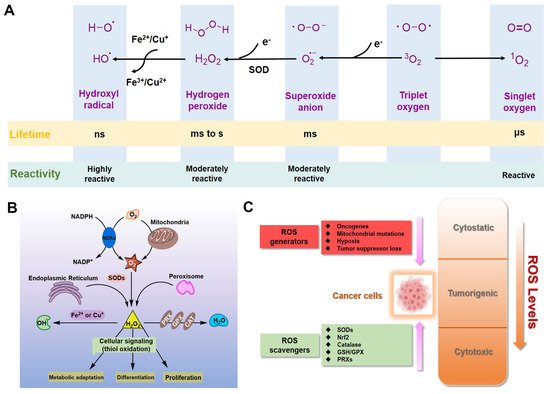
For eukaryotic cells, reactive oxygen species (ROS) encompass a group of molecules derived from oxygen. Due to the well-established role of ROS in cell signaling, cancer cells always have higher levels of endogenous ROS to enhance rapid cell growth and proliferation through the mitogen-activated protein kinase (MAPK)/extracellular-regulated kinase 1/2 (ERK1/2), phosphoinositide-3-kinase (PI3K)/Akt, nuclear factor-κB (NF-κB), and hypoxia-sensitive α (HIF1α) pathways. Evaluated ROS have frequently been observed in various cancers, which activate multiple pro-tumourigenic signaling, and induce survival and proliferation of cancer cells. Hydrogen peroxide and superoxide anion are the most important redox signaling agents in cancer cells, whose homeostasis is maintained by dozens of growth factors, cytokines and antioxidant enzymes. Therefore, antioxidant enzymes, especially Cu/Zn superoxide dismutase (SOD1), tend to have higher activities to maintain the homeostasis of ROS in cancer cells. We can inhibit the activity of SOD1 using copper chelators to kill cancer cells.
- anti-cancer
- reactive oxygen species
- chelators
- metal complexes
- antioxidant enzymes
- SOD1
- TrxR
- mitochondria
- inhibitors
1. Introduction
2. Inorganic SOD1 Inhibitors with Anti-Cancer Prospects
In mammals, the main biological function of SODs is to catalyze the dismutation of O2•− into H2O2 and O2 [39,40]. Cu/Zn superoxide dismutase (SOD1), the major SOD, mainly exists in the formation of homodimers in cells and is widely distributed in the nucleus, the cytoplasm, and the intermembrane space (IMS) of mitochondria [41]. Next, Mn superoxide dismutase (SOD2) exclusively exists in the mitochondrial matrix [42]. An extracellular form of SOD (EC-SOD), also a Cu/Zn-containing SOD, is tetrameric and exists in most mammals [42]. Besides this, SOD1 also regulates multiple redox signals to control growth and metabolic pathways, such as glucose metabolism and transcription [5,43,44,45]. Therefore, SODs, especially SOD1, are the first firewall to resist oxidative stress. Recently, emerging evidence from researchers has indicated that SOD1 is usually overexpressed in cancer cells; its activity is essential to maintain higher ROS levels under the critical threshold during aberrant energy metabolism of cancer progression [41]. For example, SOD1 accumulations were observed not only in the cytoplasm but also in the nucleus of human primary breast and mammary cancers [46]. Besides this, prostate cancer cells (DU145) also have higher levels of activity and expression of SOD1, compared with normal prostate cells (RWPE-1) [5]. In vitro studies also showed that the fast growth of non-small cell lung cancer (NSCLC) and leukemia depends on the high activity of SOD1, which controls the oncogenic KRAS and EGFR pathways [47,48], as well as other cancer cells and xenograft tumors [49]. In general, SOD1 is recognized as a promising anti-cancer target, and several small-molecule targeting drugs for SOD1 have already entered the preclinical and clinical development stages [50]. Since the activity of SOD1 mainly comes from the copper ion in the active center, a vast majority of SOD1 inhibitors are competitive chelators of copper ions. In 1975, Heikkila et al. found that diethyldithiocarbamate (DDC) can competitively bind to copper ions (Figure 2), thereby inhibiting SOD1 activity at a millimolar level [51]. After being inhibited by DDC, SOD1 cannot restore enzyme activity through dialysis, but adding CuSO4 during dialysis restores SOD1 activity [51]. In 1979, Misra systematically explored the mechanism by which DDC inhibits SOD1 activity [52]. In Phase I, one DDC molecule first coordinates with the copper(II) center in SOD1, with retention of activity. In Phase II, a second DDC displaces the copper(II) center, with a loss of activity. The shortcomings of DDC as a SOD1 inhibitor are mainly reflected in its high working concentration and poor specificity, such as its interference with the activity of cytochrome c oxidase [53,54]. Nevertheless, DDC still has a wide range of anti-cancer applications, and DDC effectively inhibits SOD1 activity to kill cancer cells [55,56,57].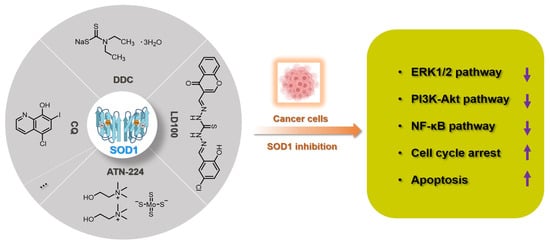
3. Prespective
SOD1 is indeed a recognized target for cancer treatment. At present, a variety of chelators have been used for SOD1 inhibition. LD100 may be the most effective inhibitor designed through coordination chemistry. However, the use of inorganic strategies to develop anti-cancer drugs based on SOD1 inhibition still requires further efforts. First, we need to solve the problem of compatibility between targeted and clinical deliveries. On the other hand, we also should reduce the side effects of chelating agents while ensuring the efficiency of SOD1 inhibition. The summary of SOD1 metal-chelating inhibition can provide a reference for the design of SOD1 inhibitors with anti-cancer effects in the future.4. References
- Waszczak, C.; Carmody, M.; Kangasjärvi, J. Reactive oxygen species in plant signaling. Rev. Plant Biol. 2018, 69, 209-236.
- Weinberg, F.; Ramnath, N.; Nagrath, D. Reactive oxygen species in the tumor microenvironment: an overview. Cancers 2019, 11, 1191.
- Yang, B.; Chen, Y.; Shi, J. Reactive oxygen species (ROS)-based nanomedicine. Rev. 2019, 119, 4881-4985.
- Marcec, M.J.; Gilroy, S.; Poovaiah, B.W.; Tanaka, K. Mutual interplay of Ca2+ and ROS signaling in plant immune response. Plant Sci. 2019, 283, 343-354.
- Li, X.; Chen, Y.; Zhao, J.; Shi, J.; Wang, M.; Qiu, S.; Hu, Y.; Xu, Y; Cui, Y.; Liu, C.; Liu, The specific inhibition of SOD1 selectively promotes apoptosis of cancer cells via regulation of the ROS signaling network. Oxid. Med. Cell. Longev. 2019.
- Schieber, M.; Chandel, N.S. ROS function in redox signaling and oxidative stress. Biol. 2014, 24, R453-R462.
- Milkovic, L.; Cipak Gasparovic, A.; Cindric, M.; Mouthuy, P.A.; Zarkovic, N. Short overview of ROS as cell function regulators and their implications in therapy concepts. Cells 2019, 8, 793-807.
- Sies, H.; Jones, D.P. Reactive oxygen species (ROS) as pleiotropic physiological signalling agents. Rev. Mol. Cell Bio. 2020, 21, 363-383.
- D'Autréaux, B.; Toledano, M.B. ROS as signalling molecules: mechanisms that generate specificity in ROS homeostasis. Rev. Mol. Cell Bio. 2007, 8, 813-824.
- Reczek, C.R.; Chandel. N.S. ROS-dependent signal transduction. Opin. Cell Biol. 2015, 33, 8-13.
- Moloney, J.N.; Cotter, T.G. ROS signalling in the biology of cancer. Cell Dev. Biol. 2018, 80, 50-64.
- Wang, Y.; Branicky, R.; Noë, A.; Hekimi, S. Superoxide dismutases: Dual roles in controlling ROS damage and regulating ROS signaling. Cell Biol. 2018, 217, 1915-1928.
