |
640 |
64.5 (right) and 39.7 (left) |
20.5 (right) and 23.1 (left) |
14.1 (right) and 35.3 (left) |
| (Issing et al., 1994) |
Surgery (clinical case report) |
1 |
- |
- |
100 |
| (Mehta et al., 2010) |
Cadaver (clinical case report) |
1 |
- |
- |
100 (right) |
| (Dhindsa and Sodhi, 2014) |
Cadaver (clinical case report) |
1 |
100 (right) |
- |
100 (left) |
| (Fujimoto et al., 1974) |
Cadaver (clinical case report) |
1 |
- |
- |
100 |
| (Lovasova et al., 2017) |
Cadaver (clinical case report) |
1 |
100 |
- |
- |
| (Sreedharan et al., 2018) |
Cadavers |
60 * |
88.33 |
8.33 |
3.33 |
| (Hayashi et al., 2019) |
Surgery (clinical case report) |
1 |
100 |
- |
|
The results are reported as percentage (%) of cases for different type of study. Asterisk (*) means that the analysis was conducted on heminecks. ECA: origin from the external carotid artery; CB: origin from the carotid bifurcation; CCA: origin from the common carotid artery.
3. STA Common Trunk (Lingual and Facial Arteries)
Table 3. Available data concerning the STA origin from thyrolingual and thyrolinguofacial trunk.
| Author(s) |
Type of Study |
Number of Cases |
Thyrolingualtrunk (%) |
Thyrolinguofacialtrunk (%) |
| (Ozgur et al., 2008) |
Cadavers |
40 * |
2.5 |
- |
| (Vázquez et al., 2009) |
Cadavers |
330 * |
0.9 |
0.3 |
| (Natsis et al., 2011) |
Cadavers |
100 |
3 |
- |
| (Kapre et al., 2013) |
Cadavers |
21 |
9.5 |
- |
| (Anagnostopoulou and Mavridis, 2014) |
Cadavers |
68 |
14.7 |
12.3 |
| (Sanjeev et al., 2010) |
Cadavers |
37 |
2.7 |
- |
| (Ozgur et al., 2009) |
Cadavers |
40 |
2.5 |
- |
| (Ongeti and Ogeng’o, 2012) |
Cadavers |
46 |
6.5 |
- |
| (Zümre et al., 2005) |
Cadavers |
40 * |
2.5 |
2.5 |
| (Nochikattil, 2017) |
Surgery (clinical case report) |
1 |
100 |
- |
| (Lemaire et al., 2001) |
Cadaver (clinical case report) |
1 |
100 |
- |
| (Jadhav et al., 2011) |
Cadaver (clinical case report) |
1 |
100 |
- |
The results are reported as percentage (%) of cases for different type of study. Asterisk (*) means that the analysis was conducted on heminecks.
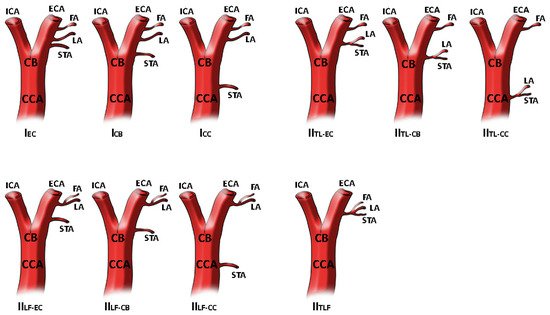
Figure 1. STA different origin as reported and modified by Natsis and colleagues. In type I STA origins as separate branch at different levels. In type II STA is a part of thyrolingual trunk or thyrolinguofacial trunk. The image has been modified as previously reported
[3][7]. Superior thyroid artery origin classification. Type I, separate branches, I
EC: STA as separate branch from ECA, I
CB: STA as separate branch from CB, I
CC: STA as separate branch from CCA. Type II
TL branching patterns, II
TL-EC: thyrolingual trunk from ECA, II
TL-CB: thyrolingual trunk from CB,
IITL-CC: thyrolingual trunk from CCA. Type II
LF branching patterns, II
LF-EC: linguofacial trunk and STA from ECA, II
LF-CB: linguofacial trunk from ECA and STA at the level of CB, II
LF-CC: linguofacial trunk from ECA and STA from CCA. Type II
TLF branching pattern, thyrolinguofacial trunk from ECA.
4. Inferior Thyroid Artery (ITA)
Regarding the ITA, and referring to the existing literature, there are more examples of anatomical variants than the STA, discovered by non-invasive techniques, cadaver dissection or during surgical intervention. The knowledge of the ITA’s anatomical variants is essential for its relationship with the laryngeal nerve: it may be absent, present as an ancillary (accessory) ITA, and appearing double or originate at different levels
[4][20], and as reported in the studies described in
Table 5, even if the most common origin of the ITA is the thyrocervical trunk (TCT), it can also originate from other vessels such as the CCA, the subclavian artery (SA), the vertebral artery (VA) or the suprascapular artery (SSA)
[4][
The results are reported as percentage (%) of cases for different type of study. Asterisk (*) means that the analysis was conducted on heminecks. TCT: origin from thyrocervical trunk (right or left); SA: origin from subclavian artery (right or left); VA: origin from vertebral artery; CCA: origin from common carotid artery (right or left); SSA; origin from suprascapular artery.
4. Thyroid Ima Artery (TIMA)
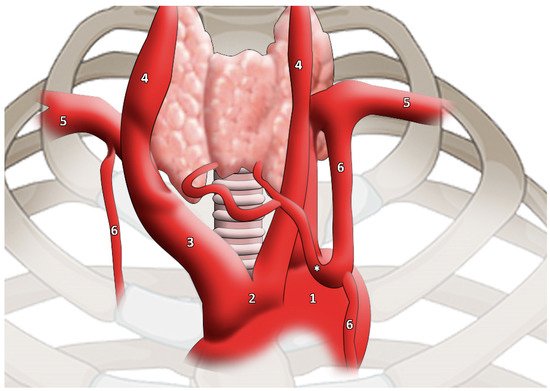
The main branch went to the lower edge of the thyroid gland, subsequently dividing into two branches to supply the gland itself. The artery that compensates for the lack of normal thyroid vessels is called the TIMA, and it should not be considered as an accessory thyroid artery (
Figure 2).
Figure 2. TIMA (highlighted by * asterisk) as reported and modified by Moriggl and colleagues. It is worth noticing the artery calibre
[14][46]. 1, aortic arch; 2, common origin of innominate artery and left common carotid artery; 3, innominate artery; 4, common carotid artery; 5, subclavian artery; 6, internal thoracic artery.