- Su, X.; Shen, Z.; Yang, Q.; Sui, F.; Pu, J.; Ma, J.; Ma, S.; Yao, D.; Ji, M.; Hou. P. Vitamin C kills thyroid cancer cells through ROS-dependent inhibition of MAPK/ERK and PI3K/AKT pathways via distinct mechanisms. Theranostics 2019, 9,
- Li, Y.; Liang, R.; Zhang, X.; Wang, J.; Shan, C.; Liu, S.; Li, L.; Zhang, S. Copper chaperone for superoxide dismutase promotes breast cancer cell proliferation and migration via ROS-mediated MAPK/ERK signaling. Pharmacol. 2019, 10, 356-367.
- Steelman, L.S.; Abrams, S.L.; Whelan, J.; Bertrand, F.E.; Ludwig, D.E.; Bäsecke, J.; Libra, M.; Stivala, F.; Milella, M.; Tafuri, A.; Lunghi, P.; Bonati, A.; Martelli, A.M. McCubrey, J.A. Contributions of the Raf/MEK/ERK, PI3K/PTEN/Akt/mTOR and Jak/STAT pathways to leukemia. Leukemia 2008, 22, 686-707.
- Yeo, D.; Hwang, S.J.; Kim, W.J.; Youn, H.J.; Lee. H.J. The aqueous extract from Artemisia capillaris inhibits acute gastric mucosal injury by inhibition of ROS and NF-kB. Pharmacother. 2018, 99, 681-687.
- Park, S.A.; Na, H. K.; Kim, E.H.; Cha, Y.N.; Surh, Y.J. 4-Hydroxyestradiol induces anchorage-independent growth of human mammary epithelial cells via activation of IκB kinase: Potential role of reactive oxygen species. Cancer Res. 2009, 69, 2416-2424.
- Castelli, S.; Ciccarone, F.; Tavian, D.; Ciriolo, M.R. ROS-dependent HIF1α activation under forced lipid catabolism entails glycolysis and mitophagy as mediators of higher proliferation rate in cervical cancer cells. Exp. Clin. Canc Res. 2021, 40, 1-18.
- Szatrowski, T.P.; Nathan, C.F. Production of large amounts of hydrogen peroxide by human tumor cells. Cancer Res. 1991, 51, 794-798.
- Perillo, B.; Di Donato, M.; Pezone, A.; Di Zazzo, E.; Giovannelli, P.; Galasso, G.; Castoria, G.; Migliaccio, A. ROS in cancer therapy: The bright side of the moon. Mol. Med. 2020, 52, 192-203.
- Hu, Y.; Rosen, D.G.; Zhou, Y.; Feng, L.; Yang, G.; Liu, J. Huang, P. Mitochondrial manganese-superoxide dismutase expression in ovarian cancer: role in cell proliferation and response to oxidative stress. Biol. Chem. 2005, 280, 39485-39492.
- Saydam, N.; Kirb, A.; Demir, Ö.; Hazan, E.; Oto, Ö.; Saydam, O.; Güner, G. Determination of glutathione, glutathione reductase, glutathione peroxidase and glutathione S-transferase levels in human lung cancer tissues. Cancer Lett. 1997, 119, 13-19.
- Murawaki, Y.; Tsuchiya, H.; Kanbe, T.; Harada, K.; Yashima, K.; Nozaka, K.; Tanida, O.; Kohno, M.; Mukoyama, T.; Nishimuki, E.; Kojo, H.; Matsura, T.; Takahashi, K.; Osaki, M.; Ito, H.; Yodoi, J.; Murawaki, Y. Shiota, G. Aberrant expression of selenoproteins in the progression of colorectal cancer. Cancer Lett. 2008, 259, 218-230.
- Oberley, T.D.; Oberley, L.W. Antioxidant enzyme levels in cancer. Histopathol. 1997, 12, 525–535.
- De Sá Junior, P. L.; Câmara, D.A.D.; Porcacchia, A.S.; Fonseca, P. M. M.; Jorge, S.D.; Araldi, R.P.; Ferreira, A.K. The roles of ROS in cancer heterogeneity and therapy. Med. Cell. Longev. 2017.
- Chio, I.I.C.; Tuveson D.A. ROS in cancer: the burning question. Trends Mol. Med. 2017, 23, 411-429.
- Zehra, S.; Cirilli, I.; Silvestri, S.; Gómez-Ruiz, S.; Tabassum, S.; Arjmand, F. Structure elucidation, in vitro binding studies and ROS-dependent anti-cancer activity of Cu (II) and Zn (II) phthaloylglycinate (phen) complexes against MDA-MB-231 cells. Metallomics 2021, 13, mfab064.
- Guo, W.; Ye, S.; Cao, N.; Huang, J.; Gao, J.; Chen, Q. ROS-mediated autophagy was involved in cancer cell death induced by novel copper (II) complex. Toxicol Pathol. 2010, 62, 577-582.
- Liu, J.; Guo, W.; Li, J.; Li, X.; Geng, J.; Chen, Q.; Gao, J. Tumor-targeting novel manganese complex induces ROS-mediated apoptotic and autophagic cancer cell death. J. mol. med. 2015, 35, 607-616.
- Marloye, M.; Berger, G.; Gelbcke, M.; Dufrasne, F. A survey of the mechanisms of action of anticancer transition metal complexes. Future Med. Chem. 2016, 8, 2263-2286.
- Sîrbu, A.; Palamarciuc, O.; Babak, M.V.; Lim, J.; Ohui, K.; Enyedy, E.A.; Shova, S.; Darvasiová, D.; Rapta, P.; Ang, W.H.; Arion, V.B. Copper (II) thiosemicarbazone complexes induce marked ROS accumulation and promote nrf2-mediated antioxidant response in highly resistant breast cancer cells. Dalton Trans. 2017, 46, 3833-3847.
- Donate, F.; Juarez, J.C.; Burnett, M.E.; Manuia, M.M.; Guan, X.; Shaw, D.E.; Smith, E.L.P.; Timucin, C.; Braunstein, M.J.; Batuman, O.A. Mazar, A. P. Identification of biomarkers for the antiangiogenic and antitumour activity of the superoxide dismutase 1 (SOD1) inhibitor tetrathiomolybdate (ATN-224). J. cancer. 2008, 98, 776-783.
- Dong, X.; Zhang, Z.; Zhao, J.; Lei, J.; Chen, Y.; Li, X.; Chen, H.; Tian, J.; Zhang, D.; Liu, C.; Liu, C. The rational design of specific SOD1 inhibitors via copper coordination and their application in ROS signaling research. Sci. 2016, 7, 6251-6262.
- Kalaivani, P.; Saranya, S.; Poornima, P.; Prabhakaran, R.; Dallemer, F.; Padma, V. V.; Natarajan, K. Biological evaluation of new nickel (II) metallates: Synthesis, DNA/protein binding and mitochondrial mediated apoptosis in human lung cancer cells (A549) via ROS hypergeneration and depletion of cellular antioxidant pool. J. Med. Chem. 2014. 82, 584-599.
- Zhang, P.; Sadler, P.J. Redox-active metal complexes for anticancer therapy. J. Inorg. Chem. 2017, 2017, 1541-1548.
- Imberti, C.; Zhang, P.; Huang, H.; Sadler, P.J. New designs for phototherapeutic transition metal complexes. Chem. Int. Ed. 2020, 59, 61-73.
- Luo, Z.; Yu, L.; Yang, F.; Zhao, Z.; Yu, B.; Lai, H.; Wong, K.; Ngai, S.M.; Zheng, W.; Chen, T. Ruthenium polypyridyl complexes as inducer of ROS-mediated apoptosis in cancer cells by targeting thioredoxin reductase. Metallomics 2014, 6, 1480-1490.
- Ng, C.H.; Kong, S.M.; Tiong, Y.L.; Maah, M.J.; Sukram, N.; Ahmad, M.; Khoo, A.S.B. Selective anticancer copper (II)-mixed ligand complexes: targeting of ROS and proteasomes. Metallomics 2014, 6, 892-906.
- Borgstahl, G.E.O, Oberley-Deegan, R.E. Superoxide dismutases (SODs) and SOD mimetics. Antioxidants 2018, 7, 156-158.
- Robinett, N.G.; Peterson, R.L.; Culotta, V.C. Eukaryotic copper-only superoxide dismutases (SODs): A new class of SOD enzymes and SOD-like protein domains. Biol. Chem. 2018, 293, 4636-4643.
- Papa, L.; Manfredi, G.; Germain, D. SOD1, an unexpected novel target for cancer therapy. Genes & Cancer, 2014, 5, 15-21.
- Wang, X.; Zhang, H.; Sapio, R.; Yang, J.; Wong, J.; Zhang, X.; Guo, J.Y.; Pine, S. Remmen, H. V. Li, H. White, E.; Liu, C.; Kiledjian, M.; Pestov, D.G.; Zheng, X.F.S. SOD1 regulates ribosome biogenesis in KRAS mutant non-small cell lung cancer. commun. 2021, 12, 1-15.
- Tsang, C.K.; Liu, Y.; Thomas, J.; Zhang, Y.; Zheng, X.F.S. Superoxide dismutase 1 acts as a nuclear transcription factor to regulate oxidative stress resistance. Commun. 2014, 5, 1-11.
- Li, X.; Qiu, S.; Shi, J.; Wang, S.; Wang, M.; Xu, Y.; Nie, Z.; Liu, C.; Liu, C. A new function of copper zinc superoxide dismutase: as a regulatory DNA-binding protein in gene expression in response to intracellular hydrogen peroxide. Nucleic Acids Res. 2019, 10, 5074–5085.
- Reddi, A.R.; Culotta, V.C. SOD1 integrates signals from oxygen and glucose to repress respiration. Cell 2013, 152, 224-235.
- Papa, L.; Hahn, M.; Marsh, E.L.; Evans, B.S. Germain, D. SOD2 to SOD1 switch in breast cancer. Biol. Chem. 2014, 289, 5412-5416.
- Glasauer, A.; Sena, L.A.; Diebold, L.P.; Mazar, A.P. Chandel, N.S. Targeting SOD1 reduces experimental non–small-cell lung cancer. Clin. Invest. 2014, 124, 117-128.
- Somwar, R.; Erdjument-Bromage, H.; Larsson, E.; Shum, D.; Lockwood, W. W. Superoxide dismutase 1 (SOD1) is a target for a small molecule identified in a screen for inhibitors of the growth of lung adenocarcinoma cell lines. Natl. Acad. Sci. 2011, 108, 16375-16380.
- Gomez, M.L.; Shah, N.; Kenny, T.C.; Jenkins Jr, E.C.; Germain, D. SOD1 is essential for oncogene-driven mammary tumor formation but dispensable for normal development and proliferation. Oncogene 2019, 38, 5751-5765.
- Che, M.; Wang, R.; Li, X.; Wang, H.Y.; Zheng, X.F.S. Expanding roles of superoxide dismutases in cell regulation and cancer. Drug Discov. Today 2016, 21, 143-149.
- Heikkila, R.E.; Cabbat, F.S.; Cohen, G. In vivo inhibition of superoxide dismutase in mice by diethyldithiocarbamate. Biol. Chem. 1976, 251, 2182-2185.
- Misra, H.P. Reaction of copper-zinc superoxide dismutase with diethyldithiocarbamate. Biol. Chem. 1979, 254, 11623-11628.
- Singh, N.; Savanur, M.A.; Srivastava, S.; D'Silva, P.; Mugesh, G. A manganese oxide nanozyme prevents the oxidative damage of biomolecules without affecting the endogenous antioxidant system. Nanoscale, 2019, 11, 3855-3863.
- Griffiths, D.E.; Wharton, D.C. Studies of the electron transport system XXXV. Purification and properties of cytochrome oxidase. Biol. Chem. 1961, 236, 1850-1856.
- Skrott, Z.; Cvek, B. Diethyldithiocarbamate complex with copper: the mechanism of action in cancer cells. Mini Rev. Med. Chem. 2012, 12, 1184-1192.
- Feuser, P.E.; Cordeiro, A.P.; Silveira, G.B. Borges Corrêa, M. E. A.; Silveira, P.C. L.; Sayer, C.; Hermes de Araújo, P. H.; Machado-de-Ávila,R.A.; Dal Bó, A. G. Co-encapsulation of sodium diethyldithiocarbamate (DETC) and zinc phthalocyanine (ZnPc) in liposomes promotes increases phototoxic activity against (MDA-MB 231) human breast cancer cells. Surface. 2021, 197, 111434.
- Cho, H.Y.; Mavi, A.; Chueng, S.T.D.; Borges Corrêa, M.E.A.; Silveira, P.C.L.; Sayer, C.; Araújo, P.H.H.; Machado-de-Ávila, R.A.; Dal Bó, A.G. Tumor homing reactive oxygen species nanoparticle for enhanced cancer therapy. ACS Appl. Mater. Inter. 2019, 11, 23909-23918.
- Ding, W.Q.; Liu, B.; Vaught, J.L.; Yamauchi, H.; Lind, S.E. Anticancer activity of the antibiotic clioquinol. Cancer Res. 2005, 65, 3389-3395.
- Di Vaira, M.; Bazzicalupi, C.; Orioli, P.; Messori, L.; Bruni, B.; Zatta, P. Clioquinol, a drug for Alzheimer's disease specifically interfering with brain metal metabolism: structural characterization of its zinc (II) and copper (II) complexes. Chem. 2004, 43, 3795-3797.
- Katsuyama, M.; Kimura, E.; Ibi, M, Iwata, K.; Matsumoto, M.; Asaoka, N.; Yabe-Nishimura, C. Clioquinol inhibits dopamine-β-hydroxylase secretion and noradrenaline synthesis by affecting the redox status of ATOX1 and copper transport in human neuroblastoma SH-SY5Y cells. Toxicol. 2021, 95, 135-148.
- Brewer, G.J.; Dick, R.D.; Grover, D.K.; LeClaire, V.; Tseng, M.; Wicha, M.; Pienta, K.; Redman, B.G.; Jahan, T.; Sondak, V.K.; Strawderman, M.; LeCarpentier, G.; Merajver, S.D. Treatment of metastatic cancer with tetrathiomolybdate, an anticopper, antiangiogenic agent: Phase I study. Cancer Res. 2000, 6, 1-10.
- Juarez, J.C.; Manuia, M.; Burnett, M.E.; Betancourt, O.; Boivin, B.; Shaw, D. E.; Tonks, N. K.; Mazar, A. P.; Donate, F. Superoxide dismutase 1 (SOD1) is essential for H2O2-mediated oxidation and inactivation of phosphatases in growth factor signaling. Natl. Acad. Sci. 2008, 105, 7147-7152.
- Lin, J.; Zahurak, M.; Beer, T. M.; Ryan, C. J.; Wilding, G.; Mathew, P.; Morris, M.; Callahan, J.A.; Gordon, G.; Reich, S.D.; Carducci, M.A.; Antonarakis, E.S. A non-comparative randomized phase II study of 2 doses of ATN-224, a copper/zinc superoxide dismutase inhibitor, in patients with biochemically recurrent hormone-naïve prostate cancer. Oncol-Semin. Ori. 2013, 5, 581-588
- Juarez, J.C.; Betancourt, O.; Pirie-Shepherd, S.R.; Guan, X.; Price, M.L.; Shaw, D.E.; Mazar, A.P. Doñate, F. Copper binding by tetrathiomolybdate attenuates angiogenesis and tumor cell proliferation through the inhibition of superoxide dismutase. Cancer Res. 2006, 12, 4974-4982.
- Maiti, B.K.; Moura, J.J. Diverse biological roles of the tetrathiomolybdate anion. Chem. Rev. 2021, 429, 213635.
- Alvarez, H.M.; Xue, Y.; Robinson, C.D.; Canalizo-Hernandez, M. A.; Marvin, R. G.; Kelly, R.A.; Mondragon, A.; Penner-Hahn, J.E.; O'Halloran, T.V. Tetrathiomolybdate inhibits copper trafficking proteins through metal cluster formation. Science 2010, 327, 331-334.
